Abstract
Emphysematous pyelonephritis (EPN) is a necrotizing gas producing infection of the renal parenchyma that commonly occurs in patients with diabetes. EPN requires early diagnosis and treatment due to the possible life-threatening septic complications. We report a rare case of EPN caused by an unfavorable mixed infection of Candida parapsilosis and Finegoldia magna. To our knowledge, this is the first reported case of EPN caused by Finegoldia magna. A 62-year-old male with diabetes mellitus (DM) presented with abdominal pain, shortness of breath, and nausea in which a diagnosis of septic shock was made due to EPN. Our patient first noticed abdominal pain 3 weeks prior to hospital presentation; however, he avoided getting treatment due to a fear of contracting severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This patient exhibited deterioration and expired after surgical intervention despite uneventful nephrectomy. This case suggests that medical care avoidance behaviors among patients could potentially complicate their clinical course.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Emphysematous pyelonephritis (EPN) is a severe necrotizing infection that results in gas production in the renal parenchyma, collecting system, and perinephric tissue [1]. Gram-negative bacteria, such as Escheria coli and Klebsiella, are the most common causative pathogens of EPN [1]. Type 2 DM is the most common associated factor, followed by obstructive uropathy [2]. Up to 90% of all cases of EPN occur in patients with uncontrolled diabetes mellitus [3]. Computed Tomography (CT) is recommended for the evaluation of this disease and early nephrectomy is considered the treatment of choice, especially if a patient has a poor prognosis [1]. If not recognized and treated promptly, the clinical course of EPN can be life-threatening.
A recent phenomenon of medical care avoidance among patients with life threatening illnesses, due to a fear of contracting coronavirus disease 2019 (COVID-19) during their hospital stay, is associated with misconceptions regarding disease severity and modes of viral transmission [4]. Fear is a well-known determinant of medical care avoidance and leads to devastating clinical outcomes, due to the requirement of radical treatments and longer hospital stays, which further stresses the medical system resulting in increased healthcare costs [5]. Currently, the COVID‐19 pandemic is the largest threat facing healthcare systems worldwide. In urological fields, it is recommended that all elective surgeries be deferred in regions with a large number of COVID‐19 cases [6]. However, surgical intervention must be considered for urological emergencies, including EPN [7]. There is a lack of papers illustrating how healthcare avoidance among urology patients, during the COVID-19 pandemic, has impacted their healthcare outcomes. We herein describe the case of a 62-year-old male who delayed treatment for EPN, caused by Candida parapsilosis and Finegoldia magna, due to a fear of contracting COVID-19 at the hospital. The patient unfortunately passed away from a cardiopulmonary arrest due to medical co-morbid conditions, severe sepsis, and hemodynamic instability. We hypothesize that delayed treatment, due to avoidance behaviors, may contribute to higher mortality rates in urological patients with EPN.
Case presentation
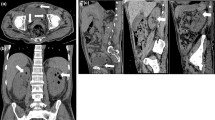
An ill appearing 62-year-old male was admitted to the emergency department (ED) with shortness of breath, chest pain, confusion, abdominal pain, and nausea. Per emergency medical services, the patient’s wife called 911 as she noticed a gradual change in his mental status. Onset of abdominal pain was 3 weeks prior to ED presentation; delay in care was secondary to fear of contracting severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), per patient. The patient’s past medical history is significant for type 2 DM, morbid obesity, chronic obstructive pulmonary disease, hiatal hernia, kidney stones, and benign prostatic hypertrophy. The Patient was febrile, hypotensive, and tachypneic on arrival. Patient’s presentation was consistent with sepsis and a CT scan revealed gas and fluid collection in the right retroperitoneum (Figs. 1 and 2). Significant labs on admission included leukocytosis of 49.3 (10^9/L), platelets elevated to 709 (10^9/L), acute kidney injury with a creatinine level of 3.92 (pg/L), glucose of 70 (mmol/L), hemoglobin A1c of 5.6%, and lactate was elevated to 6.8 (mmol/L). Patient was given two liters of lactated Ringers solution for hypotension and two units packed red blood cells. Vancomycin and piperacillin-tazobactam were started for presumed sepsis. Patient was then taken to the operating room (OR) for an exploratory laparotomy, right nephrectomy, and debridement of necrotizing infection of the retroperitoneum. This surgery revealed pus in the right collecting system and a non-salvageable right kidney that was necrotic and mottled in appearance. The necrotizing soft-tissue infection of the right retroperitoneum was removed along with the necrotic peri-renal tissue. Urinalysis was positive for Candida parapsilosis and the initial OR culture grew Finegoldia magna. Histopathology findings demonstrated acute pyelonephritis with polymorphonuclear cells, chronic inflammation, and areas of necrosis with abscess formation extending into the right kidney parenchyma and perinephric adipose tissue (Figs. 3, 4, 5). He developed acute kidney injury requiring continuous renal replacement therapy. His hospital course was then complicated by recurrent episodes of upper gastrointestinal bleeding not amenable to endoscopic treatment or embolization by interventional radiology. The patient subsequently experienced an acute mental status change, desaturation on the ventilator, and increased pressor requirement with heavy sanguineous output from his rectal and nasogastric tubes. The patient was compassionately extubated, made comfortable and soon expired.
Discussion
Potential etiologies that have been postulated to underlie the pathogenesis of EPN include high glucose concentrations in tissues, tissue ischemia, impaired immunity, and gas-forming bacteria [1]. A high level of glucose in tissues together with decreased blood flow to the kidneys, which is prevalent in patients with diabetes mellitus, facilitates the production of gas via the fermentation of glucose and lactate [3]. While diabetes is the most common predisposing factor for EPN, it has not been associated with increased mortality [2]. Other common risk factors for developing EPN includes urinary tract obstruction, immunosuppression, and end stage renal disease. A patient with a urinary tract obstruction has a 25–40% chance of developing secondary EPN [1]. Our patient was not at an increased risk for developing EPN as his DM was in control and imaging did not show any evidence of kidney stones. Upon admission to the ED, his glucose and hemoglobin A1c levels were normal at 70 (mmol/L) and 5.6%, respectively. A few months prior to developing EPN, the patient underwent ureteroscopy and stone manipulation and there was no evidence of remaining stones after the procedure and upon admission to the ED. The delay in care is what made this patient’s infection a true emergency. A meta‐analysis of the risk factors affecting the mortality rate among patients with EPN concluded that a systolic blood pressure less than 90 mmHg, thrombocytopenia, impaired consciousness, and increased serum creatinine levels are associated with higher mortality [2]. Our patient had most of the factors mentioned above including hypotension, impaired consciousness, and increased creatinine levels upon arrival to the ED.
Escherichia coli remains the most common causative pathogen of EPN, but there are also reports of Proteus mirabilis, Klebsiella pneumonia, Group D Streptococcus and coagulase-negative Staphylococcus as being causative agents [1]. This case describes a unique clinical manifestation of EPN caused by an unfavorable mixed infection of Candida parapsilosis and Finegoldia magna. To date, there is only one reported case of EPN caused by Candida parapsilosis and there are no cases of EPN caused by Finegoldia magna reported in the literature [8]. Fungal etiology has rarely been reported for EPN and usually responds well with antifungal treatment [8]. Finegoldia magna is an opportunistic anaerobic gram positive cocci and is found in the normal flora of the gastrointestinal and genitourinary tract [9]. This bacteria is implicated in a range of infections including urinary tract infections, necrotizing pneumonia, infective endocarditis, and meningitis [9]. Finegoldia magna, and other anaerobic bacteria, are well known as gas-producing pathogens. Certain Candida species, including Candida parapsilosis, are known to produce gas in vitro. Candida parapsilosis has been detected in the laboratory, via a positive sugar fermentation test, to produce acid and gas in a test tube [10]. A rare etiology, such as Candida parapsilosis and Finegoldia magna, should be considered as causative organisms when evaluating a case of EPN. The management of EPN consists of both surgical and medical treatment. Traditionally, early nephrectomy has been considered the treatment of choice in EPN and is to be considered if a patient has a poor prognosis, several risk factors, or does not improve on conservative treatment [11]. Our patient received Vancomycin, Ceftriaxone, Amikacin, and Micafungin to cover the unusual strains of bacteria and fungi causing this infection.
The dramatic presentation and significant complications seen in this patient may have been reduced by an earlier admittance to the ED. The patient reported that he first noticed abdominal pain 3 weeks prior to admittance to the hospital; however, his fear kept him from coming in. With a significant history of prior kidney stones and stone removal, the patient has experienced similar flank pain in the past but chose to ignore his new onset of symptoms. The severe symptoms of EPN, such as shortness of breath and confusion, appeared one day prior to admission. The initial symptoms of abdominal pain and fevers were ignored and the patient was finally brought to the hospital, once his wife called 911, secondary to an altered mental status and shortness of breath. The COVID-19 pandemic has received immense news coverage and has emphasized social distancing as well as avoiding places, where the virus could be easily spread among individuals, including hospitals. As shown in our patient’s case, the emphasis placed on staying home and vigilance for viral transmission encourages medical care avoidance and leads to dire clinical outcomes. Urologists can play a unique role during the COVID-19 pandemic by educating patients, especially those who are more at risk of developing EPN, on how to recognize the signs and symptoms as well as the importance of an early diagnosis.
Conclusion
EPN, while commonly caused by uropathogens, is a fatal infection that may be caused by uncommon etiological agents such as Candida parapsilosis and Finegoldia magna. EPN is commonly seen in diabetic patients and CT scan is the most effective tool for an early diagnosis. Physicians and health care providers need to address the public fear of contracting COVID-19 in the hospital, as well as the confusion regarding symptomology of fatal infections such as EPN, to eliminate the phenomenon of medical care avoidance among patients.
References
Ubee SS, McGlynn L, Fordham M. Emphysematous pyelonephritis. BJU Int. 2011. https://doi.org/10.1111/j.1464-410X.2010.09660.x.
Falagas ME, Alexiou VG, Giannopoulou KP, Siempos II. Risk factors for mortality in patients with emphysematous pyelonephritis: a meta-analysis. J Urol. 2007. https://doi.org/10.1016/j.juro.2007.05.017.
Smitherman KO, Peacock JE. Infectious emergencies in patients with diabetes mellitus. Med Clin North Am. 1995. https://doi.org/10.1016/S0025-7125(16)30084-0.
Lau JTF, Griffiths S, Choi KC, Tsui HY. Avoidance behaviors and negative psychological responses in the general population in the initial stage of the H1N1 pandemic in Hong Kong. BMC Infect Dis. 2010. https://doi.org/10.1186/1471-2334-10-139.
Kannan VD, Veazie PJ. Predictors of avoiding medical care and reasons for avoidance behavior. Med Care. 2014. https://doi.org/10.1097/MLR.0000000000000100.
Goldman HB, Haber GP. Recommendations for tiered stratification of urological surgery urgency in the COVID-19 Era. J Urol. 2020. https://doi.org/10.1097/ju.0000000000001067.
Puliatti S, Eissa A, Eissa R, et al. COVID-19 and urology: a comprehensive review of the literature. BJU Int. 2020. https://doi.org/10.1111/bju.15071.
Bhat RA, Bashir G, Wani M, Lone S. Emphysematous pyelonephritis caused by Candida parapsilosis: An unknown etiological agent. N Am J Med Sci. 2012. https://doi.org/10.4103/1947-2714.99521.
Badri M, Nilson B, Ragnarsson S, Senneby E, Rasmussen M. Clinical and microbiological features of bacteraemia with Gram-positive anaerobic cocci: a population-based retrospective study. Clin Microbiol Infect. 2019. https://doi.org/10.1016/j.cmi.2018.09.001.
Milne LJR. Fungi. In: Collee J, Fraser AG, Marmion BP, editors. Mackie and Mc Cartney practical medical microbiology. 14th ed. New York: Churchill Livingstone; 1996. p. 702–703.
Wang Q, Sun M, Ma C, et al. Emphysematous pyelonephritis and cystitis in a patient with uremia and anuria: a case report and literature review. Medicine (United States). 2018. https://doi.org/10.1097/MD.0000000000011272.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Krol, B.C., Hemal, A.K., Fenu, E.M. et al. A rare case of emphysematous pyelonephritis caused by Candida parapsilosis and Finegoldia magna complicated by medical care avoidance. CEN Case Rep 10, 111–114 (2021). https://doi.org/10.1007/s13730-020-00531-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13730-020-00531-4