Abstract
Background
To determine the rate of non-convulsive status epilepticus with/without prominent motor phenomena (SE-PM/ NCSE) and predictive value of electroclinical findings of continious electroencephalography (cEEG) monitoring of these patients and its association with prognosis in intensive care units (ICU).
Methods
We retrospectively collected data of 218 patients whose cEEG was performed in ICU between 2016 and 2018. The cEEG for NCSE diagnosis was evaluated according to Salzburg Consensus Criteria (SCC).
Results
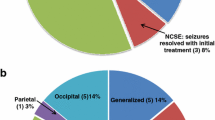
The mean age of patients was 57.09 ± 18.9 (16–95) years and 49.1% (107) were female. Of 218 patients, 32 (14.7%) had SE-PM/NCSE. According to SCC the rate of NCSE (NCSE + possible NCSE) was 9.6% (n = 21). Prior to cEEG recording, 38.9% (n = 85) of overall patients had a history of seizure/convulsion, and 22.7% (n = 21) of these patients diagnosed with NCSE based on cEEG. The mortality rates in critically ill patients were 41.3% (30.8%, 42.8%; for SE-PM and NCSE respectively). Prognosis was associated with age, epilepsy diagnosis, having convulsion/seizure history on follow-up, GCS, need for ventilation, kind of drugs, sepsis diagnosis, and minimum frequency of background activity of the cEEG (p = 0.001, 0.002, 0.001, 0.020, 0.001, 0.001, 0.001, 0.0001 respectively).
Conclusions
NCSE findings are mostly found in patients who were comatose and had seizure/convulsion history on follow-up. Mortality is higher in patients diagnosed with NCSE followed in the ICU compared to SE-PM.

Similar content being viewed by others
References
Fogang Y, Legros B, Depondt C, Mavroudakis N, Gaspard N (2017) Yield of repeated intermittent EEG for seizure detection in critically ill adults. Neurophysiol Clin/Clin Neurophysiol 47:5–12
Trinka E, Kälviäinen R (2017) 25 years of advances in the definition, classification and treatment of status epilepticus. Seizure 44:65–73
Leitinger M, Trinka E, Giovannini G, Zimmermann G, Florea C, Rohracher A, Kalss G, Neuray C, Kreidenhuber R, Höfler J (2019) Epidemiology of status epilepticus in adults: a population-based study on incidence, causes, and outcomes. Epilepsia 60:53–62
Towne A, Waterhouse E, Boggs J, Garnett L, Brown A, Smith J, DeLorenzo R (2000) Prevalence of nonconvulsive status epilepticus in comatose patients. Neurology 54:340–340
Kang BS, Jhang Y, Kim Y-S, Moon J, Shin J-W, Moon HJ, Lee S-T, Jung K-H, Chu K, Park K-I (2014) Etiology and prognosis of non-convulsive status epilepticus. J Clin Neurosci 21:1915–1919
DeLorenzo R, Hauser W, Towne A, Boggs J, Pellock J, Penberthy L, Garnett L, Fortner C, Ko D (1996) A prospective, population-based epidemiologic study of status epilepticus in Richmond, Virginia. Neurology 46:1029–1035
Power KN, Gramstad A, Gilhus NE, Engelsen BA (2015) Adult nonconvulsive status epilepticus in a clinical setting: semiology, aetiology, treatment and outcome. Seizure 24:102–106
Trinka E, Cock H, Hesdorffer D, Rossetti AO, Scheffer IE, Shinnar S, Shorvon S, Lowenstein DH (2015) A definition and classification of status epilepticus–report of the ILAE task force on classification of status epilepticus. Epilepsia 56:1515–1523
Herman ST, Abend NS, Bleck TP, Chapman KE, Drislane FW, Emerson RG, Gerard EE, Hahn CD, Husain AM, Kaplan PW (2015) Consensus statement on continuous EEG in critically ill adults and children, part I: indications. J Clin Neurophysiol Off Publ Am Electroencephalogr Soc 32:87
Claassen J, Taccone FS, Horn P, Holtkamp M, Stocchetti N, Oddo M (2013) Recommendations on the use of EEG monitoring in critically ill patients: consensus statement from the neurointensive care section of the ESICM. Intensive Care Med 39:1337–1351
Rubinos C, Godoy D (2020) Electroencephalographic monitoring in the critically ill patient: What useful information can it contribute? Med Intensiva (Engl Ed) 44:301–309
Leitinger M, Beniczky S, Rohracher A, Gardella E, Kalss G, Qerama E, Höfler J, Lindberg-Larsen AH, Kuchukhidze G, Dobesberger J (2015) Salzburg consensus criteria for non-convulsive status epilepticus–approach to clinical application. Epilepsy Behav 49:158–163
Fountain NB (2000) Status epilepticus: risk factors and complications. Epilepsia 41:S23–S30
Kaplan PW (2003) Prognosis in nonconvulsive status epilepticus. Prognosis of epilepsies. John Libbey Eurotext, Paris, pp 311–325
Young BG, Jordan KG, Doig GS (1996) An assessment of nonconvulsive seizures in the intensive care unit using continuous EEG monitoring: an investigation of variables associated with mortality. Neurology 47:83–89
Shneker BF, Fountain NB (2003) Assessment of acute morbidity and mortality in nonconvulsive status epilepticus. Neurology 61:1066–1073
Treiman DM, Meyers PD, Walton NY, Collins JF, Colling C, Rowan AJ, Handforth A, Faught E, Calabrese VP, Uthman BM (1998) A comparison of four treatments for generalized convulsive status epilepticus. N Engl J Med 339:792–798
Brophy GM, Bell R, Claassen J, Alldredge B, Bleck TP, Glauser T, LaRoche SM, Riviello JJ, Shutter L, Sperling MR (2012) Guidelines for the evaluation and management of status epilepticus. Neurocrit Care 17:3–23
Sinha SR, Sullivan LR, Sabau D, Orta DSJ, Dombrowski KE, Halford JJ, Hani AJ, Drislane FW, Stecker MM (2016) American clinical neurophysiology society guideline 1: minimum technical requirements for performing clinical electroencephalography. Neurodiagn J 56:235–244
Beniczky S, Hirsch LJ, Kaplan PW, Pressler R, Bauer G, Aurlien H, Brøgger JC, Trinka E (2013) Unified EEG terminology and criteria for nonconvulsive status epilepticus. Epilepsia 54:28–29
Hirsch LJ, LaRoche SM, Gaspard N, Gerard E, Svoronos A, Herman ST, Mani R, Arif H, Jette N, Minazad Y, Kerrigan JF, Vespa P, Hantus S, Claassen J, Young GB, So E, Kaplan PW, Nuwer MR, Fountain NB, Drislane FW (2013) American clinical neurophysiology society’s standardized critical care EEG terminology: 2012 version. J Clin Neurophysiol 30:1–27
Glauser T, Shinnar S, Gloss D, Alldredge B, Arya R, Bainbridge J, Bare M, Bleck T, Dodson WE, Garrity L (2016) Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: report of the guideline committee of the american epilepsy society. Epilepsy curr 16:48–61
Laccheo I, Sonmezturk H, Bhatt AB, Tomycz L, Shi Y, Ringel M, DiCarlo G, Harris D, Barwise J, Abou-Khalil B (2015) Non-convulsive status epilepticus and non-convulsive seizures in neurological ICU patients. Neurocrit Care 22:202–211
Leitinger M, Trinka E, Gardella E, Rohracher A, Kalss G, Qerama E, Höfler J, Hess A, Zimmermann G, Kuchukhidze G (2016) Diagnostic accuracy of the Salzburg EEG criteria for non-convulsive status epilepticus: a retrospective study. Lancet Neurol 15:1054–1062
Goselink RJ, van Dillen JJ, Aerts M, Arends J, van Asch C, van der Linden I, Pasman J, Saris CG, Zwarts M, van Alfen N (2019) The difficulty of diagnosing NCSE in clinical practice; external validation of the Salzburg criteria. Epilepsia 60:e88–e92
Swisher CB, Shah D, Sinha SR, Husain AM (2015) Baseline EEG pattern on continuous ICU EEG monitoring and incidence of seizures. J Clin Neurophysiol 32:147–151
Claassen J, Mayer S, Kowalski R, Emerson R, Hirsch L (2004) Detection of electrographic seizures with continuous EEG monitoring in critically ill patients. Neurology 62:1743–1748
Westover MB, Shafi MM, Bianchi MT, Moura LM, O’rourke D, Rosenthal ES, Chu CJ, Donovan S, Hoch DB, Kilbride RD (2015) The probability of seizures during EEG monitoring in critically ill adults. Clin Neurophysiol 126:463–471
Trinka E, Leitinger M (2015) Which EEG patterns in coma are nonconvulsive status epilepticus? Epilepsy Behav 49:203–222
Yuan F, Yang F, Li W, Yang X, Gao Q, Bi L, Jiang Y, Jiang W (2018) Nonconvulsive status epilepticus after convulsive status epilepticus: Clinical features, outcomes, and prognostic factors. Epilepsy Res 142:53–57
Koutroumanidis M, Sakellariou D (2015) Low frequency nonevolving generalized periodic epileptiform discharges and the borderland of hypoxic nonconvulsive status epilepticus in comatose patients after cardiac arrest. Epilepsy Behav 49:255–262
Shafi MM, Westover MB, Cole AJ, Kilbride RD, Hoch DB, Cash SS (2012) Absence of early epileptiform abnormalities predicts lack of seizures on continuous EEG. Neurology 79:1796–1801
Struck AF, Osman G, Rampal N, Biswal S, Legros B, Hirsch LJ, Westover MB, Gaspard N (2017) Time-dependent risk of seizures in critically ill patients on continuous electroencephalogram. Ann Neurol 82:177–185
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aslan-Kara, K., Demir, T., Satılmış, Ü. et al. Prognostic indicators of non-convulsive status epilepticus in intensive care unit. Acta Neurol Belg 123, 1257–1266 (2023). https://doi.org/10.1007/s13760-022-01981-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-022-01981-6