Abstract
Purpose
Limited data guide practice in evaluation and treatment of septic bursitis. We aimed to characterize clinical characteristics, microbiology, and outcomes of patients with septic bursitis stratified by bursal involvement, presence of trauma, and management type.
Methods
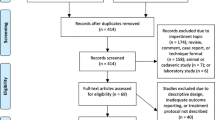
We conducted a retrospective cohort study of adult patients admitted to a single center from 1998 to 2015 with culture-proven olecranon and patellar septic bursitis. Baseline characteristics, clinical features, microbial profiles, operative interventions, hospitalization lengths, and 60-day readmission rates were determined. Patients were stratified by bursitis site, presence or absence of trauma, and operative or non-operative management.
Results
Of 44 cases of septic bursitis, patients with olecranon and patellar bursitis were similar with respect to age, male predominance, and frequency of bursal trauma; patients managed operatively were younger (p = 0.05). Clinical features at presentation and comorbidities were similar despite bursitis site, history of trauma, or management. The most common organism isolated from bursal fluid was Staphylococcus aureus. Patients managed operatively were discharged to rehabilitation less frequently (p = 0.04).
Conclusions
This study of septic bursitis is among the largest reported. We were unable to identify presenting clinical features that differentiated patients treated surgically from those treated conservatively. There was no clear relationship between preceding trauma or bursitis site and clinical course, management, or outcomes. Patients with bursitis treated surgically were younger. Additional study is needed to identify patients who would benefit from early surgical intervention for septic bursitis.




Similar content being viewed by others
References
Laupland KB, Davis HD. Olecranon septic bursitis managed in an ambulatory setting. The Calgary Home Parenteral Therapy Program Study Group. Clin Invest Med. 2001;24:171–8.
Martinez-Taboada VM, et al. Cloxacillin-based therapy in severe septic bursitis: retrospective study of 82 cases. Joint Bone Spine. 2009;76:665–9.
Perez C, et al. Infectious olecranon and patellar bursitis: short-course adjuvant antibiotic therapy is not a risk factor for recurrence in adult hospitalized patients. J Antimicrob Chemother. 2010;65:1008–14.
Hoffmeyer P, et al. Septic olecranon bursitis in a general hospital population. Can Med Assoc J. 1980;122:874–6.
Garcia-Porrua C, et al. The clinical spectrum of severe septic bursitis in Northwestern Spain: a 10 year study. J Rheumatol. 1999;26:663–7.
Ho G, et al. Septic bursitis in the prepatellar and olecranon bursae. An analysis of 25 cases. Ann Intern Med. 1978;89:21–7.
Sayegh ET, Strauch RJ. Treatment of olecranon bursitis: a systematic review. Arch Orthop Trauma Surg. 2014;134:1517–36.
Cea-Pereiro JC, et al. A comparison between septic bursitis caused by S. aureus and those caused by other organisms. Clin Rheumatol. 2001;20:10–4.
Stell IM. Management of acute bursitis: outcome study of a structured approach. J R Soc Med. 1999;92:516–21.
Canoso JJ, Sheckman PR. Septic subcutaneous bursitis. Report of sixteen cases. J Rheumatol. 1979;6:96–102.
Soderquist B, Hedstrom SA. Predisposing factors, bacteriology and antibiotic therapy in 35 cases of septic bursitis. Scand J Infect Dis. 1986;18:305–11.
Pien FD, et al. Septic bursitis: experience in a community practice. Orthopedics. 1991;14:981–4.
Gomez-Rodriguez N, et al. Infectious bursitis: study of 40 cases in the prepatellar and olecranon regions. Enferm Infecc Microbiol Clin. 1997;15:237–42.
Raddatz DA, et al. Septic bursitis: presentation, treatment, and prognosis. J Rheumatol. 1987;14:1160–3.
Zimmermann B, et al. Septic bursitis. Semin Arthritis Rheum. 1995;24:391–410.
De Angelis G, et al. Prosthetic joint infections in the elderly. Infection. 2015;43:629–37.
Osmon DR, et al. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013;56:e1–25.
Roschmann RA, Bell CL. Septic bursitis in immunocompromised patients. Am J Med. 1987;83:661–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Lieber, S.B., Fowler, M.L., Zhu, C. et al. Clinical characteristics and outcomes of septic bursitis. Infection 45, 781–786 (2017). https://doi.org/10.1007/s15010-017-1030-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-017-1030-3