Abstract
Purpose of Review
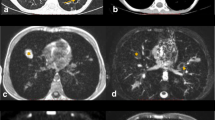
Magnetic resonance imaging (MRI) has robust soft tissue characterization capability which was previously limited to evaluation of the mediastinum, cardiac, and chest wall imaging. MRI has now progressed from an experimental tool to complementary and alternate radiation free imaging modality for optimal identification and comprehensive evaluation of the lung parenchyma including structural, functional, and real-time imaging covering lung nodules/masses, infections, interstitial lung disease, airway diseases, and vascular and pleural abnormalities.
Recent Findings
Recent use of fast imaging techniques and respiratory gating has overcome several of the previously reported MRI technical difficulties such as respiratory, cardiac and diaphragmatic motion, as well as susceptibility related to air tissue interface in the lungs.
Summary
MRI is a viable tool to the imaging armamentarium for the identification and characterization of pulmonary parenchymal abnormalities, providing complementary diagnostic information to computed tomography (CT), improving the non-invasive diagnostic accuracy and problem-solving for indeterminate lesions.












Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
de Groot PM, Chung JH, Ackman JB, Berry MF, Carter BW, Colletti PM, et al. ACR Appropriateness Criteria® noninvasive clinical staging of primary lung cancer. J Am Coll Radiol. 2019;16(5):S184–95.
McComb BL, Ravenel JG, Steiner RM, Chung JH, Ackman JB, Carter B, et al. ACR Appropriateness Criteria® chronic dyspnea-noncardiovascular origin. J Am Coll Radiol. 2018;15(11):S291–301.
Harun HH, Karim MK, Abbas Z, Sabarudin A, Muniandy SC, Ng KH. Radiation doses and cancer risk from CT pulmonary angiography examinations.
Lahham A, ALMasri H, Kameel S. Estimation of female radiation doses and breast cancer risk from chest CT examinations. Radiat Prot Dosim. 2018;179(4):303–9.
Schwartz F, Stieltjes B, Szucs-Farkas Z, Euler A. Over-scanning in chest CT: comparison of practice among six hospitals and its impact on radiation dose. Eur J Radiol. 2018;102:49–54.
Dournes G, Macey J, Blanchard E, Berger P, Laurent F. MRI of the pulmonary parenchyma: towards clinical applicability? Rev Pneumol Clin. 2017;73(1):40–9.
Parwani P, Ramesh T, Akhter N, Iliescu C, Palaskas N, Kim P, et al. Differentiation of cardiac masses by cardiac magnetic resonance imaging. Curr Cardiovasc Imaging Rep. 2020;13(1):1.
Kapur S, Bhalla AS, Jana M. Pediatric chest MRI: a review. Indian J Pediatr. 2019;5:1–2.
Hirsch FW, Sorge I, Vogel-Claussen J, Roth C, Gräfe D, Päts A, et al. The current status and further prospects for lung magnetic resonance imaging in pediatric radiology. Pediatr Radiol. 2020;29:1–6.
• Raptis CA, Ludwig DR, Hammer MM, Luna A, Broncano J, Henry TS, et al. Building blocks for thoracic MRI: challenges, sequences, and protocol design. J Magn Reson Imaging. 2019;50(3):682–701 The paper discusses the thoracic MRI protocol challenges and how to overcome them in clinical practice.
Chang KJ, Kamel IR, Macura KJ, Bluemke DA. 3.0-T MR imaging of the abdomen: comparison with 1.5 T. Radiographics. 2008;28(7):1983–98.
•• Biederer J, Beer M, Hirsch W, et al. MRI of the lung (2/3). Why... when ... how? Insights Imaging. 2012, 3(4):355–71. https://doi.org/10.1007/s13244-011-0146-8One of the first papers detailing lung MRI protocol for clinical use based on expert consensus.
Biederer J. General requirements of MRI of the lung and suggested standard protocol. In: Kauczor HU, Wielpütz MO, editors. MRI of the lung. Berlin Heidelberg: Springer; 2018.
Broncano J, Luna A, Caro P, Sanchez J, Vazquez J. Cardiac DWI:from basics to clinical applications. Eur Congress Radiol. 2018: C-2633. https://doi.org/10.1594/ecr2018/C-2633.
Winzer R, Hoberück S, Zöphel K, Kotzerke J, Brauer T, Hoffmann RT, et al. Diffusion-weighted MRI for initial staging in Hodgkins lymphoma: comparison with FDG PET. Eur J Radiol. 2020;123:108775.
Luna A, Sánchez-Gonzalez J, Caro P. Diffusion-weighted imaging of the chest. Magn Reson Imaging Clin N Am. 2011;19(1):69–94. https://doi.org/10.1016/j.mric.2010.09.006.
• Chen L, Zhang J, Bao J, et al. Meta-analysis of diffusion-weighted MRI in the differential diagnosis of lung lesions. J Magn Reson Imaging. 2013;37(6):1351–8. https://doi.org/10.1002/jmri.23939A meta-anlysis study evaluating role of DWI in differentiating benign from malignant lesions on chest MRI. This continues to be a highly investigated topic in MRI field to minimize need of invasive tissue sampling.
Yumrutepe S, Turtay MG, Oguzturk H, Aytemur Z, Guven T, Turgut K, et al. Diffusion-weighted magnetic resonance imaging of thorax in diagnosis of pulmonary embolism. Med Sci. 2018;7:759–61.
Christodoulou AG, Shaw JL, Nguyen C, Yang Q, Xie Y, Wang N, et al. Magnetic resonance multitasking for motion-resolved quantitative cardiovascular imaging. Nature Biomed Eng. 2018;2(4):215–26.
Zeng G, Teng Y, Zhu J, Zhu D, Yang B, Hu L, et al. Clinical application of MRI-respiratory gating technology in the evaluation of children with obstructive sleep apnea hypopnea syndrome. Medicine. 2018;97(4).
Ebner L, Kammerman J, Driehuys B, Schiebler ML, Cadman RV, Fain SB. The role of hyperpolarized 129xenon in MR imaging of pulmonary function. Eur J Radiol. 2017;86(2017):343–52. https://doi.org/10.1016/j.ejrad.2016.09.015.
Muradyan I, Patz S. Hyperpolarized 129Xenon MRI of the lung. In: Kauczor HU, Wielpütz MO, editors. MRI of the lung. Berlin Heidelberg: Springer; 2018.
Nasim F, Ost DE. Management of the solitary pulmonary nodule. Curr Opin Pulm Med. 2019;25(4):344–53.
Robertson J, Nicholls S, Bardin P, Ptasznik R, Steinfort D, Miller A. Incidental pulmonary nodules are common on CT coronary angiogram and have a significant cost impact. Heart Lung Circulation. 2019;28(2):295–301.
MacMahon H, Naidich DP, Goo JM, Lee KS, Leung AN, Mayo JR, et al. Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology. 2017;284(1):228–43.
Donnelly EF, Kazerooni EA, Lee E, Henry TS, Boiselle PM, Crabtree TD, et al. ACR Appropriateness Criteria® lung cancer screening. J Am Coll Radiol. 2018;15(11):S341–6.
• Cieszanowski A, Lisowska A, Dabrowska M, et al. MR imaging of pulmonary nodules: detection rate and accuracy of size estimation in comparison to computed tomography. PLoS One. 2016;11(6):1–11. https://doi.org/10.1371/journal.pone.0156272An important study evaluating diagnostic accuracy of MRI in detection of pulmonary nodules of various sizes. Currently, pulmonary nodules greater than 4 mm on CT require follow-up. This study showed that these nodules can be readily identified on MRI.
Sommer G, Tremper J, Koenigkam-Santos M, Delorme S, Becker N, Biederer J, et al. Lung nodule detection in a high-risk population: comparison of magnetic resonance imaging and low-dose computed tomography. Eur J Radiol. 2014;83(3):600–5. https://doi.org/10.1016/j.ejrad.2013.11.012.
Meier-Schroers M, Homsi R, Schild HH, Thomas D. Lung cancer screening with MRI: characterization of nodules with different non-enhanced MRI sequences. Acta Radiol. 2019;60(2):168–76. https://doi.org/10.1177/0284185118778870.
Wang X, Wan Q, Chen H, Li Y, Li X. Classification of pulmonary lesion based onmultiparametricMRI: utility of radiomics and comparison of machine learning methods. Eur Radiol. 2020;30:4595–4605. https://doi.org/10.1007/s00330-020-06768-y.
Ohno Y, Kauczor HU, Hatabu H, Seo JB, van Beek EJ, International Workshop for Pulmonary Functional Imaging (IWPFI). MRI for solitary pulmonary nodule and mass assessment: current state of the art. J Magn Reson Imaging. 2018;47(6):1437–58.
Ohno Y, Koyama H, Dinkel J. Lung cancer. In: Kauczor HU, Wielpütz MO, editors. MRI of the lung. Berlin Heidelberg: Springer; 2018.
Bruzzi JF, Komaki R, Walsh GL, Truong MT, Gladish GW, Munden RF, et al. Imaging of non-small cell lung cancer of the superior sulcus. RadioGraphics. 2008;28(2):561–72. https://doi.org/10.1148/rg.282075710.
Kratz JR, Woodard G, Jablons DM. Management of lung cancer invading the superior sulcus. Thorac Surg Clin. 2017;27(2):149–57.
Heelan RT, Demas BE, Caravelli JF, Martini N, Bains MS, McCormack PM, et al. Superior sulcus tumors: CT and MR imaging. Radiology. 1989;170(3):637–41.
Kurihara Y, Matsuoka S, Yamashiro T, Fujikawa A, Matsushita S, Yagihashi K, et al. MRI of pulmonary nodules. Am J Roentgenol. 2014;202(3):210–6. https://doi.org/10.2214/AJR.13.11618.
Kiryu T, Ohashi N, Matsui E, Hoshi H, Iwata H, Shimokawa K. Rounded atelectasis: delineation of enfolded visceral pleura by MRI. J Comput Assist Tomogr. 2002;26(1):37–8. https://doi.org/10.1097/00004728-200201000-00007.
Stathopoulos GT, Karamessini MT, Sotiriadi AE, Pastromas VG. Rounded atelectasis of the lung. Respir Med. 2005;99(5):615–23. https://doi.org/10.1016/j.rmed.2004.10.003.
Yang RM, Li L, Wei XH, Guo YM, Huang YH, Lai LS, et al. Differentiation of central lung cancer from atelectasis: comparison of diffusion-weighted MRI with PET/CT. PloS One. 2013 Apr 4;8(4):e60279. https://doi.org/10.1371/journal.pone.0060279.
Zhang X, Fu Z, Gong G, Wei H, Duan J, Chen Z, et al. Implementation of diffusion-weighted magnetic resonance imaging in target delineation of central lung cancer accompanied with atelectasis in precision radiotherapy. Oncol Lett. 2017;14(3):2677–82.
Jokerst C, Chung JH, Ackman JB, Carter B, Colletti PM, Crabtree TD, et al. ACR appropriateness criteria® acute respiratory illness in immunocompetent patients. J Am Coll Radiol. 2018;15(11):S240–51.
Lee C, Colletti PM, Chung JH, Ackman JB, Berry MF, Carter BW, et al. ACR Appropriateness Criteria® acute respiratory illness in Immunocompromised patients. J Am Coll Radiol. 2019;16(11):S331–9.
Liszewski MC, Görkem S, Sodhi KS, Lee EY. Lung magnetic resonance imaging for pneumonia in children. Pediatr Radiol. 2017;47(11):1420–30.
Marangu D, Gray D, Vanker A, Zampoli M. Exogenous lipoid pneumonia in children: a systematic review. Paediatr Respir Rev. 2019;33:45–51. https://doi.org/10.1016/j.prrv.2019.01.001.
Sehgal IS, Choudhary H, Dhooria S, Aggarwal AN, Bansal S, Garg M, et al. Prevalence of sensitization to Aspergillus flavus in patients with allergic bronchopulmonary aspergillosis. Med Mycol. 2019;57(3):270–6.
Gao Y, Soubani A. Advances in the diagnosis and management of pulmonary aspergillosis. Adv Respiratory Med. 2019;87(6):231–43.
Sodhi KS, Gupta P, Shrivastav A, Saxena AK, Mathew JL, Singh M, et al. Evaluation of 3 T lung magnetic resonance imaging in children with allergic bronchopulmonary aspergillosis: pilot study. Eur J Radiol. 2019;111:88–92.
Zeng J, Liu Z, Shen G, Zhang Y, Li L, Wu Z, et al. MRI evaluation of pulmonary lesions and lung tissue changes induced by tuberculosis. Int J Infect Dis. 2019;82:138–46. https://doi.org/10.1016/j.ijid.2019.03.004.
Romei C, Turturici L, Tavanti L, Miedema J, Fiorini S, Marletta M, et al. The use of chest magnetic resonance imaging in interstitial lung disease: a systematic review. Eur Respir Rev. 2018;27(150):180062.
Lonzetti L, Zanon M, Pacini GS, Altmayer S, Martins de Oliveira D, Rubin AS, et al. Magnetic resonance imaging of interstitial lung diseases: a state-of-the-art review. Respir Med. 2019;155(April 2019):79–85. https://doi.org/10.1016/j.rmed.2019.07.006.
Weatherley ND, Eaden JA, Stewart NJ, Bartholmai BJ, Swift AJ, Bianchi SM, et al. Experimental and quantitative imaging techniques in interstitial lung disease. Thorax. 2019;74(6):611–9.
Arkema EV, Cozier YC. Epidemiology of sarcoidosis: current findings and future directions. Therapeutic Adv Chronic Dis. 2018;9(11):227–40.
Bhalla AS, Das A, Naranje P, Goyal A, Guleria R, Khilnani GC. Dilemma of diagnosing thoracic sarcoidosis in tuberculosis-endemic regions: an imaging-based approach. Part 2. Indian J Radiol Imaging. 2017;27(4):380.
Chung JH, Cox CW, Forssen AV, Biederer J, Puderbach M, Lynch DA. The dark lymph node sign on magnetic resonance imaging: a novel finding in patients with sarcoidosis. J Thorac Imaging. 2014;29(2):125–9.
Gill RR, Gerbaudo VH, Jacobson FL, Trotman-Dickenson B, Matsuoka S, Hunsaker A, et al. MR imaging of benign and malignant pleural disease. Magn Reson Imaging Clin N Am. 2008;16(2):319–39. https://doi.org/10.1016/j.mric.2008.03.004.
Yaddanapudi K. Benign loculated pleural effusion. InPET/MR imaging. Cham: Springer; 2018. p. 77–8.
de Fonseka D, Walker S, Maskell N, Edey A. S58 role of MRI in characterising equivocal pleural thickening on CT.
Kaul V, McCracken DJ, Rahman NM, Epelbaum O. Contemporary approach to the diagnosis of malignant pleural effusion. Ann Am Thoracic Soc. 2019;16(9):1099–106.
Hierholzer J, Luo L, Bittner RC, Stroszczynski C, Schoenfeld N, Dorow P, et al. MRI and CT in the differential diagnosis of pleural disease. Chest. 2000;118(3):604–9.
Tsim S, Humphreys CA, Cowell GW, Stobo DB, Noble C, Woodward R, et al. Early contrast enhancement: a novel magnetic resonance imaging biomarker of pleural malignancy. Lung Cancer. 2018;118:48–56.
Usuda K, Iwai S, Funasaki A, Sekimura A, Motono N, Matoba M, et al. Diffusion-weighted imaging can differentiate between malignant and benign pleural diseases. Cancers. 2019;11(6):811.
Keskin Z, Yeşildağ M, Alkan E, Kayhan A, Tolu Ľ, Keskin S. Differentiation between transudative and exudative pleural effusions by diffusion weighted magnetic resonance imaging. Iran J Radiol. 2019;16(2):e78775. https://doi.org/10.5812/iranjradiol.78775.
Rezai S, Graves AG, Henderson CE. Thoracic endometriosis, a review. Obstet Gynecol Int J. 2019;10(5):342–6.
Montoriol PF, Da Ines D, Bourdel N, Garcier JM, Canis M. Re: thoracic endometriosis syndrome: CT and MRI features. Clin Radiol. 2014;69(5):549–50. https://doi.org/10.1016/j.crad.2014.01.023.
Rangunwala J, Sitta J, Vyas K, Roda M. Multimodality thoracoabdominal imaging findings in a rare case of thoracic endometriosis syndrome. Cureus. 2020;12(1):e6819. https://doi.org/10.7759/cureus.6819.
Maniglio P, Ricciardi E, Meli F, Vitale SG, Noventa M, Vitagliano A, et al. Catamenial pneumothorax caused by thoracic endometriosis. Radiol Case Rep. 2018;13(1):81–5.
Sanada T, Park J, Hagiwara M, Ikeda N, Nagai T, Matsubayashi J, et al. CT and MRI findings of bronchopulmonary endometriosis: a case presentation. Acta Radiol Open. 2018;7(10):2058460118801164.
Sinha S, Swift AJ, Kamil MA, et al. The role of imaging in malignant pleural mesothelioma: an update after the 2018 BTS guidelines. Clin Radiol. 2020. https://doi.org/10.1016/j.crad.2019.12.001.
Heussel CP, Wielputz MO, Kauczor HU. Disease of the pleura and the chest wall. In: Kauczor HU, Wielpütz MO, editors. MRI of the lung. Berlin Heidelberg: Springer; 2018.
Hosch W, Schlieter M, Ley S, Heye T, Kauczor HU, Libicher M. Detection of acute pulmonary embolism: feasibility of diagnostic accuracy of MRI using a stepwise protocol. Emerg Radiol. 2014;21(2):151–8. https://doi.org/10.1007/s10140-013-1176-y.
Marshall PS, Kerr KM, Auger WR. Chronic thromboembolic pulmonary hypertension. Clin Chest Med. 2013;34(4):779–97.
Aluja Jaramillo F, Gutierrez FR, Díaz Telli FG, Yevenes Aravena S, Javidan-Nejad C, Bhalla S. Approach to pulmonary hypertension: from CT to clinical diagnosis. Radiographics. 2018;38(2):357–73. https://doi.org/10.1148/rg.2018170046.
Nishiyama KH, Saboo SS, Tanabe Y, Jasinowodolinski D, Landay MJ, Kay FU. Chronic pulmonary embolism: diagnosis. Cardiovasc Diagnosis Therapy. 2018;8(3):253–71.
Yaddanapudi K. Pulmonary infarct. InPET/MR imaging. Cham: Springer; 2018. p. 71–2.
Scholz O, Denecke T, Böttcher J, Schwarz C, Mentzel HJ, Streitparth F, et al. MRI of cystic fibrosis lung manifestations: sequence evaluation and clinical outcome analysis. Clin Radiol. 2017;72(9):754–63. https://doi.org/10.1016/j.crad.2017.03.017.
Nagle SK, Puderbach M, Eichinger M, Altes TA. Magnetic resonance imaging of the lung: cystic fibrosis. In: Kauczor HU, Wielpütz MO, editors. MRI of the lung. Berlin Heidelberg: Springer; 2018.
Syrjala H, Broas M, Ohtonen P, Jartti A, Pääkkö E. Chest magnetic resonance imaging for pneumonia diagnosis in outpatients with lower respiratory tract infection. Eur Respir J. 2017;49(1):1601303.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pulmonary Radiology
Rights and permissions
About this article
Cite this article
Mushtaq, R., Jayagurunathan, U., Arif-Tiwari, H. et al. Pulmonary MRI: Applications and Use Cases. Curr Pulmonol Rep 9, 131–142 (2020). https://doi.org/10.1007/s13665-020-00257-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-020-00257-9