Abstract
In 11 adult patients with suspicion of Focal cortical dysplasia (FCD) on 1.5 T (n = 1) or 3 T (n = 10) magnetic resonance imaging (MRI), 7 T MRI was performed. Visibility, extent, morphological features and delineation were independently rated and subsequently discussed by three observers. Additionally, head-to-head comparisons with corresponding 3 T images were made in the eight patients with a previous 3 T MRI and sustained suspicion of FCD. Comparison with histopathology was done in the five patients that underwent surgery. All lesions, seen at 1.5 and 3 T, were also recognized on 7 T. At 7 T FLAIR highlighted the FCD-like lesions best, whereas T2 and T2* were deemed better suited to review structure and extent of the lesion. Image quality with the used 7 T MRI setup was higher than the quality with the used 3 T MRI setup. In 2 out of 11 patients diagnosis changed, in one after re-evaluation of the images, and in the other based on histopathology. With the used 7 T MRI setup, FCD-like lesions can be detected with more confidence and detail as compared to lower field strength. However, concordance between radiologic diagnosis and final diagnosis seems to be lower than expected.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
20–40 % of epilepsy patients are drug resistant. In this group resective surgery, if possible, is the treatment of choice [1, 2]. Finding a lesion on magnetic resonance imaging (MRI) is of clinical importance, as presence of a lesion is associated with a higher chance of developing drug resistant (refractory) epilepsy [3] and increased success rate of surgery [4–6]. Sensitivity of MRI for brain lesions partly depends on the system’s magnetic field strength [7–12]. Higher field strength gives rise to higher signal-to-noise ratio, which allows for higher anatomical resolution and increased sensitivity for contrast mechanisms such as those based on iron [13–18]. Most studies in epilepsy patients have been performed using 1.5 and 3 T MRI systems. MRI systems operating at a magnetic field strength of 7 T may have added value for epilepsy patients [19] especially because they may have a higher sensitivity for focal cortical dysplasia (FCD) and decrease the number of MRI-occult FCDs. In surgical series, FCD is a common pathologic finding with a reported presence in 8 % [20] to 53 % of the operated epileptic patients [21]. 20–30 % of patients with postsurgical proven FCD were MRI-negative [3, 22, 23]. No systematic comparison between 3 and 7 T MRI appearance of FCD is available. On the other hand, MRI diagnosis of FCD can be erroneous. FCD’s can be hard to distinguish from gliomas, with a preference for FCD on frontal locations or a lesser distinct high intensity on T2 weighted images than in case of glioma [24].
The most frequently described MRI features of FCD include: increased cortical thickness, blurred grey/white matter junction, increased signal on T2, decreased signal on T1 of the subcortical white matter and gyration anomalies [22, 23]. The most typical feature highly specific for FCD type II is alteration of white matter signal towards the ventricle, the “transmantle sign” [25]. Presence of a focal lesion (e.g., mesiotemporal sclerosis) combined with FCD defines FCD type III. FCD can be characterised by combinations of several of the above mentioned MRI features [26]. In many patients only a subset of these MRI features are detected [26]. As presentation of an abnormality can be dependent on the field strength, we wanted to study the presentation on 7 T MRI of FCD’s previously described on lower field strength MRI. Further more findings on 3 T MRI if available were compared to the appearance at 7 T MRI and radiologic diagnosis was compared to histopathology in operated cases.
Methods
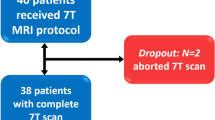
Ten adult patients, diagnosed with localisation related epilepsy and presence of a lesion diagnosed as FCD on 3 T (n = 10) or 1.5 T (n = 1) MRI, were included (patient characteristics: Table 1). An additional patient (patient 5) was excluded from further analysis as due to technical failure on 7 T MRI the signal-to-noise ratio was too low. All lesions were located extra-temporal, one with temporal extension and one with dual pathology. Standard MRI exclusion criteria were applied. Presence of a dental retainer wire was added as a 7 T-specific MRI exclusion criterion. At present this is not an exclusion criterion any more [27]. Informed consent was obtained from all individual participants included in the study. The study was approved by the Institutional Review Board of LUMC (Leiden Universitair Medisch Centrum).
7 T MRI was performed on a Philips Achieva platform (Philips Healthcare, Cleveland, Ohio) using a 32 channel receive head coil with quadrature transmit. The following sequences were used: 3D T1 (TR 4.2 ms, TE 1.88 ms, voxel-size 0.9 × 0.9 × 0.9 mm), 3D FLAIR (TR 7900 ms, TE 300 ms, TI 2200 ms, voxel-size 0.85 × 0.85 × 0.85 mm), T2 TSE (TR 3000 ms, TE 58 ms, voxel-size 0.5 × 0.5 × 1 mm) and T2* (TR 1764 ms, TE 25 ms, voxel-size 0.24 × 0.24 × 1 mm). Total acquisition time was under 1 h, which was considered acceptable for possible future use in clinical practice. The 3 T MRI images were acquired using a 16 channel receive head coil and a state-of-the-art epilepsy protocol [3D-T1 (TR 8.1 ms, TE 3.7 ms, voxel 1 × 1 × 1 mm), T2 (TR 3000 ms, TE 80 ms, voxel 0.5 × 0.5 × 5 mm), T2* in the last 5 patients (TR 777 ms, TE 16 ms, voxel 0.9x1.1x5 mm), IR (TR 120 ms, TE 10 ms, TI 400 ms, voxel 0.4 × 0.6 × 2 mm), FLAIR (TR 8000 ms, TE 50 ms, TI 2400 ms, voxel 1.1 × 1.1 × 0.5 mm)] performed on a Philips 3.0 T Achieva platform (Philips Medical systems, Best, The Netherlands). Diagnosis of FCD was made by an experienced neuroradiologist in a tertiary epilepsy centre (PH). In one patient only 1.5 T MRI, made in a referring hospital, was available; since this 1.5 T MRI examination showed clearly an FCD, additional 3 T MRI was deemed unnecessary.
Patient charts were examined by two neurologists (AC, LW), with experience in analysing patients for epilepsy surgery. Based on medical history, semiology, EEG, and if available seizure-recordings clinical estimation of the location of the epileptogenic focus was formulated. If the patient underwent surgery data on histopathology were noted. Data were compared to the MRI results.
Two experienced neuroradiologists (MvB, PH) and a neurologist (AC) visually inspected the images.
All observers were aware of the presence of an MRI-detectable lesion. Windowing was individually adapted to gain optimal contrast. Orientation of slides with the highest visibility of the abnormality was chosen separately for each field strength. Presence and characteristics of a possible FCD (see Table 2) were noted using a predefined scoring system. Seven features were scored: blurring of the grey–white matter junction, focal thickening of the cortex, focal increased intensity, presence of a transmantle sign, clear demarcation of transition to normal cortex, gyral pattern and abnormal internal structure. A flag-like appearance of the FCD was noted in several patients. This characteristic was added to the study.
In eight patients with a 3 T MRI and a sustained pre-operative diagnosis of FCD the features of the FCD on T2 and FLAIR images were rated for visibility using a Likert scale from 1 to 3 [28]: 1 indicating 7 T superior to 3 T, 2 equal quality, and 3 indicating 3 T superior to 7 T. Comparison was made between the same sequences using a Sign test (http://www.fon.hum.uva.nl/Service/Statistics/Sign_Test.html). Non-difference was set as the null hypothesis. As T2* was not available in all 3 T MRIs no comparison between T2* on 7 T and on 3 T sequence was made.
Results
In none of the patients abnormalities were found on 7 T MRI that were not observed at lower field strength and all lesions visible at lower field strength were visible at 7 T. In the ten analysed patients, both neurologists agreed that the stereotyped seizures were based on a single epileptogenic focus. In each patient one or more hypotheses on the possible locations of this epileptogenic focus could be postulated. Comparison between these hypotheses and the location of the lesion on MRI showed concordance in each individual patient.
By visual inspection in all patients the lesion was detected on 7 T MRI without prior knowledge of the location as seen at lower field strength. In patient 1 the diagnosis changed from FCD to cavernoma based on the 7 T MRI and re-evaluation of the 3 T images. The treating physician was informed. Further visual analysis of the 7 T MRI was done for the remaining nine patients.
On the T1-weighted images cortical thickening and blurring were most prominent (Fig. 1). A hypo-intense line at the grey–white matter junction was observed on T2 weighted images (Fig. 2) in eight patients creating a typical three layer flag-like appearance. Detection of the FCD was readily made on the FLAIR images (Fig. 3), whereas the abnormal internal structure of FCDs was most clearly seen on T2* (Fig. 4). Supplementary online data shows more examples. Of the seven imaging features, four (blurring of grey–white matter, focal signal increase, visibility of transition to normal cortex, abnormal internal structure) were observed in all nine patients. Focal thickening was observed in eight patients, funnel shaped extension in and the presence of an abnormal gyral pattern in six patients (Table 2). The flag-like appearance was noted in all but patient 3.
In the eight patients in whom 3 T MRI was available, 7 T MRI depiction scored significantly better than 3 T MRI for blurring (p < 0.01), abnormalities of internal structure (p < 0.01) and demarcation of transition to normal cortex (p < 0.02) (Fig. 5) on T2 and for abnormalities of internal structure (p < 0.04) on FLAIR. Although not statistically significant, 7 T MRI tended to be superior to 3 T on another 7 out of 14 scored items (2 sequences compared, with 7 features analysed in each comparison) 3 T MRI tended to be superior to 7 T on none of the 14 items (Table 3). When combining all seven analysed characteristics on T2 and FLAIR in each individual patient, 7 T scored better than 3 T (Table 4).
Five of the six included patients that were also evaluated for epilepsy surgery were operated. In patient 3 histopathology showed a ganglioglioma WHO grade 1, patient 8 had FCD type IIIb (frontal infantile desmoplastic ganglioglioma with bordering FCD operated plus parietal FCD that we analysed in this study), patient 9 showed a FCD type IIa and patients 10 and 11 showed a FCD type IIb. The location of the lesion was congruent between MRI and surgical specimen. The 3 and 7 T MRI images of the two patients in whom the diagnosis changed from FCD to, respectively cavernoma and ganglioglioma are shown in Fig. 6.
One patient complained of profound nausea at entering the MRI. Slowing down the table movement reduced the symptoms. During the imaging this complaint was not present.
Discussion
The main finding of this study is that all observers agreed that on conventional visual analysis the lesions were easily detected and better detailed with the applied 7 T MRI protocol than on lower field strength. None of the known lesions were missed on the 7 T images. Using a semi-quantitative scale, overall our 7 T MRI protocol tended to be superior to the previously applied 3 T protocol. Statistical significance was reached for 4 out of 14 scored items. In two patients final diagnosis changed from FCD to, respectively cavernoma and gangioglioma.
As far as we know this is the first publication describing 7 T MRI in a group of patients with suspicion of FCD using a standard clinical protocol.
In one patient, due to the 7 T images diagnosis changed from FCD to cavernoma. There are several explanations possible for this change. First, due to slice thickness in the 3 T images the small hemosiderin deposit could have been located exactly in between two slices, thus escaping detection. Due to the thinner slice thickness of the 7 T images, the hemosiderin is more obvious. The images as depicted in Fig. 6 seem to substantiate this hypothesis. Second, the artefact effect of hemosiderin is more pronounced on 7 T MRI than on 3 T MRI, thereby highlighting the cavernoma more evidently in 7 T MRI. The sequence most sensitive for hemosiderin is SWI (susceptibility weighted imaging). However, in epilepsy the presence of small hemosiderin deposits is of minor relevance and therefore in the initial phase of our study this sequence was not part of our standard epilepsy protocol. This will have probably lowered the sensitivity for the detection of small haemorrhages of the 3 T MRI more than the sensitivity of 7 T MRI. Especially compared to 7 T MRI in which a T2* weighted sequence was part of the protocol. Third, there is a time delay of several months between these 3 and 7 T MRI’s. Although there were no additional clinical symptoms, it is possible that in between these time points the amount of blood surrounding the cavernoma increased. As the patient is no longer under our care we regrettably do not have access to a 3 T MRI made after the 7 T MRI.
In one of the five operated cases histopathology showed that the abnormality was a ganglioglioma instead of a FCD type II as the radiological diagnosis stated. Re-challenging of three pathologists and two radiologists with information on the opinion of the other specialist did not change their conclusions. Taking the diagnosis of the pathologists as golden standard, this proves that MRI can help giving an indication of the diagnosis. But visual inspection is not (yet) able to provide the definite diagnosis with 100 % certainty. Noteworthy is the fact that in this patient (patient 3) all evaluated MRI-characteristics of FCD were present.
The frequency of the imaging features of FCDs as seen in our study is higher than reported for FCD in the literature for 1.5 and 3 T studies. For example cortical thickening was seen in 50 % [29] to 76 % [30] whereas in our series it is 89 %. Blurring ranged from 36 % [31] to 87 % [32], whereas in our series it is 100 %. For transmantle sign this ranged from 19 % [33] to 81 % [31], and in our series it is 67 %. Most publications are based on histopathologically proven diagnoses of FCD, including patients without MRI abnormalities, whereas for our study the suspicion of a FCD on lower field strength MRI was an inclusion criterion. This explains the relative high frequency of the imaging features in our series. Quality of the 7 T MRI images itself plays a role as well: signal-to-noise ratio scales approximately linear with magnetic field strength [34, 35]. Furthermore, it has also been observed that 7 T MRI provides an increased contrast-to-noise ratio in FLAIR as compared to 1.5 and 3 T [13, 36]. The smaller voxels that can be achieved with 7 T MRI within a clinically applicable protocol will also provide better spatial resolution, leading to the detection of thin abnormalities, such as blurring or the transmantle sign.
Other limitations of the current studies include the fact that, besides the magnetic field strength, the scanners differed with respect to other hardware such as the number of receive channels of the head-coil and that choices of sequence parameters were based on local expertise without an effort to homogenize these between the field strengths. Comparisons were made between acquisitions made on the scanners available to us, which led to inherent differences in receive and transmit coil properties, other hardware components as well as software. Using, for example, a 32-channel head coil for the 3 T might have improved image quality on that field strength. However, based on our experience with both field strengths we think that magnetic field strength is the main contributor to the observed improved image quality.
Applying visual analysis, in our series 7 T MRI FLAIR was the sequence on which the lesions were most prominent. The flag-like three-layer appearance is easiest appreciated on T2. The middle hypo-intense line is accentuated by the bordering hyper-intense parts of the lesions. However, even though much less pronounced, looking at the homologue contralateral area this line often is bilaterally noticeable. The appearance of this line is not equally distributed in all different regions, which is in line with the findings of Zwanenburg et al. [37] who described similar regional differences (but no asymmetries) in the normal brain in 7 T MRI. The line is located at the grey–white matter junction and is present in almost all regions, and therefore it does not represent the striae of Gennari [38]. Based on our small series, this line seems to be more prominent with rising age, even more in the FCD-like region than in the other regions of the brain. We postulate that this line represents iron deposits which would explain an age-dependency [39]. Alternatively, this line could represent a low signal coming from the deepest cortical layer, seen on thin 7 T slices but masked on thicker 3 T slices. In 7 T MRI this accentuated three-layer appearance on the T2 weighted images has the potential to be used as an imaging marker of FCD. The internal structure and extend of the lesions were best visible on T2 and especially T2* sequences. This is in line with expectations, as the T2* sequence provides high spatial resolution and sensitivity to the magnetic susceptibility properties of tissues, thus improving evaluation of the different components within the cortex. When in more cases histopathology will become available, this might help in differentiating between different pathological substrates, like the different types of FCD.
Although due to the nature of this study we did not co-register all the sequences of 3 and 7 T study, visual inspection and interpretation support the notion that on 7 T the lesion seemed often to extend beyond what is seen on 3 T.
Because of the better delineation of lesions on 7 T, if intracranial EEG recording is needed we would advise to use the T2 sequence to guide the implantation. Especially in case of multiple depth-electrodes (stereo-EEG) where presurgical delineation of the abnormality is even more dependant on electrode placing than when using grids.
In epilepsy, abnormalities observed on MRI do not always reflect the epileptogenic focus. This is illustrated by the observation of Salmenpera et al. [40] that 9 % of 3 T MRI-positive findings are not related to the epileptogenic lesion. Therefore, every positive MRI result should be interpreted with caution and in combination with the electro clinical findings. However, clinical assessment based on the intra-individual stereotyped semiology makes it likely that all our patients had a single epileptogenic focus, correlating well with the observed location of the lesion. Interpretation of MRI should only be done including all clinical information available. This holds true for all other modalities such as PET, MEG and intracranial EEG as well. Probably, multimodality fusion will increase insight in analysing difficult surgery cases. The limitation of our study is that we included only patients with a diagnosis of FCD based on 3 or 1.5 T MRI and only three patients had a histologically proven diagnosis. Further studies will evaluate the additional value of 7 T MRI in presurgical analysis in patients without abnormalities on 3 T MRI. There is one study on the detectability of FCD’s on 7 T MRI in 21 patients without lesions on 3 or 1.5 T MRI, showing a 29 % diagnostic gain [41]. Agreement in imaging interpretation was reached through consensus-based discussions based on visual identification of structural abnormalities. Four out of the six patients with a thus detected lesion were operated, all showing a FCD on histopathology. These results are almost identical to our own results [42].
Conclusion
7 T brain imaging in vivo is feasible in epilepsy patients and can be beneficial. Lesions are well recognizable and details are better visible than at lower field strengths. The presence of typical FCD-characteristics on MRI; however, does not always reflect the final histopathological diagnosis.
Abbreviations
- EEG:
-
Electro encephalography
- FCD:
-
Focal cortical dysplasia
- FLAIR:
-
Fluid attenuated inversion recovery
- IR:
-
Inversion recovery
- MRI:
-
Magnetic resonance imaging
- PET:
-
Positron emission tomography
- SWI:
-
Susceptibility weighted imaging
- T:
-
Tesla
- TE:
-
Echo time
- TR:
-
Relaxation time
References
Cockerell OC, Johnson AL, Sander JW, Hart YM, Shorvon SD (1995) Remission of epilepsy: results from the national general practice study of epilepsy. Lancet 346:1228
Kwan P, Brodie MJ (2000) Early identification of refractory epilepsy. N Engl J Med 342(5):314–319
Kim YH, Kang HC, Kim DS, Kim SH, Shim KW, Kim HD, Lee JS (2011) Neuroimaging in identifying focal cortical dysplasia and prognostic factors in pediatric and adolescent epilepsy surgery. Epilepsia 52(4):722–727
Bien CG, Szinay M, Wagner J, Clusmann H, Becker AJ, Urbach H (2009) Characteristics and surgical outcomes of patients with refractory magnetic resonance imaging-negative epilepsies. Arch Neurol 66:1491–1499
Oster JM, Igbokwe E, Cosgrove R, Cole AJ (2012) Identifying subtle cortical gyral abnormalities as a predictor of focal cortical dysplasia and a cure for epilepsy. Arch Neurol 69(2):257–261
Rowland NC, Englot DJ, Cage TA, Sughrue ME, Barbaro NM, Chang EF (2012) A meta-analysis of predictors of seizure freedom in the surgical management of focal cortical dysplasia. J Neurosurg 116(5):1035–1041
Von Oertzen J, Urbach H, Jungbluth S, Kurthen M, Reuber M, Fernández G, Elger CE (2002) Standard magnetic resonance imaging is inadequate for patients with refractory focal epilepsy. J Neurol Neurosurg Psychiatry 73(6):643–647
Knake S, Triantafyllou C, Wald LL, Wiggins G, Kirk GP, Larsson PG et al (2005) 3 T phased array MRI improves the presurgical evaluation in focal epilepsies: a prospective study. Neurology 65:1026–1031
Phal PM, Usmanov A, Nesbit GM, Anderson JC, Spencer D, Wang P, Helwig JA, Roberts C, Hamilton BE (2008) Qualitative comparison of 3-T and 1.5-T MRI in the evaluation of epilepsy. AJR Am J Roentgenol 191(3):890–895
Strandberg M, Larsson EM, Backman S, Kallen K (2008) Pre-surgical epilepsy evaluation using 3 T MRI. Do surface coils provide additional information? Epileptic Disord 10:83–92
Mellerio C, Labeyrie MA, Chassoux F, Roca P, Alami O, Plat M, Naggara O, Devaux B, Meder JF, Oppenheim C (2014) 3 T MRI improves the detection of transmantle sign in type 2 focal cortical dysplasia. Epilepsia 55(1):117–122
Tselikas L, Souillard-Scemama R, Naggara O, Mellerio C, Varlet P, Dezamis E, Domont J, Dhermain F, Devaux B, Chrétien F, Meder JF, Pallud J, Oppenheim C (2015) Imaging of gliomas at 1.5 and 3 Tesla—a comparative study. Neuro Oncol 17(6):895–900
Li TQ, van Gelderen P, Merkle H, Talagala L, Koretsky AP, Duyn J (2006) Extensive heterogeneity in white matter intensity in high-resolution T2*-weighted MRI of the human brain at 7.0 T. Neuroimage 32(3):1032–1040
Kwan JY, Jeong SY, Van Gelderen P, Deng HX, Quezado MM, Danielian LE, Butman JA, Chen L, Bayat E, Russell J, Siddique T, Duyn JH, Rouault TA, Floeter MK (2012) Iron accumulation in deep cortical layers accounts for MRI signal abnormalities in ALS: correlating 7 Tesla MRI and pathology. PLoS One 7(4):e35241. doi:10.1371/journal.pone.0035241
Fukunaga M, Li TQ, van Gelderen P, de Zwart JA, Shmueli K, Yao B, Lee J, Maric D, Aronova MA, Zhang G, Leapman RD, Schenck JF, Merkle H, Duyn JH (2010) Layer-specific variation of iron content in cerebral cortex as a source of MRI contrast. Proc Natl Acad Sci USA 107(8):3834–3839
Conijn MM, Geerlings MI, Biessels GJ, Takahara T, Witkamp TD, Zwanenburg JJ, Luijten PR, Hendrikse J (2011) Cerebral microbleeds on MR imaging: comparison between 1.5 and 7 T. AJNR Am J Neuroradiol 32(6):1043–1049
Yao B, Bagnato F, Matsuura E, Merkle H, van Gelderen P, Cantor FK, Duyn JH (2012) Chronic multiple sclerosis lesions: characterization with high-field-strength MR imaging. Radiology 262(1):206–215
Van Veluw SJ, Zwanenburg JJ, Engelen-Lee J, Spliet WG, Hendrikse J, Luijten PR, Biessels GJ (2013) In vivo detection of cerebral cortical microinfarcts with high-resolution 7 T MRI. J Cereb Blood Flow Metab 33(3):322–329
Breyer T, Wanke I, Maderwald S, Woermann FG, Kraff O, Theysohn JM, Ebner A, Forsting M, Ladd ME, Schlamann M (2010) Imaging of patients with hippocampal sclerosis at 7 Tesla: initial results. Acad Radiol 17(4):421–426
Alexiou GA, Varely M, Sfakianos G, Prodromou N (2009) Benign lesions accompanied by intractable epilepsy in children. J Child Neurol 24(6):697–700
Piao YS, Lu DH, Chen L, Liu J, Wang W, Liu L, Yu T, Wang YP, Li YJ (2010) Neuropathological findings in intractable epilepsy: 435 Chinese cases. Brain Pathol 20(5):902–908
Tassi L, Colombo N, Garbelli R, Francione S, Lo RG, Mai R et al (2002) Focal cortical dysplasia: neuropathological subtypes, EEG, neuroimaging and surgical outcome. Brain 125:1719–1732
Krsek P, Maton B, Korman B, Pacheco-Jacome E, Jayakar P, Dunoyer C, Rey G, Morrison G, Ragheb J, Vinters HV, Resnick T, Duchowny M (2008) Different features of histopathological subtypes of pediatric focal cortical dysplasia. Ann Neurol 63(6):758–769
Abdel Razek AA, Kandell AY, Elsorogy LG, Elmongy A, Basett AA (2009) Disorders of cortical formation: MR imaging features. AJNR Am J Neuroradiol 30(1):4–11
Colombo N, Tassi L, Deleo F, Citterio A, Bramerio M, Mai R, Sartori I, Cardinale F, Lo Russo G, Spreafico R (2012) Focal cortical dysplasia type IIa and IIb: MRI aspects in 118 cases proven by histopathology. Neuroradiology 54(10):1065–1077
Blümcke I, Thom M, Aronica E, Armstrong DD, Vinters HV, Palmini A et al (2011) The clinicopathologic spectrum of focal cortical dysplasia’s: a consensus classification proposed by an ad hoc task force of the ILAE diagnostic methods commission(1). Epilepsia 52:158–174
Wezel J, Kooij BJ, Webb AG (2014) Assessing the MR compatibility of dental retainer wires at 7 Tesla. Magn Reson Med 72(4):1191–1198
Likert R (1932) A technique for the measurement of attitudes. Arch Psychol 140:1–55
Krsek P, Maton B, Jayakar P, Dean P, Korman B, Rey G, Dunoyer C, Pacheco-Jacome E, Morrison G, Ragheb J, Vinters HV, Resnick T, Duchowny M (2009) Incomplete resection of focal cortical dysplasia is the main predictor of poor postsurgical outcome. Neurology 72:217–223
Lerner JT, Salamon N, Hauptman JS et al (2009) Assessment and surgical outcomes for mild type I and severe type II cortical dysplasia: a critical review and the UCLA experience. Epilepsia 50:1310–1335
Urbach H, Scheffler B, Heinrichsmeier T et al (2002) Focal cortical dysplasia of Taylor’s balloon cell type: a clinicopathological entity with characteristic neuroimaging and histopathological features, and favorable postsurgical outcome. Epilepsia 43:33–40
Colombo N, Tassi L, Galli C et al (2003) Focal cortical dysplasias: MR imaging, histopathologic, and clinical correlations in surgically treated patients with epilepsy. AJNR Am J Neuroradiol 24:724–733
Besson P, Andermann F, Dubeau F et al (2008) Small focal cortical dysplasia lesions are located at the bottom of a deep sulcus. Brain 131:3246–3255
Van der Kolk AG, Hendrikse J, Luijten PR (2012) Ultrahigh-field magnetic resonance imaging: the clinical potential for anatomy, pathogenesis, diagnosis, and treatment planning in brain disease. Neuroimaging Clin N Am 22(2):343–362
Versluis MJ, van der Grond J, van Buchem MA, van Zijl P, Webb AG (2012) High-field imaging of neurodegenerative diseases. Neuroimaging Clin N Am 22(2):159–171
Zwanenburg JJ, Hendrikse J, Visser F, Takahara T, Luijten PR (2010) Fluid attenuated inversion recovery (FLAIR) MRI at 7.0 Tesla: comparison with 1.5 and 3.0 Tesla. Eur Radiol 20(4):915–922
Zwanenburg JJM, Hendrikse J, Luijten PR (2012) Generalized multiple-layer appearance of the cerebral cortex with 3D FLAIR 7.0-T MR imaging. Radiology 263(3):995–1001
Gennari F (1782) Francisci Gennari parmensis medicinae doctoris collegiati de peculiari structura cerebri nonnullisque eius morbis–paucae aliae anatom. Observat Accedunt, Regio Typographeo, Parma
Hagemeier J, Geurts JJ, Zivadinov R (2012) Brain iron accumulation in aging and neurodegenerative disorders. Expert Rev Neurother 12(12):1467–1480
Salmenpera TM, Symms MR, Rugg-Gunn FJ, Boulby PA, Free SL, Barker GJ, Yousry TA, Duncan JS (2007) Evaluation of quantitative magnetic resonance imaging contrasts in MRI-negative refractory focal epilepsy. Epilepsia 48(2):229–237
De Ciantis A, Barba C, Tassi L, Cosottini M, Tosetti M, Costagli M, Bramerio M, Bartolini E, Biagi L, Cossu M, Pelliccia V, Symms MR, Guerrini R (2016) 7T MRI in focal epilepsy with unrevealing conventional field strength imaging. Epilepsia. doi:10.1111/epi.13313
Colon AJ, Osch MJPv, Buijs M, Grond Jvd, Hillebrandt A, Schijns O, Ossenblok P, Hofman P, Buchem Mv, Boon P (2016) MEG-guided analysis of 7 T-MRI in patients with epilepsy. (submitted)
Acknowledgments
The authors wish to thank G.L. Wagner, neurologist and J.C. Beckervordersandforth and E. Aronica, neuropathologists, for their support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest to disclose.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Colon, A.J., van Osch, M.J.P., Buijs, M. et al. Detection superiority of 7 T MRI protocol in patients with epilepsy and suspected focal cortical dysplasia. Acta Neurol Belg 116, 259–269 (2016). https://doi.org/10.1007/s13760-016-0662-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-016-0662-x