Abstract
Purpose of Review
As the presence of valvular heart disease increases with age and women have a longer life-expectancy than men, gender disparities for patients with valvular heart disease (VHD) are exacerbated in the aging population. In this article, we review the differences in presentation, pathophysiology, treatment, and outcomes between men and women with VHD and examine available data as to how these differences may impact the aging population.
Recent Findings
Available data demonstrate significant gender-related differences in clinical presentation, treatment, and outcomes for patients with valvular heart disease (VHD). It is also well-established that men and women exhibit different risk profiles which leads to a significant impact on treatment outcomes. Women tend to be under-referred, often present for delayed treatment, and are under-represented in most large-scale clinical trials.
Summary
Valvular heart disease is a major contributor to cardiovascular morbidity and mortality in women—the leading cause of mortality in women worldwide. Many studies demonstrate anatomic and pathophysiologic gender differences in the structure and function of aortic and mitral valve disease processes. These differences are not incorporated in current ACC/AHA guidelines for diagnosis and management of aortic and mitral disease, which leads to the under-diagnosis and undertreatment of VHD in women. As a result, women present later in the disease process and experience increased risk for VHD-related events and increased morbidity and mortality with surgical and percutaneous interventions. These sex specific differences are likely to be amplified in older adults, as women compose a greater proportion of the aging population with increased life expectancy compared to men.
Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Anon. Aortic Stenosis Overview. https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/heart-valve-problems-and-causes/problem-aortic-valve-stenosis. Accessed 9 Feb 2024.
Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: executive summary: a report of the american college of cardiology/american heart association joint committee on clinical practice guidelines. Circulation. 2021;143:e35–71.
Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368:1005–11.
• Tribouilloy C, Bohbot Y, Rusinaru D, et al. Excess mortality and undertreatment of women with severe aortic stenosis. J Am Heart Assoc. 2021;10:e018816. Despite prevalent symptoms, AVR is less often performed in women and 5-year excess mortality is noted in women versus men, even after age matching.
Hariri EH, El Halabi J, Kassis N, et al. Sex differences in the progression and long-term outcomes of native mild to moderate aortic stenosis. JACC Cardiovasc Imaging. 2024;17:1–12.
Thaden JJ, Nkomo VT, Suri RM, et al. Sex-related differences in calcific aortic stenosis: correlating clinical and echocardiographic characteristics and computed tomography aortic valve calcium score to excised aortic valve weight. Eur Heart J. 2016;37:693–9.
Rodriguez-Gabella T, Zimarino M, Barbanti M, et al. Sex based analysis of the impact of red blood cell transfusion and vascular or bleeding complications related to TAVI - The TRITAVI-Women Study. Int J Cardiol. 2021;333:69–76.
Nguyen V, Mathieu T, Melissopoulou M, et al. Sex differences in the progression of aortic stenosis and prognostic implication: the COFRASA-GENERAC study. JACC Cardiovasc Imaging. 2016;9:499–501.
Chaker Z, Badhwar V, Alqahtani F, et al. Sex differences in the utilization and outcomes of surgical aortic valve replacement for severe aortic stenosis. J Am Heart Assoc. 2017;6:e006370.
Elhmidi Y, Piazza N, Mazzitelli D, Wottke M, Lange R, Bleiziffer S. Sex-related differences in 2197 patients undergoing isolated surgical aortic valve replacement. J Card Surg. 2014;29:772–8.
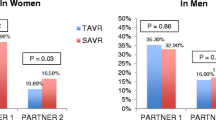
Panoulas VF, Francis DP, Ruparelia N, et al. Female-specific survival advantage from transcatheter aortic valve implantation over surgical aortic valve replacement: Meta-analysis of the gender subgroups of randomised controlled trials including 3758 patients. Int J Cardiol. 2018;250:66–72.
O’Connor SA, Morice M-C, Gilard M, et al. Revisiting sex equality with transcatheter aortic valve replacement outcomes: a collaborative, patient-level meta-analysis of 11,310 patients. J Am Coll Cardiol. 2015;66:221–8.
Zhou C, Xia Z, Chen B, Song Y, Lian Z. Gender differences in age-stratified early outcomes in patients with transcatheter aortic valve implantation. Am J Cardiol. 2023;187:100–9.
Bienjonetti-Boudreau D, Fleury M-A, Voisine M, et al. Impact of sex on the management and outcome of aortic stenosis patients. Eur Heart J. 2021;42:2683–91.
Zahid S, Khan MZ, Ullah W, et al. Gender Differences in Age-Stratified Inhospital Outcomes After Transcatheter Aortic Valve Implantation (from the National Inpatient Sample 2012 to 2018). Am J Cardiol. 2022;167:83–92.
Tersalvi G, Gaiero L, Capriolo M, et al. Sex differences in epidemiology, morphology, mechanisms, and treatment of mitral valve regurgitation. Medicina (Kaunas). 2023;59:1017.
El-Busaid H, Hassan S, Odula P, Ogeng’o J, Ndung’u B. Sex variations in the structure of human atrioventricular annuli. Folia Morphol (Warsz). 2012;71:23–7.
Gual-Capllonch F, Sáenz de Ibarra JI, Bayés-Genís A, Delgado V. Atrial mitral and tricuspid regurgitation: sex matters a call for action to unravel the differences between women and men. Front Cardiovasc Med. 2022;9:877592.
Elmariah S, Budoff MJ, Delaney JAC, et al. Risk factors associated with the incidence and progression of mitral annulus calcification: the multi-ethnic study of atherosclerosis. Am Heart J. 2013;166:904–12.
Avierinos J-F, Inamo J, Grigioni F, Gersh B, Shub C, Enriquez-Sarano M. Sex differences in morphology and outcomes of mitral valve prolapse. Ann Intern Med. 2008;149:787–95.
David TE, Ivanov J, Armstrong S, Christie D, Rakowski H. A comparison of outcomes of mitral valve repair for degenerative disease with posterior, anterior, and bileaflet prolapse. J Thorac Cardiovasc Surg. 2005;130:1242–9.
Vakamudi S, Jellis C, Mick S, et al. Sex Differences in the Etiology of Surgical Mitral Valve Disease. Circulation. 2018;138:1749–51.
Lawrie GM. Surgical treatment of mitral regurgitation. Curr Opin Cardiol. 2020;35:491–9.
Bonow RO, O’Gara PT, Adams DH, et al. 2020 focused update of the 2017 ACC expert consensus decision pathway on the management of mitral regurgitation: a report of the american college of cardiology solution set oversight committee. J Am Coll Cardiol. 2020;75:2236–70.
Lazam S, Vanoverschelde J-L, Tribouilloy C, et al. Twenty-year outcome after mitral repair versus replacement for severe degenerative mitral regurgitation: analysis of a large, prospective, multicenter. International Registry Circulation. 2017;135:410–22.
Gammie JS, Sheng S, Griffith BP, et al. Trends in mitral valve surgery in the United States: results from the Society of Thoracic Surgeons Adult Cardiac Surgery Database. Ann Thorac Surg. 2009;87:1431–7.
Song HK, Grab JD, O’Brien SM, Welke KF, Edwards F, Ungerleider RM. Gender differences in mortality after mitral valve operation: evidence for higher mortality in perimenopausal women. Ann Thorac Surg. 2008;85:2040–4.
Vassileva CM, McNeely C, Spertus J, Markwell S, Hazelrigg S. Hospital volume, mitral repair rates, and mortality in mitral valve surgery in the elderly: an analysis of US hospitals treating Medicare fee-for-service patients. J Thorac Cardiovasc Surg. 2015;149:762-768.e1.
Seeburger J, Eifert S, Pfannmüller B, et al. Gender differences in mitral valve surgery. Thorac Cardiovasc Surg. 2013;61:42–6.
Mohadjer A, Brown G, Shah SR, et al. Sex-based differences in coronary and structural percutaneous interventions. Cardiol Ther. 2020;9:257–73.
Feldman T, Foster E, Glower DD, et al. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med. 2011;364:1395–406.
Obadia J-F, Messika-Zeitoun D, Leurent G, et al. Percutaneous repair or medical treatment for secondary mitral regurgitation. N Engl J Med. 2018;379:2297–306.
Stone GW, Lindenfeld J, Abraham WT, et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med. 2018;379:2307–18.
• Kosmidou I, Lindenfeld J, Abraham WT, et al. Sex-specific outcomes of transcatheter mitral-valve repair and medical therapy for mitral regurgitation in heart failure. JACC Heart Fail. 2021;9:674–83. In the COAPT trial, mitral TEER resulted in improved clinical outcomes compared with GDMT alone, irrespective of sex. However, the impact of mitral TEER in reducing HFH was less pronounced in women compared with men beyond the first year after treatment.
Werner N, Puls M, Baldus S, et al. Gender-related differences in patients undergoing transcatheter mitral valve interventions in clinical practice: 1-year results from the German TRAMI registry. Catheter Cardiovasc Interv. 2020;95:819–29.
Anon. Ageing and health. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. Accessed 9 Feb 2024.
Kodali SK, Velagapudi P, Hahn RT, Abbott D, Leon MB. Valvular Heart Disease in Patients ≥80 Years of Age. J Am Coll Cardiol. 2018;71:2058–72.
• Attinger-Toller A, Ferrari E, Tueller D, et al. Age-related outcomes after transcatheter aortic valve replacement: insights from the SwissTAVI Registry. JACC Cardiovasc Interv. 2021;14:952–60. Increasing age is associated with a linear trend for mortality, stroke, and pacemaker implantation during early and longer-term follow-up after TAVR. Standardized mortality ratios were higher for TAVR patients younger than 90 years of age compared with expected rates of mortality in an age- and sex-matched Swiss population.
Alachkar MN, Kirschfink A, Alnaimi A, et al. Transcatheter mitral valve repair is feasible and effective in oldest-old patients: results from real-world cohort. J Geriatr Cardiol. 2022;19:761–7.
van der Kley F, van Rosendael PJ, Katsanos S, et al. Impact of age on transcatheter aortic valve implantation outcomes: a comparison of patients aged ≤ 80 years versus patients > 80 years. J Geriatr Cardiol. 2016;13:31–6.
van den Brink FS, Wijtsma I, Amrane H, et al. Outcome of transcatheter aortic valve replacement in patients over 85 years of age versus patients aged 85 and younger. Neth Heart J. 2022;30:473–8.
Kahraman AN. Impact of age on long term survival following transcatheter aortic valve implantation. J Geriatr Cardiol. 2019;16:265–71.
Ismayl M, Abbasi MA, Al-Abcha A, et al. Outcomes of transcatheter aortic valve implantation in nonagenarians and octogenarians (analysis from the national inpatient sample database). Am J Cardiol. 2023;199:59–70.
Galatas C, Afilalo J. Transcatheter aortic valve replacement over age 90: Risks vs benefits. Clin Cardiol. 2020;43:156–62.
Bernard J, St-Louis R, Robichaud M, et al. Is Transcatheter Aortic Valve Replacement Futile in Patients Over Ninety Years of Age? CJC Open. 2023;5:784–91.
Rashedi N, Otto CM. Treatment of severe aortic valve stenosis: impact of patient sex and life expectancy on treatment choice. Eur Cardiol. 2022;17:e25.
Malik AH, Zaid S, Yandrapalli S, et al. Trends and Outcomes With Transcatheter Versus Surgical Mitral Valve Repair in Patients ≥80 Years of Age. Am J Cardiol. 2020;125:1083–7.
Song C, Madhavan MV, Lindenfeld J, et al. Age-related outcomes after transcatheter mitral valve repair in patients with heart failure: analysis from COAPT. JACC Cardiovasc Interv. 2022;15:397–407.
Author information
Authors and Affiliations
Contributions
TD, LD, LL, and HF performed all literature review and authored the main manuscript text. SJP and TLJ served as senior authors and editors of the manuscript and finalized the manuscript submitted after review and editing.
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Desmarais, T., Dichiacchio, L., Fanous, H. et al. Gender Disparities in Valvular Heart Disease and Treatment in the Aging Population. Curr Geri Rep (2024). https://doi.org/10.1007/s13670-024-00419-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s13670-024-00419-6