Abstract
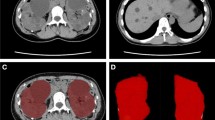
To date, there is insufficient evidence regarding use of sodium–glucose cotransporter-2 (SGLT2) inhibitors for patients with autosomal-dominant polycystic kidney disease (ADPKD), as such cases have been excluded from previous clinical trials exploring the kidney protection effects of such medications. Here, findings of an ADPKD patient who received dapagliflozin, a selective SGLT2 inhibitor, for 1 year are presented. A 38-year-old woman with a family history of ADPKD wished for treatment with dapagliflozin. After starting administration at 10 mg/day, total kidney volume (TKV) continued to increase, from 1641 to 1764 mL after 84 days and then to 2297 mL after 340 days. The estimated glomerular filtration rate (eGFR) was also decreased from 67.3 to 56.2 mL/min/1.73 m2, and then to 51.4 mL/min/1.73 m2 at those times. Immediately after discontinuation of dapagliflozin, TKV and eGFR were slightly improved to 2263 mL and 55.1 mL/min/1.73 m2, respectively. Following a review of basic research studies, we consider that increased intratubular urinary osmotic pressure, compensatory glucose reabsorption by sodium–glucose cotransporter-1 in the late proximal tubule, and hypertrophy shown in collected cells caused by increased vasopressin may be associated with ADPKD disease progression. Caution may be needed when administering dapagliflozin to patients with ADPKD.


Similar content being viewed by others
References
Torres VE, Harris PC, Pirson Y. Autosomal dominant polycystic kidney disease. Lancet. 2007;369(9569):1287–301. https://doi.org/10.1016/S0140-6736(07)60601-1.
Ong AC, Devuyst O, Knebelmann B, Walz G, Diseases E-EWGfIK. Autosomal dominant polycystic kidney disease: the changing face of clinical management. Lancet. 2015;385(9981):1993–2002. https://doi.org/10.1016/S0140-6736(15)60907-2.
Dachy A, Decuypere JP, Vennekens R, Jouret F, Mekahli D. Is autosomal dominant polycystic kidney disease an early sweet disease? Pediatr Nephrol. 2022;37(9):1945–55. https://doi.org/10.1007/s00467-021-05406-z.
Nowak KL, Hopp K. Metabolic reprogramming in autosomal dominant polycystic kidney disease: evidence and therapeutic potential. Clin J Am Soc Nephrol. 2020;15(4):577–84. https://doi.org/10.2215/CJN.13291019.
Warner G, Hein KZ, Nin V, Edwards M, Chini CC, Hopp K, et al. Food restriction ameliorates the development of polycystic kidney disease. J Am Soc Nephrol. 2016;27(5):1437–47. https://doi.org/10.1681/ASN.2015020132.
Kipp KR, Rezaei M, Lin L, Dewey EC, Weimbs T. A mild reduction of food intake slows disease progression in an orthologous mouse model of polycystic kidney disease. Am J Physiol Renal Physiol. 2016;310(8):F726–31. https://doi.org/10.1152/ajprenal.00551.2015.
Torres JA, Kruger S, Broderick C, Amarlkhagva T, Agrawal S, Dodam JR, et al. Ketosis ameliorates renal cyst growth in polycystic kidney disease. Cell Metab. 2019;30(6):1007–23. https://doi.org/10.1016/j.cmet.2019.09.012.
Nowak KL, Steele C, Gitomer B, Wang W, Ouyang J, Chonchol MB. Overweight and obesity and progression of ADPKD. Clin J Am Soc Nephrol. 2021;16(6):908–15. https://doi.org/10.2215/CJN.16871020.
Hopp K, Catenacci VA, Dwivedi N, Kline TL, Wang W, You Z, et al. Weight loss and cystic disease progression in autosomal dominant polycystic kidney disease. iScience. 2022;25(1):103697. https://doi.org/10.1016/j.isci.2021.103697.
Heerspink HJL, Stefansson BV, Correa-Rotter R, Chertow GM, Greene T, Hou FF, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383(15):1436–46. https://doi.org/10.1056/NEJMoa2024816.
The E-KCG, Herrington WG, Staplin N, Wanner C, Green JB, Hauske SJ, et al. Empagliflozin in patients with chronic kidney disease. N Engl J Med. 2023;388(2):117–27. https://doi.org/10.1056/NEJMoa2204233.
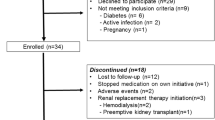
Morioka F, Nakatani S, Uedono H, Tsuda A, Mori K, Emoto M. Short-term dapagliflozin administration in autosomal dominant polycystic kidney disease—a retrospective single-arm case series study. J Clin Med. 2023;12(19):6341. https://doi.org/10.3390/jcm12196341.
Irazabal MV, Rangel LJ, Bergstralh EJ, Osborn SL, Harmon AJ, Sundsbak JL, et al. Imaging classification of autosomal dominant polycystic kidney disease: a simple model for selecting patients for clinical trials. J Am Soc Nephrol. 2015;26(1):160–72. https://doi.org/10.1681/ASN.2013101138.
Kapoor S, Rodriguez D, Riwanto M, Edenhofer I, Segerer S, Mitchell K, et al. Effect of sodium-glucose cotransport inhibition on polycystic kidney disease progression in PCK rats. PLoS ONE. 2015;10(4): e0125603. https://doi.org/10.1371/journal.pone.0125603.
Li SR, Gulieva RE, Helms L, Cruz NM, Vincent T, Fu H, et al. Glucose absorption drives cystogenesis in a human organoid-on-chip model of polycystic kidney disease. Nat Commun. 2022;13(1):7918. https://doi.org/10.1038/s41467-022-35537-2.
Devuyst O, Chapman AB, Gansevoort RT, Higashihara E, Perrone RD, Torres VE, et al. Urine osmolality, response to tolvaptan, and outcome in autosomal dominant polycystic kidney disease: results from the TEMPO 3:4 trial. J Am Soc Nephrol. 2017;28(5):1592–602. https://doi.org/10.1681/ASN.2016040448.
Wang X, Zhang S, Liu Y, Spichtig D, Kapoor S, Koepsell H, et al. Targeting of sodium-glucose cotransporters with phlorizin inhibits polycystic kidney disease progression in Han:SPRD rats. Kidney Int. 2013;84(5):962–8. https://doi.org/10.1038/ki.2013.199.
Neumiller JJ, White JR Jr, Campbell RK. Sodium-glucose co-transport inhibitors: progress and therapeutic potential in type 2 diabetes mellitus. Drugs. 2010;70(4):377–85. https://doi.org/10.2165/11318680-000000000-00000.
Rieg T, Masuda T, Gerasimova M, Mayoux E, Platt K, Powell DR, et al. Increase in SGLT1-mediated transport explains renal glucose reabsorption during genetic and pharmacological SGLT2 inhibition in euglycemia. Am J Physiol Renal Physiol. 2014;306(2):F188–93. https://doi.org/10.1152/ajprenal.00518.2013.
Sinha F, Federlein A, Biesold A, Schwarzfischer M, Krieger K, Schweda F, et al. Empagliflozin increases kidney weight due to increased cell size in the proximal tubule S3 segment and the collecting duct. Front Pharmacol. 2023;14:1118358. https://doi.org/10.3389/fphar.2023.1118358.
Wang X, Wu Y, Ward CJ, Harris PC, Torres VE. Vasopressin directly regulates cyst growth in polycystic kidney disease. J Am Soc Nephrol. 2008;19(1):102–8. https://doi.org/10.1681/ASN.2007060688.
Watanabe S, Sawa N, Mizuno H, Yamanouchi M, Suwabe T, Hoshino J, et al. Development of osmotic vacuolization of proximal tubular epithelial cells following treatment with sodium-glucose transport protein 2 inhibitors in type II diabetes mellitus patients-3 case reports. CEN Case Rep. 2021;10(4):563–9. https://doi.org/10.1007/s13730-021-00609-7.
Ferrannini G, Hach T, Crowe S, Sanghvi A, Hall KD, Ferrannini E. Energy balance after sodium-glucose cotransporter 2 inhibition. Diabetes Care. 2015;38(9):1730–5. https://doi.org/10.2337/dc15-0355.
Perkins BA, Cherney DZ, Partridge H, Soleymanlou N, Tschirhart H, Zinman B, et al. Sodium-glucose cotransporter 2 inhibition and glycemic control in type 1 diabetes: results of an 8-week open-label proof-of-concept trial. Diabetes Care. 2014;37(5):1480–3. https://doi.org/10.2337/dc13-2338.
Takata T, Isomoto H. Pleiotropic effects of sodium-glucose cotransporter-2 inhibitors: renoprotective mechanisms beyond glycemic control. Int J Mol Sci. 2021;22(9):4374. https://doi.org/10.3390/ijms22094374.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have conflicts of interests to declare in regard to dapagliflozin. Regarding SGLT2 inhibitors other than dapagliflozin, KM has received honorariums for lecturing from Mitsubishi Tanabe Pharma Corporation, AstraZeneca K.K., and Nippon Boehringer Ingelheim. KM and ME have received research funding from Tanabe Pharma Corporation.
Ethical approval
This article does not contain results of any studies with human participants or animals performed by any of the authors.
Informed consent
Written informed consent was obtained from the patient for publication of her clinical data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Nakatani, S., Morioka, F., Uedono, H. et al. Dapagliflozin administration for 1 year promoted kidney enlargement in patient with ADPKD. CEN Case Rep (2023). https://doi.org/10.1007/s13730-023-00840-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13730-023-00840-4