Abstract
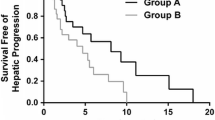
Hepatic arterial infusion chemotherapy (HAIC) for liver metastases (LMs) from breast cancer is not a standard of care, but its effectiveness in patients with extensive LMs who cannot tolerate systemic therapy has been reported. Herein, we report a case of breast cancer LMs that were controlled by anthracycline-based HAIC. A 46-year-old woman with estrogen receptor-positive, human epidermal growth factor receptor 2-negative metastatic breast cancer who had multiple LMs and bone metastases underwent seven lines of systemic therapy (paclitaxel/bevacizumab for 38 months; letrozole, nivolumab/fulvestrant, eribulin, gemcitabine/vinorelbine, high-dose toremifene/abemaciclib, and capecitabine for 21 months in total). However, owing to its adverse effects and the continued progression of the LMs, systemic therapy was switched to HAIC (40 mg/body epirubicin on day 1, 4 mg/body mitomycin C on days 1 and 15, and 500 mg/body 5-fluorouracil on days 1, 8, and 15; 28-day courses). In response to HAIC, the LMs remarkably regressed and were controlled for 17 months without severe adverse effects. HAIC was stopped when multiple brain metastases arose, and the patient died 2 months later. This case suggests that HAIC is a reasonable option for patients with extensive LMs, even in the late stage of treatment. HAIC recipients should be carefully selected through multidisciplinary discussions as the survival benefits of HAIC over systemic treatment remain unclear. Our findings identify a potential window for the use of traditional chemotherapeutic agents such as anthracyclines. Novel strategies to improve drug delivery are warranted in the future.




Similar content being viewed by others
Data availability
All data related to this report are available from the corresponding author upon reasonable request.
References
Camacho LH, Kurzrock R, Cheung A et al (2007) Pilot study of regional, hepatic intra-arterial paclitaxel in patients with breast carcinoma metastatic to the liver. Cancer 109:2190–2196
Arai Y, Sone Y, Inaba AY, Kido C (1994) Hepatic arterial infusion chemotherapy for liver metastases from breast cancer. Cancer Chemother Pharmacol 33(Suppl):S142–S144
Aarts BM, Muñoz FMG, Wildiers H et al (2021) Intra-arterial therapies for liver metastatic breast cancer: a systematic review and meta-analysis. Cardiovasc Intervent Radiol 44:1868–1882
Masuda T, Niizeki O, Niizeki T et al (2021) Successful treatment with hepatic arterial infusion chemotherapy in a breast cancer patient with multiple liver metastases who declined systemic therapy. Case Rep Oncol 14:1261–1265
Gofuku J, Yayoi E, Ikeda N et al (2004) Long-term survivors with liver metastasis from breast cancer who were received intra-arterial chemotherapy. Gan To Kagaku Ryoho 31:1828–1831
Furuta M, Watanabe J, Aramaki T, Notsu A, Yasui H (2020) Hepatic arterial infusion chemotherapy for metastatic breast cancer patients with resistance to standard systemic chemotherapies. In Vivo 34:275–2782
Hsiao JH, Chang HT, Tseng YD et al (2018) Hepatic arterial infusion chemotherapy is a feasible treatment option for breast cancer with liver-predominant metastatic disease. In Vivo 32:1635–1641
Tewes M, Peis MW, Bogner S et al (2017) Hepatic arterial infusion chemotherapy for extensive liver metastases of breast cancer: efficacy, safety and prognostic parameters. J Cancer Res Clin Oncol 143:2131–2141
Ikeda T, Adachi I, Takashima S et al (1999) A phase I/II study of continuous intra-arterial chemotherapy using an implantable reservoir for the treatment of liver metastases from breast cancer: a Japan Clinical Oncology Group (JCOG) study 9113. Jpn J Clin Oncol 29:23–27
Tekin K, Kocaoglu H, Bayar S (2002) Long-term survival after regional chemotherapy for liver metastases from breast cancer. A case report. Tumori 88:167–169
Ueshima K, Komemushi A, Aramaki T et al (2022) Clinical practice guidelines for hepatic arterial infusion chemotherapy with a port system proposed by the Japanese Society of Interventional Radiology and Japanese Society of Implantable Port Assisted Treatment. Liver Cancer 11:407–425
Wang M, Zhang J, Ji S et al (2017) Transarterial chemoembolisation for breast cancer with liver metastasis: a systematic review. Breast 36:25–30
Yin T, Nie L, Wu D et al (2020) Chemotherapy for breast cancer progresses to liver metastases after surgery and systemic treatment. Transl Cancer Res 9:993–1000
Holte D, Lyssikatos JP, Valdiosera AM et al (2020) Evaluation of PNU-159682 antibody drug conjugates (ADCs). Bioorg Med Chem Lett 30:127640
Joubert N, Beck A, Dumontet C, Denevault-Sabourin C (2020) Antibody-drug conjugates: the last decade. Pharmaceuticals (Basel) 13:245
Ang C, Jhaveri K, Patel D et al (2013) Hepatic arterial infusion and systemic chemotherapy for breast cancer liver metastases. Breast J 19:96–99
Tsimberidou AM, Moulder S, Fu S et al (2010) Phase I clinical trial of hepatic arterial infusion of cisplatin in combination with intravenous liposomal doxorubicin in patients with advanced cancer and dominant liver involvement. Cancer Chemother Pharmacol 66:1087–1093
Shi HB, Qiang WG, Zhu WL et al (2021) Hepatic artery infusion pump combined with systemic chemotherapy for patients with liver metastases from breast carcinoma. Technol Cancer Res Treat 20:15330338211051552
Fountzilas E, Krishnan E, Janku F et al (2018) A phase I clinical trial of hepatic arterial infusion of oxaliplatin and oral capecitabine, with or without intravenous bevacizumab, in patients with advanced cancer and predominant liver involvement. Cancer Chemother Pharmacol 82:877–885
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Masahiro Kawashima received a research grant from Nippon Kayaku Co. Ltd. and Kyowa Kirin Co. Ltd. Masahiro Kawashima received lecture fees from Pfizer Inc., Daiichi Sankyo Co. Ltd., Guardant Health Amea Inc., Eisai Co. Ltd., and Chugai Pharmaceutical Co. Ltd.
Ethical approval
Ethics committee approval was waived due to the nature of case report.
Informed consent
Informed consent was obtained from the patient included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Kawashima, M., Matsumoto, T., Nishimura, T. et al. Anthracycline-based hepatic arterial infusion chemotherapy achieved 17 months of disease regression in a patient with breast cancer liver metastases resistant to multiple systemic chemotherapies. Int Canc Conf J 13, 153–157 (2024). https://doi.org/10.1007/s13691-024-00656-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13691-024-00656-8