Abstract
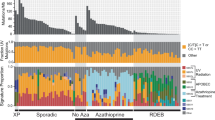
Extramammary Paget’s disease (EMPD) is a rare skin cancer that mainly occurs in apocrine sweat gland-rich areas in elderly people. The prognosis of metastatic EMPD is unfavorable because of the lack of fully effective systemic therapies. However, the difficulty in establishing a model of EMPD has hampered basic research for exploring its pathogenesis and optimal treatments. Here, we established for the first time an EMPD cell line (named KS-EMPD-1) from a primary tumor on the left inguinal region of an 86-year-old Japanese male. The cells were successfully maintained for more than 1 year, with a doubling time of 31.2 ± 0.471 h. KS-EMPD-1 exhibited constant growth, spheroid formation, and invasiveness, and was confirmed to be identical to the original tumor by short tandem repeat analyses, whole exome sequencing, and immunohistochemistry (CK7+CK20−GCDFP15+). Western blotting of the cells revealed the protein expression of HER2, NECTIN4, and TROP2, which have recently attracted attention as potential therapeutic targets for EMPD. KS-EMPD-1 was highly sensitive to docetaxel and paclitaxel on chemosensitivity test. The KS-EMPD-1 cell line is a promising resource for basic and preclinical research on EMPD to better define the tumor characteristics and treatment strategy of this rare cancer.





Similar content being viewed by others
References
Kibbi N, Owen JL, Worley B, et al. Evidence-based clinical practice guidelines for extramammary Paget disease. JAMA Oncol. 2022;8(4):618–28.
Kanitakis J. Mammary and extramammary Paget’s disease. J Eur Acad Dermatol Venereol. 2007;21(5):581–90.
Shepherd V, Davidson EJ, Davies-Humphreys J. Extramammary Paget’s disease. BJOG. 2005;112(3):273–9.
Ito T, Kaku-Ito Y, Furue M. The diagnosis and management of extramammary Paget’s disease. Exp Rev Anticancer Ther. 2018;18(6):543–53.
Hashimoto H, Ito T. Current management and treatment of extramammary Paget’s disease. Curr Treat Options Oncol. 2022;23(6):818–30.
Ishizuki S, Nakamura Y. Extramammary Paget’s disease: diagnosis, pathogenesis, and treatment with focus on recent developments. Curr Oncol. 2021;28(4):2969–86.
Simonds RM, Segal RJ, Sharma A. Extramammary Paget’s disease: a review of the literature. Int J Dermatol. 2019;58(8):871–9.
Funaro D, Krasny M, Lam C, Desy D, Sauthier P, Bouffard D. Extramammary Paget disease: epidemiology and association to cancer in a Quebec-based population. J Low Genit Tract Dis. 2013;17(2):167–74.
Nasioudis D, Bhadra M, Ko EM. Extramammary Paget disease of the vulva: Management and prognosis. Gynecol Oncol. 2020;157(1):146–50.
Yin S, Xu L, Wang S, et al. Prevalence of extramammary Paget’s disease in urban China: a population-based study. Orphanet J Rare Dis. 2021;16(1):134.
van der Zwan JM, Siesling S, Blokx WA, Pierie JP. Capocaccia R Invasive extramammary Paget’s disease and the risk for secondary tumours in Europe. Eur J Surg Oncol. 2012;38(3):214–21.
Ohara K, Fujisawa Y, Yoshino K, et al. A proposal for a TNM staging system for extramammary Paget disease: retrospective analysis of 301 patients with invasive primary tumors. J Dermatol Sci. 2016;83(3):234–9.
Hatta N, Yamada M, Hirano T, Fujimoto A, Morita R. Extramammary Paget’s disease: treatment, prognostic factors and outcome in 76 patients. Br J Dermatol. 2008;158(2):313–8.
Ito T, Kaku Y, Nagae K, et al. Tumor thickness as a prognostic factor in extramammary Paget’s disease. J Dermatol. 2015;42(3):269–75.
Murata T, Honda T, Egawa G, et al. Three-dimensional evaluation of subclinical extension of extramammary Paget disease: visualization of the histological border and its comparison to the clinical border. Br J Dermatol. 2017;177(1):229–37.
Matsuo K, Nishio S, Matsuzaki S, et al. Surgical margin status and recurrence pattern in invasive vulvar Paget’s disease: a Japanese Gynecologic Oncology Group study. Gynecol Oncol. 2021;160(3):748–54.
Kaku-Ito Y, Ito T, Tsuji G, et al. Evaluation of mapping biopsies for extramammary Paget disease: a retrospective study. J Am Acad Dermatol. 2018;78(6):1171-7.e4.
Li X, Zhao C, Kou H, Zhu F, Yang Y, Lu Y. PDD-guided tumor excision combined with photodynamic therapy in patients with extramammary Paget’s disease. Photodiagn Photodyn Ther. 2022;38: 102841.
Lukowiak TM, Perz AM, Aizman L, et al. Mohs micrographic surgery for male genital tumors: local recurrence rates and patient-reported outcomes. J Am Acad Dermatol. 2021;84(4):1030–6.
Hashimoto H, Kaku-Ito Y, Furue M, Ito T. Mucosal invasion, but not incomplete excision, has negative impact on long-term survival in patients with extramammary Paget’s disease. Front Oncol. 2021;11: 642919.
Hashimoto H, Kaku-Ito Y, Furue M, Ito T. The outcome of chemotherapy for metastatic extramammary Paget’s disease. J Clin Med. 2021;10(4):739.
Kato J, Hida T, Yamashita T, et al. Successful TS-1 monotherapy as the second-line treatment for advanced extramammary Paget’s disease: a report of two cases. J Dermatol. 2018;45(1):80–2.
Matsushita S, Fujii K, Kajihara I, et al. Efficacy of S-1 plus docetaxel in the treatment of metastatic extramammary Paget’s disease: a multicentre retrospective study. Br J Dermatol. 2021;185(2):458–60.
Fukuda K, Funakoshi T. Metastatic extramammary Paget’s disease: pathogenesis and novel therapeutic approach. Front Oncol. 2018;8:38.
Richter CE, Hui P, Buza N, et al. HER-2/NEU overexpression in vulvar Paget disease: the Yale experience. J Clin Pathol. 2010;63(6):544–7.
Tanaka R, Sasajima Y, Tsuda H, et al. Human epidermal growth factor receptor 2 protein overexpression and gene amplification in extramammary Paget disease. Br J Dermatol. 2013;168(6):1259–66.
Tanaka R, Sasajima Y, Tsuda H, et al. Concordance of the HER2 protein and gene status between primary and corresponding lymph node metastatic sites of extramammary Paget disease. Clin Exp Metastasis. 2016;33(7):687–97.
Bartoletti M, Mazzeo R, De Scordilli M, et al. Human epidermal growth factor receptor-2 (HER2) is a potential therapeutic target in extramammary Paget’s disease of the vulva. Int J Gynecol Cancer. 2020;30(11):1672–7.
Kusaba Y, Kajihara I, Myangat TM, et al. Clinical significance of ERBB2 S310F mutation in extramammary Paget’s disease. J Dermatol. 2022;49(9):e305–6.
Kimura T, Akamatsu Y, Kajihara I, Fukushima S, Ihn H. Case of metastatic extramammary Paget’s disease treated with trastuzumab-biosimilar monotherapy after S-1 and docetaxel combination chemotherapy. J Dermatol. 2020;47(1):e1-2.
Sekiguchi N, Kubota S, Noguchi T, et al. Experiences of trastuzumab plus paclitaxel combination therapy in metastatic human epidermal growth factor receptor 2-positive extramammary Paget’s disease: four cases and a review. J Dermatol. 2020;47(11):1276–9.
Zattarin E, Nichetti F, Ligorio F, et al. Case report: Prolonged clinical benefit with sequential trastuzumab-containing treatments in a patient with advanced extramammary Paget disease of the groin. Front Oncol. 2022;12: 925551.
Liegl B, Horn LC, Moinfar F. Androgen receptors are frequently expressed in mammary and extramammary Paget’s disease. Mod Pathol. 2005;18(10):1283–8.
Diaz de Leon E, Carcangiu ML, Prieto VG, et al. Extramammary Paget disease is characterized by the consistent lack of estrogen and progesterone receptors but frequently expresses androgen receptor. Am J Clin Pathol. 2000;113(4):572–5.
Azmahani A, Nakamura Y, Ozawa Y, et al. Androgen receptor, androgen-producing enzymes and their transcription factors in extramammary Paget disease. Hum Pathol. 2015;46(11):1662–9.
Yamada-Kanazawa S, Mijiddorj MT, Kajihara I, et al. Upregulated androgen receptor variant-7 mRNA and protein in extramammary Paget’s disease. J Eur Acad Dermatol Venereol. 2022;36(9):e724–6.
Goto H, Sugita K, Yamamoto O. Expression of programmed death-ligand 1 and programmed death-1 in patients with extramammary Paget’s disease. Indian J Dermatol. 2021;66(2):169–73.
Kato J, Sugita S, Horimoto K, et al. Expression of programmed cell death ligand 1 (PD-L1) at in situ and invasive extramammary Paget’s disease and literature review. Australas J Dermatol. 2021;62(3):412–4.
Mauzo SH, Tetzlaff MT, Milton DR, et al. Expression of PD-1 and PD-L1 in extramammary Paget disease: implications for immune-targeted therapy. Cancers (Basel). 2019;11(6):754.
Hashimoto H, Kaku-Ito Y, Oda Y, Ito T. CDK4: a novel therapeutic target for extramammary Paget’s disease. Front Oncol. 2021;11: 710378.
Chang K, Li GX, Kong YY, et al. Chemokine receptors CXCR4 and CXCR7 are associated with tumor aggressiveness and prognosis in extramammary Paget disease. J Cancer. 2017;8(13):2471–7.
Kusaba Y, Kajihara I, Myangat TM, et al. Intertumor and intratumor heterogeneity of PIK3CA mutations in extramammary Paget’s disease. J Dermatol. 2022;49(5):508–14.
Kitamura S, Yanagi T, Maeda T, Shimizu H. Drp1 expression levels correlate with clinical stage in extramammary Paget’s disease. J Eur Acad Dermatol Venereol. 2020;34(9):e510–3.
Murata M, Ito T, Tanaka Y, Kaku-Ito Y, Furue M. NECTIN4 expression in extramammary Paget’s disease: implication of a new therapeutic target. Int J Mol Sci. 2020;21(16):5891.
Hashimoto H, Tanaka Y, Murata M, Ito T. Nectin-4: a novel therapeutic target for skin cancers. Curr Treat Options Oncol. 2022;23(4):578–93.
Ito T, Tanegashima K, Tanaka Y, et al. Trop2 expression in extramammary Paget’s disease and normal skin. Int J Mol Sci. 2021;22(14):7706.
Takeichi T, Okuno Y, Matsumoto T, et al. Frequent FOXA1-activating mutations in extramammary Paget’s disease. Cancers (Basel). 2020;12(4):820.
Kiniwa Y, Yasuda J, Saito S, et al. Identification of genetic alterations in extramammary Paget disease using whole exome analysis. J Dermatol Sci. 2019;94(1):229–35.
Lin JR, Liang J, Zhang QA, et al. Microarray-based identification of differentially expressed genes in extramammary Paget’s disease. Int J Clin Exp Med. 2015;8(5):7251–60.
Ishida Y, Kakiuchi N, Yoshida K, et al. Unbiased detection of driver mutations in extramammary Paget disease. Clin Cancer Res. 2021;27(6):1756–65.
Stasenko M, Jayakumaran G, Cowan R, et al. Genomic alterations as potential therapeutic targets in extramammary Paget’s disease of the vulva. JCO Precis Oncol. 2020;4:PO.20.00073.
Kang Z, Xu F, Zhang QA, et al. Oncogenic mutations in extramammary Paget’s disease and their clinical relevance. Int J Cancer. 2013;132(4):824–31.
Rao Y, Zhu J, Zheng H, Ren Y, Ji T. Cell origin and genome profile difference of penoscrotum invasive extramammary Paget disease compared with its in situ counterpart. Front Oncol. 2022;12: 972047.
Nishi M, Tashiro M, Yoshida H. Stimulation of growth by both androgen and estrogen of the EMP-K1 transplantable tumor with androgen and estrogen receptors from human extramammary Paget’s disease in nude mice. J Natl Cancer Inst. 1992;84(7):519–23.
Maeda T, Kitamura S, Nishihara H, Yanagi T. Extramammary Paget’s disease patient-derived xenografts harboring ERBB2 S310F mutation show sensitivity to HER2-targeted therapies. Oncogene. 2020;39(36):5867–75.
Arita T, Kondo J, Kaneko Y, et al. Novel ex vivo disease model for extramammary Paget’s disease using the cancer tissue-originated spheroid method. J Dermatol Sci. 2020;99(3):185–92.
Ito T, Hashimoto H, Tanaka Y, et al. NECTIN4 expression in sebaceous and sweat gland carcinoma. Eur J Dermatol. 2022;32(2):181–6.
Tanaka Y, Murata M, Tanegashima K, Oda Y, Ito T. Nectin cell adhesion molecule 4 regulates angiogenesis through Src signaling and serves as a novel therapeutic target in angiosarcoma. Sci Rep. 2022;12(1):4031.
Ito T, Hashimoto H, Tanaka Y, et al. TROP2 expression in sebaceous and sweat gland carcinoma. J Clin Med. 2022;11(3):607.
Tanaka Y, Murata M, Oda Y, Furue M, Ito T. Nectin cell adhesion molecule 4 (NECTIN4) expression in cutaneous squamous cell carcinoma: a new therapeutic target? Biomedicines. 2021;9(4):355.
Tanaka Y, Murata M, Shen CH, Furue M, Ito T. NECTIN4: a novel therapeutic target for melanoma. Int J Mol Sci. 2021;22(2):976.
Murata M, Ito T, Tanaka Y, Yamamura K, Furue K, Furue M. OVOL2-mediated ZEB1 downregulation may prevent promotion of actinic keratosis to cutaneous squamous cell carcinoma. J Clin Med. 2020;9(3):618.
Ito T, Kohashi K, Yamada Y, et al. Prognostic significance of forkhead box M1 (FoxM1) expression and antitumour effect of FoxM1 inhibition in melanoma. Histopathology. 2016;69(1):63–71.
Ito T, Kohashi K, Yamada Y, et al. Prognostic significance of forkhead box M1 (FOXM1) expression and antitumor effect of FOXM1 inhibition in angiosarcoma. J Cancer. 2016;7(7):823–30.
Tanaka Y, Ito T, Kaku-Ito Y, et al. Human epidermal growth factor receptor 3 serves as a novel therapeutic target for acral melanoma. Cell Death Discov. 2023;9(1):54.
Tanaka Y, Uchi H, Furue M. Antioxidant cinnamaldehyde attenuates UVB-induced photoaging. J Dermatol Sci. 2019;96(3):151–8.
Tanaka Y, Ito T, Tsuji G, Furue M. Baicalein inhibits benzo[a]pyrene-induced toxic response by downregulating Src phosphorylation and by upregulating NRF2-HMOX1 system. Antioxidants (Basel). 2020;9(6):507.
Tanaka Y, Uchi H, Ito T, Furue M. Indirubin-pregnane X receptor-JNK axis accelerates skin wound healing. Sci Rep. 2019;9(1):18174.
Capes-Davis A, Theodosopoulos G, Atkin I, et al. Check your cultures! A list of cross-contaminated or misidentified cell lines. Int J Cancer. 2010;127(1):1–8.
Bolger AM, Lohse M, Usadel B. Trimmomatic: A flexible trimmer for Illumina sequence data. Bioinformatics. 2014;30(15):2114–20.
https://bio-bwa.sourceforge.net. Accessed 7 June 2023.
Li H, Handsaker B, Wysoker A, et al. The sequence alignment/map format and SAMtools. Bioinformatics. 2009;25(16):2078–9.
https://varscan.sourceforge.met. Accessed 7 June 2023.
https://asia.ensembl.org/info/docs/tools/vep/index.html. Accessed 7 June 2023.
Han SJ, Kwon S, Kim KS. Challenges of applying multicellular tumor spheroids in preclinical phase. Cancer Cell Int. 2021;21:152.
Hanahan D, Weomberg R. Hall marks of cancer: the next generation. Cell. 2011;144:646–74.
Liston DR, Davis M. Clinically relevant concentrations of anticancer drugs: a guide for nonclinical studies. Clin Cancer Res. 2017;23(14):3489–98.
Tsuchiya R, Yoshimatsu Y, Noguchi R, et al. Establishment and characterization of NCC-DDLPS4-C1: a novel patient-derived cell line of dedifferentiated liposarcoma. J Pers Med. 2021;11(11):1075.
Saito S, Morita K, Kohara A, et al. Use of BAC array CGH for evaluation of chromosomal stability of clinically used human mesenchymal stem cells and of cancer cell lines. Hum Cell. 2011;24(1):2–8.
Ben-David U, Beroukhim R, Golub TR. Genomic evolution of cancer models: Perils and opportunities. Nat Rev Cancer. 2019;19(2):97–109.
Tseng YY, Boehm JS. From cell lines to living biosensors: New opportunities to prioritize cancer dependencies using ex vivo tumor cultures. Curr Opin Genet Dev. 2019;54:33–40.
U.S. Food and Drug Administration, FoundationOne® CDx. 2023. https://www.accessdata.fda.gov/cdrh_docs/pdf17/P170019S029B.pdf. Accessed 7 June 2023.
Noorolyai S, Shajari N, Baghbani E, Sadreddini S, Baradaran B. The relation between PI3K/AKT signaling pathway and cancer. Gene. 2019;698:120–8.
Hoxhaj G, Manning BD. The PI3K–AKT network at the interface of oncogenic signaling and cancer metabolism. Nat Rev Cancer. 2020;20(2):74–88.
Niland S, Riscanevo AX, Eble JA. Matrix metalloproteinases shape the tumor microenvironment in cancer progression. Int J Mol Sci. 2023;23:146.
Bassiouni W, Ali MAM, Schulz R. Multifunctional intracellular matrix metalloproteinases: implications in disease. FEBS J. 2021;288:7162–82.
Djuric T, Zivkovic M. Overview of MMP biology and gene associations in human diseases. In: Travascio F, editor. The role of matrix metalloproteinase in human body pathologies. London: Academic; 2017. p. 3–33.
Fusumae T, Fukuda K, Hirai I, et al. Outcomes in patients with extramammary Paget disease with brain metastasis: a retrospective analysis. J Am Acad Dermatol. 2020;83(6):1832–4.
Hirai I, Tanese K, Nakamura Y, Ishii M, Kawakami Y, Funakoshi T. Combination cisplatin–epirubicin–paclitaxel therapy for metastatic extramammary Paget’s disease. Oncologist. 2019;24(6):e394–6.
Nakamura Y, Tanese K, Hirai I, et al. Weekly docetaxel monotherapy for metastatic extramammary Paget’s disease: retrospective single-institute analysis. J Dermatol. 2020;47(4):418–22.
Yin X, Li X, Li M, et al. Treatment of metastatic primary extramammary Paget disease with combination anlotinib and tislelizumab: a case report and review of the literature. Front Med (Lausanne). 2022;9: 891958.
Criscitiello C, Morganti S, Curigliano G. Antibody-drug conjugates in solid tumors: a look into novel targets. J Hematol Oncol. 2021;14(1):20.
Acknowledgements
We are grateful to Dr. Takashi Inozume (Chiba University Graduate School of Medicine, Chiba, Japan) for his technical advice on primary cell culture. We also thank our patient as well as all members of our laboratory for their helpful advice.
Funding
This work was supported by JSPS KAKENHI, Grant number JP 22K15543 (T.I.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflicts of interest.
Ethical approval
This study was approved by the Ethics Committee of Kyushu University Hospital (Approval no. 21050-00, approved on November 10th, 2021).
Informed consent
Written informed consent was obtained from the patient before inclusion in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ito, T., Tanaka, Y., Ichiki, T. et al. KS-EMPD-1: a novel cell line of primary extramammary Paget’s disease. Human Cell 36, 1813–1829 (2023). https://doi.org/10.1007/s13577-023-00951-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13577-023-00951-1