Abstract
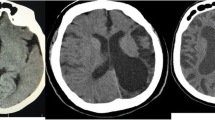
Radiological findings of Dyke–Davidoff–Masson syndrome (DDMS) in patients with different etiologies are presented in our study. The study included 12 patients (seven females, five males) for whom radiological examinations were requested due to reasons such as epilepsy, mental retardation, and/or hemiplegia. CT was performed in 12, MRI in 6, MRA in 1, and DSA in 1 patient. Following imaging findings were evaluated: cerebral and cerebellar involvement (laterality, encephalomalacia), affected territories, ventricular enlargement, sulcal enlargement, calvarial thickening, and paranasal sinus enlargement hyperaeration. Age range of the patients was 5–62 (mean 34.1 ± 21.7). Left hemicrania was affected in eight patients, right hemicrania in four. Ipsilateral calvarial thickening and lateral ventricular dilatation were observed in all patients. 11 patients had ipsilateral frontal sinus hyperaeration, sulcal enlargement and encephalomalacia. Wallerian degeneration of the mesencephalon and middle fossa hypoplasia was seen in ten patients, mastoid hyperaeration, third ventricular enlargement and thalamic involvement in nine, and corpus callosum, basal ganglion injury, and sphenoid sinus hyperaeration in eight. MCA, ACA, and PCA territories were involved in six patients. Only MCA territory involvement was seen in four patients. Cerebellar atrophy was contralateral in two patients. Symmetric bilateral atrophy was observed in one patient. DDMS can be encountered with different radiological findings based on cerebral damage formation process and the extent of damage. Patients may have different levels of cerebral hemiatrophy, ipsilateral carvarial thickening, and lateral ventricular dilatation.



Similar content being viewed by others
References
Arora R, Rani JY (2015) Dyke–Davidoff–Masson syndrome: imaging features with illustration of two cases. Quant Imaging Med Surg 5(3):469–471. doi:10.3978/j.issn.2223-4292.2014.11.17
Atalar MH, Icagasioglu D, Tas F (2007) Cerebral hemiatrophy (Dyke–Davidoff–Masson syndrome) in childhood: clinicoradiological analysis of 19 cases. Pediatr Int 49(1):70–75
Singh P, Saggar K, Ahluwalia A (2010) Dyke–Davidoff–Masson syndrome: classical imaging findings. J Pediatr Neurosci. 5(2):124–125. doi:10.4103/1817-1745.76108
Uduma FU, Emejulu JK, Motah M, Okere PC, Ongolo PC, Muna W (2013) Differential diagnoses of cerebral hemiatrophy in childhood: a review of literature with illustrative report of two cases. Glob J Health Sci 5(3):195–207
Bükte Y, Oysu AS, Ekici F, Hattapoğlu S, Sakcı Z, Fidan E (2014) Dyke–Davidoff–Masson syndrome (cerebral hemiatrophy): radiological findings. Dicle Med J 41(2):375–379. doi:10.5798/diclemedj.0921.2014.02.0434
Tasdemir HA, Incesu L, Yazicioglu AK, Belet U, Gungor L (2002) Dyke–Davidoff–Masson syndrome. Clin Imaging 26:13–17
Dyke CG, Davidoff LM, Masson CB (1933) Cerebral hemiatrophy with homolateral hypertrophy of the skull and sinuses. Surg Gynecol Obstet 57:588–600
Demir Y, Sürücü E, Çilingir V, Bulut MD, Tombul T (2015) Dyke–Davidoff–Masson syndrome with cerebral hypometabolism and unique crossed cerebellar diaschisis in 18F-FDG PET/CT. Clin Nucl Med 40(9):757–758. doi:10.1097/RLU.0000000000000890
Dutta A, Bose S, Sen K, Pandit N, Sharma S (2016) Refractory seizure in childhood: Dyke–Davidoff–Masson syndrome revisited. Oman Med J. 31(4):304–308. doi:10.5001/omj.2016.58
Shrestha B (2013) Acquired cerebral hemiatrophy: Dyke–Davidoff–Masson Syndrome—a case report. Turk Neurosurg 23(1):117–121. doi:10.5137/1019-5149.JTN.4283-11.1
Piro E, Piccione M, Marrone G, Giuffrè M, Corsello G (2013) Dyke–Davidoff–Masson syndrome: case report of fetal unilateral ventriculomegaly and hypoplastic left middle cerebral artery. Ital J Pediatr 14(39):32. doi:10.1186/1824-7288-39-32
Shen WC, Chen CC, Lee SK, Ho YJ, Lee KR (1993) Magnetic resonance imaging of cerebral hemiatrophy. J Formos Med Assoc 92:995–1000
Roy U, Panwar A, Mukherjee A, Biswas D (2016) Adult presentation of Dyke–Davidoff–Masson syndrome: a case report. Case Rep Neurol. 8(1):20–26. doi:10.1159/000443521 (eCollection 2016 Jan-Apr)
Roy K, Talukdar A, Ray S, Pal P (2012) Dyke–Davidoff–Masson syndrome-like picture in a case of Takayasu arteritis: an enigma. BMJ Case Rep. doi:10.1136/bcr-2012-006669 ([pii]: bcr2012006669)
Narain NP, Kumar R, Narain B (2008) Dyke–Davidoff–Masson syndrome. Indian Pediatr 45(11):927–928
Thomas-Sohl KA, Vaslow DF, Maria BL (2004) Sturge–Weber syndrome: a review. Pediatr Neurol 30:303–310
Sharma S, Goyal D, Negi A, Sood RG, Jhobta A, Surya M (2006) Dyke-Davidoff Masson syndrome. Indian J Radiol Imaging 16:165–166
Zamora CA, Kontzialis M (2015) Teaching neuroimages: Dyke–Davidoff–Masson in Sturge–Weber syndrome. Neurology. 85(16):e128. doi:10.1212/WNL.0000000000002043
Bekci T, Bilgici MC, Turgut E, Aslan K (2016) A rare combination: Sturge–Weber syndrome and accompanying Dyke–Davidoff–Masson syndrome. Acta Neurol Belg 116(1):79–81. doi:10.1007/s13760-015-0511-3
Corey SA, O’Donovan CA (2005) Sturge–Weber syndrome and accompanying Dyke–Davidoff–Masson syndrome. Arch Neurol 62(12):1928–1929
Sheybani L, Schaller K, Seeck M (2011) Rasmussen encephalitis: an update. Schweiz Arch Neurol Psychiatr 162:225–231
Moon WK, Chang KH, Kim IO, Han MH, Choi CG, Suh DC et al (1994) Germinomas of the basal ganglia and thalamus: MR findings and a comparison between MR and CT. AJR Am J Roentgenol 162:1413–1417
Amar DJ, Kornberg AJ, Smith LJ (2000) Encephalocraniocutaneous lipomatosis (Fishman syndrome): a rare neurocutaneous syndrome. J Pediatr Child Health 36:603–605
Qiu BP, Shi CH (2007) Silver-Russel syndrome: a case report. World J Pediatr 3:68–70
Unal O, Tombul T, Cırak B, Anlar O, Incesu L, Kayan M (2004) Left hemisphere and sex dominance of cerebral hemiatrophy (Dyke–Davidoff–Masson syndrome). Clin Imaging 28:163–165
Gupta R, Joshi S, Mittal A, Luthra I, Mittal P, Verma V (2015) Magnetic resonance imaging depiction of acquired Dyke–Davidoff–Masson syndrome with crossed cerebro-cerebellar diaschisis: report of two cases. J Pediatr Neurosci 10(3):294–296. doi:10.4103/1817-1745.165730
Hsin YL, Chuang MF, Shen TW, Harnod T (2011) Temporo-spatial analyses define epileptogenic and functional zones in a case of Dyke–Davidoff–Masson syndrome. Seizure. 20(9):713–716. doi:10.1016/j.seizure.2011.06.019
Pinto WB, de Souza PV, Pedroso JL, Barsottini OG (2013) Dyke–Davidoff–Masson syndrome: a combination of clinical and radiological signs not to be missed. Arq Neuropsiquiatr 71(11):911. doi:10.1590/0004-282X20130137
Menekşe G, Ozsoy KM, Ateş T, Okten Aİ, Güzel A (2013) Dyke–Davidoff–Masson syndrome associated with epidermoid tumour and arachnoid cyst: a case report. Balkan Med J. 30(4):432–435. doi:10.5152/balkanmedj.2013.8565
Park KI, Chung JM, Kim JY (2014) Dyke–Davidoff–Masson syndrome: cases of two brothers and literature review. J Epilepsy Res 4(1):24–27 (eCollection 2014)
Sharma B, Nagpal K, Handa R, Bhana I (2014) Dyke–Davidoff–Masson syndrome: a clinicoradiological amalgam. BMJ Case Rep. doi:10.1136/bcr-2014-204679 ([pii]: bcr2014204679)
Gupta A, Goyal MK, Singh P, Lal V (2016) Early transneuronal degeneration in Dyke–Davidoff–Masson syndrome. J Clin Neurol. 12(1):117–118. doi:10.3988/jcn.2016.12.1.117
Kumar NV, Gugapriya TS, Guru AT, Kumari SN (2016) Dyke–Davidoff–Masson syndrome. Int J Appl Basic Med Res 6(1):57–59. doi:10.4103/2229-516X.174016
Iwase T, Yoshida M, Mizuno T, Sato S, Nokura K (2015) An autopsy case of hemiconvulsion-hemiplegia-epilepsy syndrome manifesting as cerebral hemiatrophy in an elderly man. Neuropathology. 35(6):592–598. doi:10.1111/neup.12225
Donmez FY (2012) Re: Dyke–Davidoff–Masson syndrome in a 6,000-year-old skull. Neuroradiology 54(9):1027–1028. doi:10.1007/s00234-012-1060-6 (author reply 1029-30)
Basu S, Chouhan A (2013) Striking asymmetry in cerebral metabolism in Dyke–Davidoff–Masson (DDM) syndrome: FDG-PET and MRI correlation. Acta Neurochir (Wien). 155(3):519–521. doi:10.1007/s00701-012-1604-x
Winkler DT, Probst A, Wegmann W, Tolnay M (2001) Dyke Davidoff Masson syndrome with crossed cerebellar atrophy: an old disease in a new millenium. Neuropathol Appl Neurobiol 27(5):403–405
Saldanha D, Chaudhari B, Mehta SK, Javadekar AN, Kharat A (2014) Cerebral hemi atrophy as a consequence of cerebral insult in infancy: Is it difficult to diagnose? Ind Psychiatry J. 23(1):71–73. doi:10.4103/0972-6748.144978
Lin DD, Kleinman JT, Wityk RJ, Gottesman RF, Hillis AE, Lee AW et al (2009) Crossed cerebellar diaschisis in acute stroke detected by dynamic susceptibility contrast MR perfusion imaging. AJNR Am J Neuroradiol 30:710–715
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All information of this article is in accordance with national and international ethical standards. The manuscript has not been submitted to other journals for simultaneous consideration. Consent to publish has been received from all the authors. Authors whose names appear in the article have contributed sufficiently to the scientific work, and therefore share collective responsibility and accountability for the results. No personal details about the concerned patient was included in the article.
Informed consent
The ethical committee of Gaziosmanpaşa University (Tokat) approved the study.
Funding
There was no funding for this study.
Rights and permissions
About this article
Cite this article
Gökçe, E., Beyhan, M. & Sade, R. Radiological imaging findings of Dyke–Davidoff–Masson syndrome. Acta Neurol Belg 117, 885–893 (2017). https://doi.org/10.1007/s13760-017-0778-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-017-0778-7