Abstract
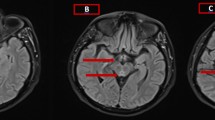
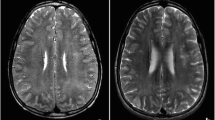
Wernicke encephalopathy (WE) resulting from vitamin B1 (VB1) deficiency is commonly regarded as being associated with a high alcohol intake; however, recently many non-alcohol-related cases have been reported. Herein, we report a case of WE due to VB1 deficiency in the early stage after the start of hemodialysis. The patient was a 79-year-old male recommended for hemodialysis due to chronic renal failure. He was admitted to our hospital due to a hemorrhagic duodenal ulcer, but hemodialysis was started as the result of exacerbation of renal function. After the start of 3-times-weekly hemodialysis, the patient’s general condition was settled and he was able to consume about half his usual dietary intake. Seventeen days after the start of hemodialysis, impaired consciousness and involuntary movements appeared, and subsequent head magnetic resonance imaging showed increased signal intensity around the cerebral aqueduct. VB1 administration based on a suspicion of WE resulted in a significant improvement in neurological symptoms and no sequelae were observed. Hemodialysis may be a risk factor for VB1 deficiency. When a dialysis patient presents with psychiatric symptoms or impaired consciousness, in particular, it is important to always keep the possibility of VB1 deficiency in mind.

Similar content being viewed by others
Availability of data and materials
Not applicable.
Abbreviations
- WE:
-
Wernicke encephalopathy
- MRI:
-
Magnetic resonance imaging
- VB1:
-
Vitamin B1
- FLAIR:
-
Axial Fluid Attenuated Inversion Recovery
References
Sechi G, Batzu L, Agro L, Fois C. Cancer-related Wernicke-Korsakoff syndrome. Lancet Oncol. 2016;17(6):e221–2. https://doi.org/10.1016/s1470-2045(16)30109-7.
MacLean LD, Rhode BM, Shizgal HM. Nutrition following gastric operations for morbid obesity. Ann Surg. 1983;198(3):347–55.
Sechi G, Sechi E, Fois C, Kumar N. Advances in clinical determinants and neurological manifestations of B vitamin deficiency in adults. Nutr Rev. 2016;74(5):281–300. https://doi.org/10.1093/nutrit/nuv107.
Onishi H, Ishida M, Toyama H, Tanahashi I, Ikebuchi K, Taji Y, et al. Early detection and successful treatment of Wernicke encephalopathy in a patient with advanced carcinoma of the external genitalia during chemotherapy. Palliat Support Care. 2016;14(3):302–6. https://doi.org/10.1017/s1478951515000875.
Isenberg-Grzeda E, Kutner HE, Nicolson SE. Wernicke-Korsakoff-syndrome: under-recognized and under-treated. Psychosomatics. 2012;53(6):507–16. https://doi.org/10.1016/j.psym.2012.04.008.
Isenberg-Grzeda E, Rahane S, DeRosa AP, Ellis J, Nicolson SE. Wernicke-Korsakoff syndrome in patients with cancer: a systematic review. Lancet Oncol. 2016;17(4):e142–8. https://doi.org/10.1016/s1470-2045(16)00037-1.
Onishi H, Sato I, Uchida N, Takahashi T, Furuya D, Ebihara Y, et al. High proportion of thiamine deficiency in referred cancer patients with delirium: a retrospective descriptive study. Eur J Clin Nutr. 2021;75(10):1499–505. https://doi.org/10.1038/s41430-021-00859-9.
Sechi G, Serra A. Wernicke’s encephalopathy: new clinical settings and recent advances in diagnosis and management. Lancet Neurol. 2007;6(5):442–55. https://doi.org/10.1016/S1474-4422(07)70104-7.
Onishi H, Ishida M, Uchida N, Shintani D, Nishikawa T, Hasegawa K, et al. Subclinical thiamine deficiency identified by preoperative evaluation in an ovarian cancer patient: Diagnosis and the need for preoperative thiamine measurement. Palliat Support Care. 2019;17(5):609–10. https://doi.org/10.1017/s1478951518000615.
Sica DA. Loop diuretic therapy, thiamine balance, and heart failure. Congest Heart Fail. 2007;13(4):244–7. https://doi.org/10.1111/j.1527-5299.2007.06260.x.
Uchida N, Ishida M, Sato I, Takahashi T, Furuya D, Ebihara Y, et al. Exacerbation of psychotic symptoms as clinical presentation of Wernicke encephalopathy in an Alzheimer’s disease patient. J Gen Fam Med. 2020;21(5):185–7. https://doi.org/10.1002/jgf2.330.
Hung SC, Hung SH, Tarng DC, Yang WC, Chen TW, Huang TP. Thiamine deficiency and unexplained encephalopathy in hemodialysis and peritoneal dialysis patients. Am J Kidney Dis. 2001;38(5):941–7. https://doi.org/10.1053/ajkd.2001.28578.
Ueda K, Takada D, Mii A, Tsuzuku Y, Saito SK, Kaneko T, et al. Severe thiamine deficiency resulted in Wernicke’s encephalopathy in a chronic dialysis patient. Clin Exp Nephrol. 2006;10(4):290–3. https://doi.org/10.1007/s10157-006-0440-9.
Stegmayr B. Dialysis procedures alter metabolic conditions. Nutrients. 2017. https://doi.org/10.3390/nu9060548.
Ihara M, Ito T, Yanagihara C, Nishimura Y. Wernicke’s encephalopathy associated with hemodialysis: report of two cases and review of the literature. Clin Neurol Neurosurg. 1999;101(2):118–21. https://doi.org/10.1016/s0303-8467(99)00014-1.
Jankowska M, Rudnicki-Velasquez P, Storoniak H, Rutkowski P, Rutkowski B, Krzymiński K, et al. Thiamine diphosphate status and dialysis-related losses in end-stage kidney disease patients treated with hemodialysis. Blood Purif. 2017;44(4):294–300. https://doi.org/10.1159/000480651.
Uruha A, Shimizu T, Katoh T, Yamasaki Y, Matsubara S. Wernicke’s encephalopathy in a patient with peptic ulcer disease. Case Rep Med. 2011;2011: 156104. https://doi.org/10.1155/2011/156104.
Nakano O, Tsuchiya A, Yamagiwa S, Terai S. Stomach dysfunction is a potential risk factor for wernicke’s encephalopathy. Intern Med. 2016;55(24):3679–80. https://doi.org/10.2169/internalmedicine.55.7483.
Oudman E, Wijnia JW, Oey MJ, van Dam M, Postma A. Wernicke’s encephalopathy in Crohn’s disease and ulcerative colitis. Nutrition (Burbank, Los Angeles County, Calif). 2021;86: 111182. https://doi.org/10.1016/j.nut.2021.111182.
Lopez RI, Collins GH. Wernicke’s encephalopathy. A complication of chronic hemodialysis. Arch Neurol. 1968;18(3):248–59. https://doi.org/10.1001/archneur.1968.00470330038003.
Faris AA. Wernicke’s encephalopathy in uremia. Neurology. 1972;22(12):1293–7. https://doi.org/10.1212/wnl.22.12.1293.
Jagadha V, Deck JH, Halliday WC, Smyth HS. Wernicke’s encephalopathy in patients on peritoneal dialysis or hemodialysis. Ann Neurol. 1987;21(1):78–84. https://doi.org/10.1002/ana.410210114.
Descombes E, Dessibourg CA, Fellay G. Acute encephalopathy due to thiamine deficiency (Wernicke’s encephalopathy) in a chronic hemodialyzed patient: a case report. Clin Nephrol. 1991;35(4):171–5.
Ookawara S, Suzuki M, Saitou M. Acute encephalopathy due to thiamine deficiency with hyperammonemia in a chronic hemodialysis patient: a case report. Nihon Jinzo Gakkai Shi. 2003;45(4):393–7.
Kinashi H, Yoshioka T, Urahama Y, Iida Y, Masamoto D, Nishimura H, et al. A case of Wernicke’s encephalopathy associated with the introduction of hemodialysis. Nihon Toseki Igakkai Zasshi. 2009;42(5):379–85. https://doi.org/10.4009/jsdt.42.379.
Nakatani-Enomoto S, Moriya A, Kikuchi S, Mochizuki H, Sugiura Y, Ugawa Y. Wernicke encephalopathy in a non-alcoholic patient with diabetic nephropathy under hemodialysis. Rinsho Shinkeigaku. 2010;50(6):409–11. https://doi.org/10.5692/clinicalneurol.50.409.
Kimura H, Takeda K, Muto Y, Mukai H, Furusho M, Nakashita S, et al. Development of Wernicke’s encephalopathy during initiation of hemodialysis in an elderly non-alcoholic patient. Clin Nephrol. 2012;78(6):487–91. https://doi.org/10.5414/cn107182.
Ubukata M, Amemiya N, Nitta K, Takei T. Wernicke’s encephalopathy during long-term hemodialysis manifesting as disturbance of consciousness. Nihon Toseki Igakkai Zasshi. 2014;47(3):217–22. https://doi.org/10.4009/jsdt.47.217.
Ota Y, Capizzano AA, Moritani T, Naganawa S, Kurokawa R, Srinivasan A. Comprehensive review of Wernicke encephalopathy: pathophysiology, clinical symptoms and imaging findings. Jpn J Radiol. 2020;38(9):809–20. https://doi.org/10.1007/s11604-020-00989-3.
Antunez E, Estruch R, Cardenal C, Nicolas JM, Fernandez-Sola J, Urbano-Marquez A. Usefulness of CT and MR imaging in the diagnosis of acute Wernicke’s encephalopathy. AJR Am J Roentgenol. 1998;171(4):1131–7. https://doi.org/10.2214/ajr.171.4.9763009.
Oudman E, Wijnia JW, Oey MJ, van Dam M, Postma A. Wernicke-Korsakoff syndrome despite no alcohol abuse: a summary of systematic reports. J Neurol Sci. 2021;426: 117482. https://doi.org/10.1016/j.jns.2021.117482.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
NS, TH, and NU were involved in drafting the manuscript. MI and HO did critical revision. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Seto, N., Ishida, M., Hamano, T. et al. A case of Wernicke encephalopathy arising in the early stage after the start of hemodialysis. CEN Case Rep 11, 314–320 (2022). https://doi.org/10.1007/s13730-021-00669-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13730-021-00669-9