Abstract
Purpose of Review
This review draws together recent publications, consensus statements on sarcoidosis and our 25-year collective experience in managing this disease. We focus on pulmonary sarcoidosis, highlighting recent and established concepts in disease mechanisms, the diversity of the clinical course, including possible ‘subtypes’ of sarcoidosis, and how to measure disease activity. We discuss the principles guiding therapeutic intervention and summarise the more recent clinical trials in sarcoidosis.
Recent Findings
These include recent progress in understanding the mechanisms of disease using new scientific tools, measurements of disease activity using CT and MRI scans, and the potential role of anti-fibrotic treatment for patients with progressive fibrotic sarcoidosis.
Summary
Sarcoidosis is a heterogeneous disease with variable organ involvement, disease course, and response to treatment. We offer an angle on when and how to treat, and provide an overall roadmap for managing sarcoidosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sarcoidosis is a very old disease. A lot of studies have contributed to the progressive mapping of disease mechanisms that underpins improvement in management. In this paper, we outline established understanding and new findings, and highlight seminal reviews and consensus statements in the last 5 years to provide context for our proposal on how to manage sarcoidosis. We focus on pulmonary sarcoidosis.
Disease Mechanisms Relevant to Clinical Management of Sarcoidosis
Sarcoidosis is an immune-mediated disease characterised by the presence of non-necrotizing granuloma and varying degrees of lymphocytic inflammation. In a nutshell, activated CD4 T cells with Th1 and Th17/Th17.1 bias are thought to be key drivers of granuloma formation and persistence [1, 2]. This is accompanied by abnormalities in the ability of the immune system to regulate itself. For example, dysfunctional regulatory T cells [3], reduction in invariant NKT cell numbers [4, 5] and polymorphisms in the BTNL2 gene [6] are proposed as contributors to the diminished control of proliferation and activity of T cells and monocytes [7]. A recent major mechanistic advance is the discovery that uninhibited mTOR signalling, possibly in lung macrophages, is central to unrestrained formation and persistence of granuloma in sarcoidosis. This has been demonstrated in murine models and transcriptomic data from human lung [8••] and bronchoalveolar samples [9••]. MTORC1 senses and integrates micro-environmental signals in order to regulate the metabolism and proliferation of many cells. Loss of control of this sensing pathway can lead to abnormalities in autophagy, (a critical mechanism to clear degraded intracellular material) and consequently, inadequate clearance of pathogens that could promote disease chronicity [10]. Abnormalities in the sensitivity by which the innate immune system and T lymphocytes sense pathogens or self-proteins, and resistance to apoptosis have also been suggested by genome-wide association studies (e.g., MHC II complex and ANXA11 polymorphisms respectively) [11, 12].
Granuloma formation and maintenance requires the collaboration of several components of the immune system, best demonstrated by studies in tuberculosis [13]. This means that there may be phases during the disease when T lymphocyte activity dominates, e.g., when the antigen/pathogen is present at a higher level, and other phases when macrophages play a more active role. Typically, there is a trigger or antigen for granulomagenesis or disease activity, which can take different forms. The large ACCESS (A Case Control Etiologic Study of Sarcoidosis) study did not identify one specific antigen in sarcoidosis but found a clear association with farming communities and occupations involving exposure to environmental inhalants and mold [14], supporting several exogenous antigens. Additional modulating factors such as stressful life events or infection are often required to ‘convert’ a predisposition, or quiescent/subclinical granuloma activity to clinically overt disease. A type 1 interferon signalling gene signature, usually upregulated during microbial encounter, has been found in transcriptomes of circulating blood immune cells of sarcoidosis patients [15], supporting an infective precipitant. Associations have also been observed with mycobacterial tuberculosis, Propionibacterium acnes and Borrelia species [16]. Several researchers have proposed that self-antigens may be a trigger for disease [17,18,19]. The latter is not proven but is an attractive hypothesis for sarcoidosis affecting internal organs such as the heart, brain and eyes.
Addressing external triggers or modulating factors like infection and stress is a key part of management and may influence treatment decisions. It is worth noting that insidious worsening of disease is the norm rather than acute exacerbations as granuloma formation is slow and takes at least a few weeks to months to consolidate. Therefore, acute worsening of disease is unusual unless there is a direct precipitant, like infection.
In the last 5 years, very few studies have added to this mechanistic understanding, but several have provided further support. Vukmirovic et al. performed bulk RNA sequencing on bronchoalveolar lavage (BAL) cells from 209 patients with sarcoidosis [9••], hypersensitivity pneumonitis and α1-anti trypsin deficiency and showed that gene sets for IL-1, IL-6, IL-8 signalling, and ‘stem cell reperfusion’ were progressively enriched in sarcoidosis as the Scadding staging increased. In those with fibrotic changes, genes regulating cell cycle and signal transduction in MTORC1 were amongst those significantly upregulated. This provides a sketch of the disease mechanisms involved that in turn underpin the management of sarcoidosis.
Clinical Features of Sarcoidosis Influencing Management Decisions
Sarcoidosis is a heterogeneous disease. The clinical course is unpredictable and patients can present with different organ involvement, severity and response to treatment. This heterogeneity in disease could be linked to the dominant underlying immune-pathological pathways at any one time, host genetics and/or the nature of the antigenic trigger that differ for each patient. These factors can also change over time and accordingly, the clinical manifestations of disease. Here, we highlight three features that impact on how we treat patients—the disease course, potential subtypes of disease and disease activity.
Disease Course
For most sarcoidosis patients, the disease is quiescent, mild and self-limiting but susceptibility to disease remains life-long. In around 50% of patients, sarcoidosis resolves within 6 months [20, 21], and in patients presenting with Lofgren’s syndrome, 80% resolve within 2 years [22]. For the remainder, several scenarios are observed—(i) patients can have low grade disease that lasts a few years that then resolves with or without treatment; (ii) the disease is active and requires a low level of immunosuppressive therapy to keep the disease from worsening; (iii) the disease is progressive and uncontrollable with current therapeutic options (less than 5% of patients). In the third scenario, there is often an additional factor driving the disease that may not be readily identifiable (e.g., recurrent infection, stress). Progressive or non-resolving highly active disease is a risk factor for fibrotic pulmonary sarcoidosis, which carries a significant mortality burden. A retrospective French cohort study (n = 142 patients) reported a mortality of 16% at 10 years from the point of diagnosis for those with fibrotic chest radiographs [23]. Progressive and extensive fibrotic disease is the most important determinant of survival in sarcoidosis (surpassing cardiac arrhythmia) [23]. Sarcoidosis patients with end-stage fibrotic disease in the United States United Network for Organ Sharing transplant database had a mortality rate of 28.1% in a 6-year period [24]. An important aim in the treatment of pulmonary sarcoidosis is therefore to prevent or limit fibrosis.
Radiological Subtypes of Pulmonary Disease
The clinical manifestations of sarcoidosis are wide-ranging, encompassing different patterns of pulmonary disease and extra-thoracic organ involvement. It is not clear whether there are true ‘endotypes’ of disease or if some of this variability relates to different antigenic stimuli or phase of disease when medical attention is sought. However, the organs involved tend to be defined early in disease. The ACCESS study showed that less than 20% of newly diagnosed patients had evidence of new organ involvement after their 2-year follow-up evaluation [14].
With pulmonary disease, there are at least four CT radiological patterns at the point of clinical presentation, which can evolve from one to another over time, as follows—(i) intrathoracic lymphadenopathy only with no lung parenchymal abnormality; (ii) nodularity along broncho-vascular bundles and fissures, typically diffuse or in clusters; (iii) perihilar conglomeration (defined as consolidation in continuum with hila) and masses, radiating from the hila, with accompanying nodularity and ground glass; or (iv) any of above but with fibrosis, signified by the presence of traction bronchiectasis, or in advanced disease, by fibro-cavitary and honeycombing/cystic changes on CT (Fig. 1a–d).
Established and emerging imaging modalities in management of sarcoidosis. a, b, c, d CT images demonstrating the different imaging appearances of sarcoidosis of lung at clinical presentation—bihilar lymphadenopathy without pulmonary parenchymal involvement (a), pulmonary nodularity in a peri-broncho-vascular and fissural distribution (b), perihilar conglomeration, ground glass opacification and nodularity, with or without fibrosis apparent (c) and perihilar distribution of disease with conglomeration, ground glass opacification, architectural distortion and traction bronchiectasis (active fibrotic disease) (d). PET-CT in sarcoidosis. These PET-CT scans were performed on a 70-year-old lady who presented with exertional dyspnoea secondary to pulmonary and cardiac sarcoidosis—appearances prior to treatment with areas of FDG avidity within the lungs (e) and repeat imaging 1 year later showing treatment response in lungs but new cardiac disease (f). (g) Advanced fibrotic sarcoidosis can resemble idiopathic pulmonary fibrosis with widespread traction bronchial dilatation and areas of cystic honeycombing
Ground glass opacification (GGO) and interlobular septal thickening are present in at least 10% of CT scans [25••] and histologically can signify cellular infiltration in the airspaces and lymphatics, respectively. GGO can also be due to fine fibrosis (particularly if associated with traction bronchiectasis) or cardiac failure, both of which are negative prognostic markers in sarcoidosis.
Disease Activity
Active disease can be viewed as disease that is progressive or where there are specific radiological abnormalities. The latter do not always cause overt disease or functional abnormalities so will not necessarily require treatment. However, recognising the presence of active disease allows physicians to monitor patients more carefully. Investigators have long attempted to find proxy measures of immune cell activity with blood assays that measure cellular proliferation or secretory activities. These include soluble IL-2Ra levels [26], ACE and calcium [27]. IL-2Ra are receptors for IL-2 that are upregulated in active T lymphocytes, and have been shown to be elevated in serum of various T cell-mediated disorders [28, 29]. However, these levels are not consistently increased in sarcoidosis. Similarly, serum ACE, which is a by-product of macrophage activity [30] and a reflection of the burden of granuloma, is not high in all patients even when there are clear features of active disease [30].
Due to the inconsistent correlation with disease activity, measures of cellular activity are less useful than radiological assessments of disease activity. Currently, the most accessible and informative radiological tests are high-resolution CT scan for pulmonary disease, gadolinium enhanced MRI scan for cardiac and neuro-sarcoidosis, and fluorodeoxyglucose positron emission tomography–CT (FDG-PET) scan for the heart and other organs.
For pulmonary sarcoidosis, CT imaging is the most informative way to evaluate disease activity, and also has the advantage of providing detailed information regarding the pattern and extent of disease. Broncho-vascular nodularity, ground glass opacity and conglomeration are associated with the presence of granuloma on open lung biopsies, while nodularity correlates strongly with BAL cell count and serum IL-2Ra levels [31]. The extent of nodularity and consolidation also positively correlate with the intensity of gallium uptake, and interlobular septal thickening with BAL lymphocytosis [31,32,33,34]. Thus, systematically measuring these HRCT abnormalities may allow quantification of disease activity and burden in pulmonary sarcoidosis. Most radiologists use these CT features to determine if the disease is active, and how disease activity evolves over time. Benamore et al. showed that a score (CTAS or CT Activity Score in Sarcoidosis), comprising the sum of nodularity, ground glass opacity, interlobular septal thickening and conglomeration/consolidation, reduced after treatment, supporting its use as a quantification tool for disease activity [25••].
FDG-PET-CT scanning is probably the most significant addition to the sarcoidosis management toolbox in the last decade [35]. Its use is based on the ability to detect metabolically active immune cells and granuloma due to increased glucose metabolic activity in these cells. A positive test is not specific for sarcoidosis but it allows detection of active cellular processes and their distribution (including occult disease), and can also sign-post sites for biopsy. It has a key role in diagnosing cardiac sarcoidosis but this requires a more stringent pre-test dietary protocol to improve sensitivity of detecting true cardiac involvement. An interesting study suggests that FDG-PET-CT can also be used to determine if fibrotic areas in the lungs are ‘active’. In a retrospective study (n = 89), Mostard and colleague found that 93% patients with Scadding stage IV sarcoidosis had FDG-avid fibrotic areas on PET-CT [36]. This supports the use of FDG-PET scans as a method of detecting active (rather than ‘burnt-out’) lung fibrosis and potentially identifying those most likely respond to anti-inflammatory and anti-fibrotic treatments. PET-CT can also be used to demonstrate lack of response to treatment [37, 38]and inform the need for alternative therapies [39] (Fig. 1e–f).
Principles of Management for Pulmonary Sarcoidosis
The key principles of management lie in firstly making an accurate diagnosis [40, 41] (particularly in excluding the presence of other conditions) and then protecting organ function whilst causing as little harm to the patient as possible. As it is not possible to accurately determine which patient will have self-limiting disease, assessing the threat to organ function is the most pragmatic way of determining whether or not to start drug treatment. In the case of pulmonary disease, we use the following criteria for commencing treatment:
-
1.
Presence of fibrosis on CT with features of active disease (i.e. fibrosis in association with ground glass opacification, nodularity, interlobular septal thickening, conglomeration or FDG avidity on PET-CT). This is usually a robust indication for treatment due to the risk of progressive fibrosis and irreversible impact on organ function. In these cases, we advocate treatment even when lung function tests are within normal range (unless there is a clear contraindication).
-
2.
Widespread or high burden pulmonary disease on CT accompanied by abnormal lung function but no fibrosis. This signifies organ dysfunction and treatment is usually indicated to improve or prevent further dysfunction. If there is widespread lung disease but normal lung function, the decision to treat is less clear-cut and requires discussion of the pros and cons. Careful monitoring of lung function and repeat imaging is required if a conservative approach is initially favoured.
-
3.
Pulmonary disease with low or moderate volume nodularity, ground glass opacity and/or interlobular septal thickening on CT imaging, with no evidence of fibrosis. In these cases, we would advocate a ‘watch and wait’ approach rather than treatment. In patients with breathlessness disproportionate to the extent of disease, it is important to consider other causes, such as cardiac involvement and pulmonary embolism.
Although this approach outlines the principles governing treatment, there are several nuances to consider. For example, it is not often clear if progression of disease in itself provides a sufficient threat to organ function to indicate treatment. Typically, sarcoidosis progresses relatively slowly and can fluctuate, thus, increases in lung abnormalities or a reduction in lung function over several months can be followed by spontaneous improvement some months later. In addition, there is not a general consensus as to what is ‘high’ or ‘low’ extent disease. There may be dense abnormalities in a small area of lung or sparse disease affecting all lobes. There could also be a small amount of ground glass opacification and nodularity around a small focal area of fibrosis in an elderly patient which may not justify the use of immunosuppressant therapy. In these cases, the pros and cons of treatment and threat to organ function should be evaluated on a case-by-case basis.
Patients with sarcoidosis can have debilitating symptoms such as fatigue and muscle aches which significantly impact their quality of life. The underlying causes for these symptoms are poorly understood but may, in part, be mediated by cytokines produced by activated immune cells. However, it is important to consider other aetiologies that also result in similar symptoms (e.g. depression, hypothyroidism, obstructive sleep apnoea, social pressures). We have found symptoms to be a poor indicator for treatment decisions. Many patients with severe progressive disease have few symptoms whilst other patients without physiological disturbances may be incapacitated by symptoms that are not responsive to immunosuppressant therapy or anti-inflammatories. In our experience, a judicious approach is encouraged, with an emphasis on holistic and supportive strategies for those without obvious organ abnormalities. Management of highly symptomatic sarcoidosis is discussed in the latest Statement from the British Thoracic Society [42••].
In parallel to the management algorithm for pulmonary sarcoidosis, those with the following extra-thoracic disease often require treatment—patients with cardiac sarcoidosis presenting with arrhythmia and cardiac failure [43], intracranial neuro-sarcoidosis, eye disease with risk to vision, renal involvement resulting in kidney dysfunction, and those with hypercalcaemia. Bone involvement affecting the vertebra also warrants careful consideration for therapeutic intervention. In all these cases, treatment is offered if the threat to organ function (and life) outweighs the adverse effects of corticosteroids and immunosuppressants. For other organs, the same treatment principles governing the lungs apply. For example, the presence of granuloma within the liver without significant liver function abnormalities requires monitoring rather than treatment and is a threat to function only if there is extensive disease. For cardiac disease with preserved function, a conservative approach can also be considered. Consideration of an implantable cardiac defibrillator [44] may be more appropriate for cardiac arrythmia alone without evidence of cardiac structural remodelling.
How to Treat Pulmonary Sarcoidosis
Induction and Maintenance Phases of Treatment
Most experts agree that short courses (e.g. a few weeks) of high-dose corticosteroids are less useful than a longer course of lower dose treatment (total of > 6 months) for long-term remission [12, 41, 42••].
Our approach to treatment adheres to the following principle—once requirement for drug treatment is agreed, prednisolone (or an immunosuppressant) is first used in higher doses for 1–3 months to achieve control of immune activity (we term this the induction phase), followed by a lower dose of prednisolone to maintain this control (the maintenance phase). The duration of the induction phase is the length required to achieve control of disease activity but typically lasts about 1 month. CT and lung function measurements are the most commonly used parameters to judge response. Radiological resolution, improvement, or in the case of progressive disease, halting of progression, are considered positive response to treatment. Complete resolution of disease or amelioration of disease activity is not necessary and often not realistic or achieved only with unacceptable side effects.
Once the induction phase has achieved its purpose, the maintenance phase of treatment is continued for at least 6 months. Here, treatment is aimed at maintaining the control of the immune activity achieved during the induction phase, and is usually demonstrated by sustained improvement in lung function or radiological imaging. In our experience, around 12–24 months of maintenance therapy is often required before withdrawal should be attempted.
Lung function testing is performed approximately 3 monthly and imaging (CXR or high-resolution CT scan, depending on age of patient) may be required approximately 6 monthly in some patients to assess success of treatment. Those who require lung imaging are typically those with progressive large volume lung disease.
A small number of patients require the reintroduction of treatment, necessitating repeating of the induction and maintenance regime within first 2 years of drug withdrawal. However, in general, very few patients require life-long treatment. The exception to this is those with large volume lung disease or active fibrotic disease. The need for continuation of treatment is assessed yearly. Apart from those with progressive fibrotic lung disease, treatment can usually be discontinued in those patients who have shown sustained recovery of lung function and evidence of improvement of radiographic abnormality.
Therapeutic Options
Prednisolone remains the first line and probably the best treatment where there are no relative or absolute contraindications (e.g. osteoporosis, diabetes mellitus, high body mass index, patient intolerance) [45]. For the majority of patients, the induction and maintenance regime with prednisolone described above is all that is required to bring the disease and immune activity under control.
If the induction phase fails to achieve disease control (usually evident at the 3–6-month point), a second-line immunosuppressant can be considered. Although this adds another drug, it does usually allow the reduction of high-dose corticosteroids to a more tolerable maintenance dose with fewer long-term side effects. Current second-line immunosuppressants include azathioprine, methotrexate and mycophenolate. These drugs typically require about 3 months for an effect to be observed. Azathioprine is used at a dose of 1.5–2 g/kg per day and methotrexate is usually effective at doses of 10–15 mg/week (with folic acid). In a recent retrospective study comparing infection rate in methotrexate with azathioprine, methotrexate appeared to be associated with fewer infections, although this needs further validation in a prospective study [46]. The use of mycophenolate is less established in sarcoidosis, and is largely based on data from clinical trials evaluating its efficacy in other inflammatory interstitial lung diseases. One retrospective study examining patients with sarcoidosis on immunosuppressants did not find improved efficacy of mycophenolate over other agents but did note equivalence, alongside good tolerability and favourable side effect profile [47].
Most patients who require second-line treatment will fall into the complex disease category, will require closer monitoring, and will benefit from input at dedicated sarcoidosis centres.
A final consideration is the management of disease which involves two or three organs. In such cases, the organ most under threat usually dictates treatment, e.g. in those with severe uveitis and minor lung disease, treatment is aimed at controlling eye disease.
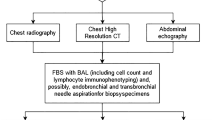
The above discussions are summarised in a roadmap of management as shown in Fig. 2.
Roadmap for management of sarcoidosis. Firstly secure the diagnosis, then characterise the disease and identify which organs are involved. Consider factors 2.1 to 2.4, and make a decision to treat or monitor without treatment within 6 months. Consider withdrawing treatment every 12 months along criteria described in text
Recent Therapeutic Trials in Sarcoidosis
Many pharmacological studies in sarcoidosis to date have been small, open label and based on retrospective data. The low numbers and heterogeneous patient groups make firm conclusions difficult. Therapeutic benefits could be evident in specific disease phenotypes, but trials designed to do this have not been available for sarcoidosis.
In the past two decades, the focus of most clinical trials has been on evaluating drugs licenced for other indications. The scientific rationale for this lies in the recognition that several of the immuno-pathological pathways that generate and sustain inflammatory and fibrotic diseases overlap with sarcoidosis. TNF-α antagonists, for example, have proven efficacy in rheumatoid arthritis and TNF-α has a role in driving inflammation and granuloma formation. Infliximab, a monoclonal antibody against TNF-α, is probably the most studied [48]. A randomised placebo-controlled trial involving 138 participants showed a modest increase in FVC of 2.5%, but there were no improvements in other endpoints including 6-min walk distance, dyspnoea scores or health-related quality of life measures [49]. An increase in FVC of around 7% was also reported in three non-controlled observational studies totalling 60 participants [48, 50, 51]. This led NICE to conclude in an Evidence Summary in 2016 that infliximab may be effective in a small subset of patients with active progressive disease refractory to first- and second-line immunosuppression but that further studies are needed [52]. At present, infliximab remains off label although can be considered third-line treatment for pulmonary sarcoidosis on a case-by-case basis in the UK. However, the drug is approved for neuro-sarcoidosis where more evidence for its efficacy is available [53].
There is good biological evidence that granulomatous inflammation can lead to fibrosis, and therefore targeting inflammation should prevent (or reduce) the development of fibrosis. However, in some patients, fibrosis appears to develop alongside or even independently of areas of radiologically apparent active disease (i.e. nodularity, conglomeration, ground glass opacification or interlobular septal thickening). Indeed, in some fibrotic cases of sarcoidosis, the radiological appearances are not dissimilar to IPF (Fig. 1g). The INBUILD study evaluated the role of nintedanib, a triple kinase inhibitor, in a range of progressive fibrotic interstitial pneumonias, including sarcoidosis. Although the number of sarcoidosis cases was small, the trial reached its primary endpoint of reduction in FVC decline and in the UK, nintedanib has now been approved for use in progressive fibrosis and can be considered for fibrotic pulmonary sarcoidosis [54••] However, there is not enough trial evidence for solo use of nintedanib in fibrotic sarcoidosis and as granulomatous inflammation is the predominant driver of disease manifestations, we currently advise anti-fibrotic therapy in carefully selected cases, usually as add-on therapy to immunosuppressants in the first instance.
Azithromycin, a macrolide antibiotic with immunomodulatory activity, reduces exacerbation frequency in COPD. Use of this antibiotic, focusing on cough as its main outcome measure, was studied in 21 patients with sarcoidosis and was found to improve cough frequency in over half and quality of life indices in the majority. However, there was no placebo group and the impact on other clinical or disease parameters was not studied [55]. The role of roflumilast, a PDE4 inhibitor, on ‘acute events’ in those with fibrotic sarcoidosis and a history of exacerbations was also recently assessed. This study was placebo-controlled and investigators used a fall in FEV1 to 90% baseline and/or an increase of prednisolone with or without antibiotics to define an ‘acute event’ over a 12-month period. The study demonstrated fewer falls in FEV1 and improved quality of life scores in the treatment group, although the results need to be interpreted with caution as only 10 patients in each arm completed the study [56].
Few patients with sarcoidosis have a significant smoking history, and some investigators propose that tobacco smoking may be a protective factor in the development of the disease. A recent pilot study enrolling 50 patients to receive a transdermal nicotine or placebo for 24 weeks found that those receiving active treatment showed increase in FVC (140 ml) compared with placebo, although the extent of lung involvement, measured through CT textural lung analysis scores remained unchanged [57].
Finally, a group of investigators used evidence of mycobacterial protein and DNA in sarcoidosis granuloma to hypothesise that mycobacteria species may drive the disease [16]. Supporting this, quadruple antibiotics (concomitant levaquin, azithromycin, ethambutol and rifabutin—CLEAR regime) targeting occult infection in cutaneous disease resulted in improvement of skin lesions after 8 weeks. However, an interesting 16-week placebo-controlled trial using the CLEAR regime for progressive pulmonary disease did not meet its primary outcome (FVC improvement) despite reduction in immune responses against mycobacterial antigens in the treatment group [58]. This is not used routinely but azithromycin should be considered as a prophylaxis in patients who have repeated lower respiratory tract infections.
Conclusion
In this review, we have provided mechanistic and clinical rationale for management and treatment of sarcoidosis, which is broadly reflected in other guidelines and statements. The outline here is intentionally simple, and we acknowledge that some sarcoidosis cases are more complex and require careful management in dedicated centres, where possible.
We emphasise the importance of confirming the diagnosis (outlined in detail in the 2020 British Thoracic Society Clinical Statement for Sarcoidosis), evaluating comorbidities, and characterising patients before treatment decisions are formed. We highlight active fibrosis, high burden disease and organ dysfunction (assessed via lung function tests) as key considerations for therapeutic intervention and provide a snapshot of some interesting clinical trials of new therapeutic agents.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Moller DR, et al. Genetic, immunologic, and environmental basis of sarcoidosis. Ann Am Thorac Soc. 2017;14(Supplement_6):S429–s436.
Ramstein J, et al. IFN-γ-producing T-helper 17.1 cells are increased in sarcoidosis and are more prevalent than T-Helper type 1 cells. Am J Respir Crit Care Med. 2016;193(11):1281–91.
Miyara M, et al. The immune paradox of sarcoidosis and regulatory T cells. J Exp Med. 2006;203(2):359–70.
Korosec P, et al. Deficiency of pulmonary Valpha24 Vbeta11 natural killer T cells in corticosteroid-naïve sarcoidosis patients. Respir Med. 2010;104(4):571–7.
Ho LP, et al. Deficiency of a subset of T-cells with immunoregulatory properties in sarcoidosis. Lancet. 2005;365(9464):1062–72.
Valentonyte R, et al. Sarcoidosis is associated with a truncating splice site mutation in BTNL2. Nat Genet. 2005;37(4):357–64.
Crawshaw A, et al. Abnormalities in iNKT cells are associated with impaired ability of monocytes to produce IL-10 and suppress T-cell proliferation in sarcoidosis. 2014;44(7):2165–2174.
•• Linke M, et al. Chronic signaling via the metabolic checkpoint kinase mTORC1 induces macrophage granuloma formation and marks sarcoidosis progression. Nat Immunol. 2017;18(3):293–302. Most recent substantive contribution to understanding of disease mechanism.
•• Vukmirovic M, et al. Transcriptomics of bronchoalveolar lavage cells identifies new molecular endotypes of sarcoidosis. Eur Respir J. 2021;58(6). Large study using high-resolution molecular techniques to examine lung-based immune response.
Pacheco Y, et al. Sarcoidosis and the mTOR, Rac1, and autophagy triad. Trends Immunol. 2020;41(4):286–99.
Fischer A, et al. Genetics of sarcoidosis. Semin Respir Crit Care Med. 2014;35(3):296–306.
Grunewald J, et al. Sarcoidosis Nature Reviews Disease Primers. 2019;5(1):45.
Flynn JL, Chan J, Lin PL. Macrophages and control of granulomatous inflammation in tuberculosis. Mucosal Immunol. 2011;4(3):271–8.
Baughman RP, et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med. 2001;164(10 Pt 1):1885–9.
Sweiss NJ, et al. Linkage of type I interferon activity and TNF-alpha levels in serum with sarcoidosis manifestations and ancestry. PLoS ONE. 2011;6(12):e29126.
Esteves T, Aparicio G, Garcia-Patos V. Is there any association between sarcoidosis and infectious agents?: a systematic review and meta-analysis. BMC Pulm Med. 2016;16(1):165–165.
Wahlström J, et al. Identification of HLA-DR–bound peptides presented by human bronchoalveolar lavage cells in sarcoidosis. J Clin Investig. 2007;117(11):3576–82.
Grunewald J, et al. T-cell receptor–HLA-DRB1 associations suggest specific antigens in pulmonary sarcoidosis. 2015;47:898-909.
Wahlström J, et al. Autoimmune T cell responses to antigenic peptides presented by bronchoalveolar lavage cell HLA-DR molecules in sarcoidosis. 2009;133(3):353–63.
Mañá J, et al. Multidisciplinary approach and long-term follow-up in a series of 640 consecutive patients with sarcoidosis: cohort study of a 40-year clinical experience at a tertiary referral center in Barcelona. Spain Medicine. 2017;96(29):e7595–e7595.
Judson MA, Boan AD, Lackland DT. The clinical course of sarcoidosis: presentation, diagnosis, and treatment in a large white and black cohort in the United States. Sarcoidosis Vasc Diffuse Lung Dis. 2012;29(2):119–27.
Grunewald J, Eklund A. Löfgren’s Syndrome. 2009;179(4):307–12.
Nardi A, et al. Stage IV sarcoidosis: comparison of survival with the general population and causes of death. Eur Respir J. 2011;38(6):1368–73.
Schott CA, et al. Declining pulmonary function in interstitial lung disease linked to lymphocyte dysfunction. Am J Respir Crit Care Med. 2020;201(5):610–3.
•• Benamore R, et al. CTAS: a CT score to quantify disease activity in pulmonary sarcoidosis. Thorax. 2016;71(12):1161–1163. One of very few studies to propose a lung-based scoring method for disease activity in pulmonary sarcoidosis.
Vanmaris RMM, Rijkers GT. Biological role of the soluble interleukin-2 receptor in sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2017;34(2):122–9.
Kraaijvanger R, et al. Biomarkers in the diagnosis and prognosis of sarcoidosis: current use and future prospects. 2020;11.
Rubin LA, et al. Serial levels of soluble interleukin 2 receptor in the peripheral blood of patients with rheumatoid arthritis: correlations with disease activity. J Rheumatol. 1990;17(5):597–602.
ter Borg EJ, et al. Changes in plasma levels of interleukin-2 receptor in relation to disease exacerbations and levels of anti-dsDNA and complement in systemic lupus erythematosus. Clin Exp Immunol. 1990;82(1):21–6.
Gilbert SR, et al. Amounts of angiotensin-converting enzyme mRNA reflect the burden of granulomas in granulomatous lung disease. 1993;148(2):483–6.
Oberstein A, et al. Non invasive evaluation of the inflammatory activity in sarcoidosis with high-resolution computed tomography. Sarcoidosis Vasc Diffuse Lung Dis. 1997;14(1):65–72.
Nishimura K, et al. CT and pathological correlation of pulmonary sarcoidosis. Semin Ultrasound CT MR. 1995;16(5):361–70.
Leung AN, et al. Sarcoidosis activity: correlation of HRCT findings with those of 67Ga scanning, bronchoalveolar lavage, and serum angiotensin-converting enzyme assay. J Comput Assist Tomogr. 1998;22(2):229–34.
Remy-Jardin M, et al. Pulmonary sarcoidosis: role of CT in the evaluation of disease activity and functional impairment and in prognosis assessment. Radiology. 1994;191(3):675–80.
Maturu VN, et al. Role of serial F-18 FDG PET/CT scans in assessing treatment response and predicting relapses in patients with symptomatic sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2016;33(4):372–80.
Mostard RL, et al. Inflammatory activity assessment by F18 FDG-PET/CT in persistent symptomatic sarcoidosis. Respir Med. 2011;105(12):1917–24.
Akaike G, et al. PET/CT in the diagnosis and workup of sarcoidosis: focus on atypical manifestations. Radiographics. 2018;38(5):1536–49.
Keijsers RG, et al. 18F-FDG PET in sarcoidosis: an observational study in 12 patients treated with infliximab. Sarcoidosis Vasc Diffuse Lung Dis. 2008;25(2):143–9.
Sobic-Saranovic D, et al. The utility of 18F-FDG PET/CT for diagnosis and adjustment of therapy in patients with active chronic sarcoidosis. J Nucl Med. 2012;53(10):1543–9.
Crouser ED, et al. Diagnosis and detection of sarcoidosis. An Official American Thoracic Society Clinical Practice Guideline. 2020;201(8):e26–51.
Belperio JA, et al. Diagnosis and treatment of pulmonary sarcoidosis: a review. JAMA. 2022;327(9):856–67.
•• Thillai M, et al. BTS Clinical statement on pulmonary sarcoidosis. Thorax. 2021;76(1):4. A recent consensus statement on features, diagnosis and management of pulmonary sarcoidosis.
Birnie David H, et al. Cardiac sarcoidosis. J Am Coll Cardiol. 2016;68(4):411–21.
Birnie DH, et al. HRS expert consensus statement on the diagnosis and management of arrhythmias associated with cardiac sarcoidosis. Heart Rhythm. 2014;11(7):1305–23.
Baughman RP, et al. ERS clinical practice guidelines on treatment of sarcoidosis. Eur Respir J. 2021;2004079.
Rossides M, et al. Infection risk in sarcoidosis patients treated with methotrexate compared to azathioprine: a retrospective ‘target trial’ emulated with Swedish real-world data. Respirology. 2021;26(5):452–60.
Hamzeh N, et al. Efficacy of mycophenolate mofetil in sarcoidosis. Respir Med. 2014;108(11):1663–9.
Vorselaars ADM, et al. Effectiveness of infliximab in refractory FDG PET-positive sarcoidosis. Eur Respir J. 2015;46(1):175–85.
Baughman RP, et al. Infliximab therapy in patients with chronic sarcoidosis and pulmonary involvement. Am J Respir Crit Care Med. 2006;174(7):795–802.
van Rijswijk HNAJ, et al. Changes in disease activity, lung function and quality of life in patients with refractory sarcoidosis after anti-TNF treatment. Expert Opin Orphan Drugs. 2013;1(6):437–43.
Ørum M, Hilberg O, Krag S, Bendstrup E. Beneficial effect of infliximab on refractory sarcoidosis. Danish Med J. 2012;10(40).
National Institute for Clinical Excellence (2016). Pulmonary sarcoidosis: infliximab. Available from: https://www.nice.org.uk/advice/es2/resources/pulmonary-sarcoidosis-infliximab-pdf-32171319493. (Accessed 8 May 2022).
Gelfand JM, et al. Infliximab for the treatment of CNS sarcoidosis: a multi-institutional series. Neurology. 2017;89(20):2092–100.
•• Wells AU, et al. Nintedanib in patients with progressive fibrosing interstitial lung diseases-subgroup analyses by interstitial lung disease diagnosis in the INBUILD trial: a randomised, double-blind, placebo-controlled, parallel-group trial. Lancet Respir Med. 2020;8(5):453–460. First study to show potential utility for anti-fibrotics in sarcoidosis.
Fraser SD, et al. Azithromycin for sarcoidosis cough: an open-label exploratory clinical trial. ERJ Open Research. 2020;6(4):00534–2020.
Baughman RP, et al. Roflumilast (Daliresp®) to reduce acute pulmonary events in fibrotic sarcoidosis: a multi-center, double blind, placebo controlled, randomized clinical trial. Sarcoidosis Vasc Diffuse Lung Dis. 2021;38(3):e2021035.
Crouser ED, et al. A pilot randomized trial of transdermal nicotine for pulmonary sarcoidosis. Chest. 2021;160(4):1340–9.
Drake WP, et al. Phase II investigation of the efficacy of antimycobacterial therapy in chronic pulmonary sarcoidosis. Chest. 2021;159(5):1902–12.
Funding
LPH is supported in part by the Oxford NIHR Biomedical Research Centre.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors do not have existing conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Interstitial Lung Disease
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fraser, E., Weeratunga, P. & Ho, LP. Management of Sarcoidosis: When to Treat, How to Treat and for How Long?. Curr Pulmonol Rep 11, 151–159 (2022). https://doi.org/10.1007/s13665-022-00298-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-022-00298-2