Abstract
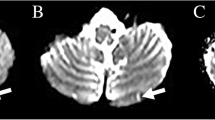
Caudal paramedian midbrain infarction (CPMI) is an extremely rare form of ischemic stroke and related clinical studies are scarce. Our aim is to investigate the clinical features, neuroradiological findings and stroke etiology of CPMI. We conducted a retrospective study of 12 patients with CPMI, confirmed by diffusion-weighted MRI from 6820 cerebral infarction patients at our stroke center from January 2012 to August 2018. Experienced neurologists evaluated the clinical manifestations, neuroimaging findings and stroke mechanisms. Twelve patients (11 men, 1 woman) aged 42–81 years old met the study inclusion criteria. Seven patients had a unilateral infarction (two right-sided, five left-sided) and five had bilateral infarctions. Sagittal image showed a backward oblique sign in the lower level of the midbrain. Significantly, the bilateral CPMIs presented with a characteristic “V-shaped” appearance in the axial MRI. All patients presented with bilateral cerebellar dysfunction which included dysarthric speech, truncal or gait ataxia and four-limb ataxia. In addition, diplopia and internuclear ophthalmoplegia were frequently encountered in CPMI. Five (41.7%) patients were classified with large artery atherosclerosis, four (33.3%) with small vessel disease, two (16.7%) with cardiogenic embolism, and one (8.3%) with undetermined etiology. CPMI is a rare cerebrovascular disease that destroys the Wernekink commissure, medial longitudinal fasciculi and other adjacent structures. It is characterized by bilateral cerebellar ataxia and eye movement disorders, mainly internuclear ophthalmoplegia. A distinct “V-shaped” radiological feature can be seen in bilateral CPMI patients. The primary mechanisms of unilateral CPMI involve small vessel disease. The underlying stroke mechanisms of bilateral CPMI are either large artery atherosclerosis disease or cardiac embolism.






Similar content being viewed by others
References
Mossuto-Agatiello L (2006) Caudal paramedian midbrain syndrome. Neurology 66(11):1668–1671. https://doi.org/10.1212/01.wnl.0000218180.03127.11
Chenguang Z, Yuanhong H, Zhiwen C, Yinghui Z, Peng W, Xingping W et al (2017) Wernekink commissure syndrome secondary to bilateral caudal paramedian midbrain infarction presenting with a unique “heart or V” appearance sign: case report and review of the literature. Front Neurol 8:376. https://doi.org/10.3389/fneur.2017.00376
Lhermitte F (1958) the cerebellar syndrome: anatomo-clinical study in the adult. Rev Neurol 98(6):435–477
Cerrato P, Lentini A, Colonna R, Bosco G, Destefanis E, Caprioli M et al (2008) Gait and bilateral limb ataxia as isolated feature of a lower midbrain tegmental infarction. J Neurol 255(2):290–291. https://doi.org/10.1007/s00415-006-0506-3
Okuda B, Tachibana H, Sugita M, Maeda Y (1993) Bilateral internuclear ophthalmoplegia, ataxia, and tremor from a midbrain infarction. Stroke J Cereb Circ 24(3):481–482. https://doi.org/10.1161/01.STR.24.3.481
Zhou C, He Y, Chao Z, Zhu Y, Wang P, Gao X (2017) The “heart appearance” sign on MRI of Wernekink’s commissure syndrome caused by bilateral caudal paramedian midbrain infarction. Neurol Sci. https://doi.org/10.1007/s10072-017-3159-3
Zhu Y, Liu HN, Zhang CD (2010) Wernekinck commissure syndrome is a pure midbrain infarction. J Clin Neurosci 17(8):1091–1092. https://doi.org/10.1016/j.jocn.2009.11.032
Mullaguri N, Battineni A, Chuquilin M (2018) Wernekink commissure syndrome with palatal myoclonus at onset: a case report and review of the literature. J Med Case Rep 12(1):113. https://doi.org/10.1186/s13256-018-1657-4
Sheetal S, Byju P (2016) Wernekink commissure syndrome. Neurol India 64:1055–1057
Dai AI, Wasay M (2006) Wernekink commissure syndrome: a rare midbrain syndrome secondary to stroke. JPMA J Pak Med Assoc 56(6):289–290
Sato S, Toyoda K, Kawase K, Kasuya J, Minematsu K (2008) A caudal mesencephalic infarct presenting only with tetra-ataxia and tremor. Cerebrovasc Dis 25(1–2):187–189. https://doi.org/10.1159/00011373
Kim TW, Yoo S, Koo J (2014) Wernekink commissure syndrome secondary to ischemic stroke: severe dysarthria is one of the main characteristics of this syndrome. Neurol Sci 35(9):1475–1477. https://doi.org/10.1007/s10072-014-1789-2
Spengos K (2005) Bilateral paramedian midbrain infarct: an uncommon variant of the “top of the basilar” syndrome. J Neurol Neurosurg Psychiatry 76(5):742–743. https://doi.org/10.1136/jnnp.2004.050146
Kumral E, Bayulkem G, Akyol A, Yunten N, Sirin H, Sagduyu A (2002) Mesencephalic and associated posterior circulation infarcts. Stroke 33(9):2224–2231. https://doi.org/10.1161/01.STR.0000027438.93029.87
Burger KM, Tuhrim S, Neidich TP (2005) Brainstem vascular stroke anatomy. Neuroimag Clin N Am 15(2):297–324. https://doi.org/10.1016/j.nic.2005.05.005
Voogd J, Baarsen KV (2013) The horseshoe-shaped commissure of Wernekinck or the decussation of the brachium conjunctivum methodological changes in the 1840s. Cerebellum 13(1):113–120. https://doi.org/10.1007/s12311-013-0520-9
Tatu L, Moulin T, Bogousslavsky J, Duvernoy H (1996) Arterial territories of human brain brainstem and cerebellum. Neurology 47(5):1125. https://doi.org/10.1212/WNL.47.5.1125
Pedroza A, Dujovny M, Ausman JI, Diaz FG, Artero JC, Berman SK et al (1986) Microvascular anatomy of the interpeduncular fossa. J Neurosurg 64(3):484–493. https://doi.org/10.3171/jns.1986.64.3.0484
Lamot U, Ribaric I, Popovic KS, Lamot U (2015) Artery of percheron infarction: review of literature with a case report. Radiol Oncol. https://doi.org/10.2478/raon-2014-0037
Lazzaro NA, Wright B, Castillo M, Fischbein NJ, Glastonbury CM, Hildenbrand PG et al (2010) Artery of percheron infarction: imaging patterns and clinical spectrum. Am J Neuroradiol 31(7):1283–1289. https://doi.org/10.3174/ajnr.A2044
Viticchi G, Falsetti L, Fiori C, Jorio G, Plutino A, Buratti L et al (2016) Acute occlusion of the percheron artery during pregnancy: a case report and a review of the literature. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc 25(3):572–577. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.11.011
Wang X, Fan YH, Lam WWM, Leung TWH, Wong KS (2008) Clinical features, topographic patterns on DWI and etiology of thalamic infarcts. J Neurol Sci 267(1–2):147–153. https://doi.org/10.1016/j.jns.2007.10.014
Weidauer S, Nichtweiss M, Zanella FE, Lanfermann H (2004) Assessment of paramedian thalamic infarcts: mr imaging, clinical features and prognosis. Eur Radiol 14(9):1615–1626. https://doi.org/10.1007/s00330-004-2303-7
Wu YT, Cafiero-Chin M, Marques C (2015) Wall-eyed bilateral internuclear ophthalmoplegia: review of pathogenesis, diagnosis, prognosis and management. Clin Exp Optom 98(1):25–30. https://doi.org/10.1111/cxo.12200
Konno T, Broderick DF, Tacik P, Caviness JN, Wszolek ZK (2016) Hypertrophic olivary degeneration: a clinico-radiologic study. Parkinson Relat Disord 28:36–40. https://doi.org/10.1016/j.parkreldis.2016.04.008
Caballero Pedro Enrique Jiménez (2010) Bilateral paramedian thalamic artery infarcts: report of ten cases. J Stroke Cerebrovasc Dis 19(4):289. https://doi.org/10.1016/j.jstrokecerebrovasdis.2009.07.003
Acknowledgements
The authors thank Longnv Luo and Daokuan Zhou for their assistance in preparation of the manuscript.
Funding
This work was supported by Key Research Program for Higher Education of Henan Province, China (ID 18A320071)
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
We declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval
This retrospective study was approved by the Institutional Review Board of the affiliated hospital of the Fifth Affiliated Hospital of Zhengzhou University. All procedures performed in studies were in accordance with the ethical standards of the Institutional Review Board of the affiliated hospital of the Fifth Affiliated Hospital of Zhengzhou University and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
In addition, the informed consent was waived due to the retrospective nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, C., Xu, Z., Huang, B. et al. Caudal paramedian midbrain infarction: a clinical study of imaging, clinical features and stroke mechanisms. Acta Neurol Belg 121, 443–450 (2021). https://doi.org/10.1007/s13760-019-01204-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-019-01204-5