Abstract
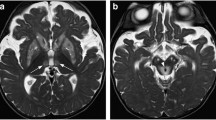
MRI signal changes in the brainstem are observed in a multitude of disorders including vascular diseases, neoplastic lesions, degenerative diseases, inflammatory disorders, metabolic diseases, infections, and trauma. In some diseases, brainstem involvement is typical and sometimes isolated, while in other diseases, brainstem lesions are only observed occasionally in the presence of other typical extra-brainstem abnormalities. In this review, we will discuss the MRI characteristics of brainstem lesions observed in different disorders associated with frequent and less frequent brainstem involvement. Identification of the origin of the brainstem lesion depends on the exact localisation of the lesion(s) inside the brainstem, the presence and the characteristics of associated lesions seen outside the brainstem, the signal changes on different MRI sequences, the evolution over time of the radiological abnormalities, the history and clinical state of the patient, and other radiological and non-radiological examinations.







Similar content being viewed by others
References
Tatu L, Moulin T, Bogousslavsky J, Duvernoy H (1996) Arterial territories of human brain: Brainstem and cerebellum. Neurology 47(5):1125–1135
Connell L, Koerte IK, Laubender RP, Morhard D, Linn J, Becker HC et al (2012) Hyperdense basilar artery sign—a reliable sign of basilar artery occlusion. Neuroradiology 54(4):321–327
Ernst M, Romero JM, Buhk J-H, Cheng B, Herrmann J, Fiehler J, et al. Sensitivity of Hyperdense Basilar Artery Sign on Non-Enhanced Computed Tomography. Hendrikse J, editor. PLoS ONE. 2015 Oct 19;10(10):e0141096.
Sylaja PN, Coutts SB, Krol A, Hill MD, Demchuk AM (2008) When to Expect Negative Diffusion-Weighted Images in Stroke and Transient Ischemic Attack. Stroke 39(6):1898–1900
Chen X, Wang J, Shan Y, Cai W, Liu S, Hu M et al (2019) Cerebral small vessel disease: neuroimaging markers and clinical implication. J Neurol 266(10):2347–2362
Hakky MM, Erbay KD, Brewer E, Midle JB, French R, Erbay SH (2013) T2 Hyperintensity of medial lemniscus: higher threshold application to ROI measurements is more accurate in predicting small vessel disease. J Neuroimaging 23(3):345–351
Erbay SH, Brewer E, French R, Midle JB, Zou KH, Lee GM et al (2012) T2 Hyperintensity of medial lemniscus is an indicator of small-vessel disease. Am J Roentgenol 199(1):163–168
Fakan B, Reisz Z, Zadori D, Vecsei L, Klivenyi P, Szalardy L (2020) Predictors of localization, outcome, and etiology of spontaneous intracerebral hemorrhages: focus on cerebral amyloid angiopathy. J Neural Transm 127(6):963–972
Aguilar MI, Brott TG (2011) Update in Intracerebral Hemorrhage. The Neurohospitalist 1(3):148–159
Flemming KD, Link MJ, Christianson TJH, Brown RD (2012) Prospective hemorrhage risk of intracerebral cavernous malformations. Neurology 78(9):632–636
Kashefiolasl S, Bruder M, Brawanski N, Herrmann E, Seifert V, Tritt S et al (2018) A benchmark approach to hemorrhage risk management of cavernous malformations. Neurology 90(10):e856–e863
Salman RA-S, Hall JM, Horne MA, Moultrie F, Josephson CB, Bhattacharya JJ, et al (2012) Untreated clinical course of cerebral cavernous malformations: a prospective, population-based cohort study. Lancet Neurol 11(3):217–24
Hou K, Li G, Qu L, Liu H, Xu K, Yu J (2020) Intracranial dural arteriovenous fistulas with brainstem engorgement: an under-recognized entity in diagnosis and treatment. Front Neurol 11:526550
Grigoryan G, Sitnikov A, Grigoryan Y (2020) Hemifacial spasm caused by the brainstem developmental venous anomaly: a case report and review of the literature. Surg Neurol Int 6(11):141
Rudie JD, Rauschecker AM, Nabavizadeh SA, Mohan S (2018) Neuroimaging of dilated perivascular spaces: from benign and pathologic causes to mimics: perivascular spaces. J Neuroimaging 28(2):139–149
Kwee RM, Kwee TC (2007) Virchow-robin spaces at MR imaging. Radiographics 27(4):1071–1086
Wardlaw JM, Smith C, Dichgans M (2019) Small vessel disease: mechanisms and clinical implications. Lancet Neurol 18(7):684–696
Reyes-Botero G, Mokhtari K, Martin-Duverneuil N, Delattre J, Laigle-Donadey F (2012) Adult brainstem gliomas. Oncologist 17(3):388–397
Villanueva-Meyer JE, Mabray MC, Cha S (2017) Current clinical brain tumor imaging. Neurosurgery 81(3):397–415
Fink JR, Muzi M, Peck M, Krohn KA (2015) Multimodality brain tumor imaging: MR imaging, PET, and PET/MR imaging. J Nucl Med 56(10):1554–1561
Schob S, Meyer J, Gawlitza M, Frydrychowicz C, Müller W, Preuss M, et al (2016) Diffusion-Weighted MRI reflects proliferative activity in primary CNS lymphoma. Coles JA, editor. PLoS ONE 11(8):e0161386.
Yuh EL, Barkovich AJ, Gupta N (2009) Imaging of ependymomas: MRI and CT. Childs Nerv Syst 25(10):1203
Luna LP, Drier A, Aygun N, Mokhtari K, Hoang-Xuan K, Galanaud D et al (2021) MRI features of intra-axial histiocytic brain mass lesions. Clin Radiol 76(2):159.e19-159.e28
Kim H-J, Jeon B, Fung VSC (2017) Role of magnetic resonance imaging in the diagnosis of multiple system atrophy. Mov Disord Clin Pract 4(1):12–20
Deguchi K, Ikeda K, Kume K, Takata T, Kokudo Y, Kamada M et al (2015) Significance of the hot-cross bun sign on T2*-weighted MRI for the diagnosis of multiple system atrophy. J Neurol 262(6):1433–1439
Mascalchi M, Vella A (2018) Neuroimaging Applications in Chronic Ataxias. In: International Review of Neurobiology [Internet]. Elsevier [cited 2021 Feb 19]. p. 109–62. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0074774218301119
Whitwell JL, Höglinger GU, Antonini A, Bordelon Y, Boxer AL, Colosimo C et al (2017) Radiological biomarkers for diagnosis in PSP: Where are we and where do we need to be? Neuroimaging Biomarkers for Diagnosis in PSP. Mov Disord 32(7):955–971
Sugiyama A, Sato N, Nakata Y, Kimura Y, Enokizono M, Maekawa T et al (2018) Clinical and magnetic resonance imaging features of elderly onset dentatorubral-pallidoluysian atrophy. J Neurol 265(2):322–329
Sugiyama A, Sato N, Kimura Y, Fujii H, Shigemoto Y, Suzuki F, et al (2020) The cerebellar white matter lesions in dentatorubral-pallidoluysian atrophy. J Neurol Sci 416:117040
Fabes J, Matthews L, Filippini N, Talbot K, Jenkinson M, Turner MR (2017) Quantitative FLAIR MRI in Amyotrophic Lateral Sclerosis. Acad Radiol 24(10):1187–1194
Sastre-Garriga J, Tintoré M, Nos C, Tur C, Río J, Téllez N et al (2010) Clinical features of CIS of the brainstem/cerebellum of the kind seen in MS. J Neurol 257(5):742–746
Tintore M, Rovira A, Arrambide G, Mitjana R, Rio J, Auger C et al (2010) Brainstem lesions in clinically isolated syndromes. Neurology 75(21):1933–1938
Minneboo A, Barkhof F, Polman CH, Uitdehaag BMJ, Knol DL, Castelijns JA (2004) Infratentorial Lesions Predict Long-term Disability in Patients With Initial Findings Suggestive of Multiple Sclerosis. Arch Neurol 61(2):217
Nakashima I, Fujihara K, Okita N, Takase S, Itoyama Y (1999) Clinical and MRI study of brain stem and cerebellar involvement in Japanese patients with multiple sclerosis. J Neurol Neurosurg Psychiatry 67(2):153–157
Nakashima I, Fujihara K, Kimpara T, Okita N, Takase S, Itoyama Y (2001) Linear pontine trigeminal root lesions in multiple sclerosis: clinical and magnetic resonance imaging studies in 5 cases. Arch Neurol [Internet]. 2001 Jan 1 [cited 2021 Feb 19];58(1). Available from: http://archneur.jamanetwork.com/article.aspx?doi=https://doi.org/10.1001/archneur.58.1.101
Keegan BM, Kaufmann TJ, Weinshenker BG, Kantarci OH, Schmalstieg WF, Paz Soldan MM et al (2016) Progressive solitary sclerosis: Gradual motor impairment from a single CNS demyelinating lesion. Neurology 87(16):1713–1719
Chan KH (2011) Brain involvement in neuromyelitis optica spectrum disorders. Arch Neurol 68(11):1432
Kim HJ, Paul F, Lana-Peixoto MA, Tenembaum S, Asgari N, Palace J et al (2015) MRI characteristics of neuromyelitis optica spectrum disorder: an international update. Neurology 84(11):1165–1173
Banks SA, Morris PP, Chen JJ, Pittock SJ, Sechi E, Kunchok A et al (2021) Brainstem and cerebellar involvement in MOG-IgG-associated disorder versus aquaporin-4-IgG and MS. J Neurol Neurosurg Psychiatry 92(4):384–390
Koelman DLH, Mateen FJ (2015) Acute disseminated encephalomyelitis: current controversies in diagnosis and outcome. J Neurol 262(9):2013–2024
Kalra S, Silman A, Akman-Demir G, Bohlega S, Borhani-Haghighi A, Constantinescu CS et al (2014) Diagnosis and management of Neuro-Behçet’s disease: international consensus recommendations. J Neurol 261(9):1662–1676
Simon NG, Parratt JD, Barnett MH, Buckland ME, Gupta R, Hayes MW et al (2012) Expanding the clinical, radiological and neuropathological phenotype of chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS). J Neurol Neurosurg Psychiatry 83(1):15–22
Taieb G, Duflos C, Renard D, Audoin B, Kaphan E, Pelletier J et al (2012) Long-term Outcomes of CLIPPERS (Chronic Lymphocytic Inflammation With Pontine Perivascular Enhancement Responsive to Steroids) in a Consecutive Series of 12 Patients. Arch Neurol [Internet]. 69(7). Available from: http://archneur.jamanetwork.com/article.aspx?doi=https://doi.org/10.1001/archneurol.2012.122
Martin RJ (2004) Central pontine and extrapontine myelinolysis: the osmotic demyelination syndromes. J Neurol Neurosurg Psychiatry. 2004 75(suppl_3):iii22–8
Kallakatta RN, Radhakrishnan A, Fayaz RK, Unnikrishnan JP, Kesavadas C, Sarma SP (2011) Clinical and functional outcome and factors predicting prognosis in osmotic demyelination syndrome (central pontine and/or extrapontine myelinolysis) in 25 patients. J Neurol Neurosurg Psychiatry 82(3):326–331
Ruzek KA, Campeau NG, Miller GM (2004) Early diagnosis of central pontine myelinolysis with diffusion-weighted imaging. AJNR Am J Neuroradiol 25(2):210–213
Manzo G, De Gennaro A, Cozzolino A, Serino A, Fenza G, Manto A (2014) MR imaging findings in alcoholic and nonalcoholic acute Wernicke’s encephalopathy: a review. Biomed Res Int 2014:1–12
Nardone R, Venturi A, Golaszewski S, Caleri F, Tezzon F, Ladurner G (2010) MR atypical wernicke encephalopathy showing extensive brain stem and diencephalic involvement. J Neuroimaging 20(2):204–207
Rovira A, Alonso J, Córdoba J (2008) MR imaging findings in hepatic encephalopathy. AJNR Am J Neuroradiol 29(9):1612–1621
Li K, Yang Y, Guo D, Sun D, Li C (2020) Clinical and MRI features of posterior reversible encephalopathy syndrome with atypical regions: a descriptive study with a large sample size. Front Neurol 24(11):194
Bonfante E, Koenig MK, Adejumo RB, Perinjelil V, Riascos RF (2016) The neuroimaging of Leigh syndrome: case series and review of the literature. Pediatr Radiol 46(4):443–451
Baertling F, Rodenburg RJ, Schaper J, Smeitink JA, Koopman WJH, Mayatepek E et al (2014) A guide to diagnosis and treatment of Leigh syndrome. J Neurol Neurosurg Psychiatry 85(3):257–265
Salari M, Fayyazi E, Mirmosayyeb O (2018) Magnetic resonance imaging findings in diagnosis and prognosis of Wilson disease. J Res Med Sci 23(1):23
Dusek P, Litwin T, Członkowska A (2019) Neurologic impairment in Wilson disease. Ann Transl Med 7(S2):S64–S64
Hitoshi S, Iwata M, Yoshikawa K (1991) Mid-brain pathology of Wilson’s disease: MRI analysis of three cases. J Neurol Neurosurg Psychiatry 54(7):624–626
Demaerel P, Van Dessel W, Van Paesschen W, Vandenberghe R, Van Laere K, Linn J (2011) Autoimmune-mediated encephalitis. Neuroradiology 53(11):837–851
Michev A, Musso P, Foiadelli T, Trabatti C, Lozza A, Franciotta D et al (2019) Bickerstaff Brainstem Encephalitis and overlapping Guillain-Barré syndrome in children: report of two cases and review of the literature. Eur J Paediatr Neurol 23(1):43–52
Köhler W, Curiel J, Vanderver A (2018) Adulthood leukodystrophies. Nat Rev Neurol 14(2):94–105
Ayrignac X, Boutiere C, Carra-dalliere C, Labauge P (2016) Posterior fossa involvement in the diagnosis of adult-onset inherited leukoencephalopathies. J Neurol 263(12):2361–2368
Shen Y, Jian W, Li J, Dai T, Bao B, Nie H (2018) Bilateral wallerian degeneration of the middle cerebellar peduncles secondary to pontine infarction: A case series. J Neurol Sci 388:182–185
Konno T, Broderick DF, Tacik P, Caviness JN, Wszolek ZK (2016) Hypertrophic olivary degeneration: a clinico-radiologic study. Parkinsonism Relat Disord 28:36–40
Bertrand A, Leclercq D, Martinez-Almoyna L, Girard N, Stahl J-P, De-Broucker T (2017) MR imaging of adult acute infectious encephalitis. Med Mal Infect 47(3):195–205
Breville G, Koralnik IJ, Lalive PH (2021) Brainstem progressive multifocal leukoencephalopathy. Eur J Neurol 28(3):1016–1021
Hodel J, Outteryck O, Dubron C, Dutouquet B, Benadjaoud MA, Duhin E et al (2016) Asymptomatic progressive multifocal leukoencephalopathy associated with natalizumab: diagnostic precision with MR imaging. Radiology 278(3):863–872
Wijburg MT, Witte BI, Vennegoor A, Roosendaal SD, Sanchez E, Liu Y et al (2016) MRI criteria differentiating asymptomatic PML from new MS lesions during natalizumab pharmacovigilance. J Neurol Neurosurg Psychiatry 87(10):1138–1145
Sandhu S, Soule E, Fiester P, Natter P, Tavanaiepour D, Rahmathulla G et al (2019) Brainstem diffuse axonal injury and consciousness. JCIS 28(9):32
Acknowledgements
We would like to thank Dr. Sarah Kabani (Service de Biostatistique, Epidémiologie Clinique, Santé Publique et Innovation en Méthodologie (BESPIM), CHU de Nîmes, 4 Rue du Professeur Debré, 30029 Nîmes Cedex 09) for proofreading our manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
The subject has given her informed consent to report data given. The manuscript was approved by the institute’s committee on human research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.














Rights and permissions
About this article
Cite this article
Renard, D., Guillamo, JS., Ion, I. et al. Brainstem lesions: MRI review of standard morphological sequences. Acta Neurol Belg 122, 597–613 (2022). https://doi.org/10.1007/s13760-022-01943-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-022-01943-y