Abstract
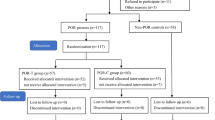
The effects of repeated controlled ovarian stimulation (COS) on the female reproductive system are still controversial. This study investigated the effects of repeated COS on the ovaries and uterus of mice and its possible mechanism. Female ICR (Institute of Cancer Research) mice were subjected to the COS using pregnant mare serum gonadotropin (PMSG) and human chorionic gonadotropin (hCG) for 1, 3, 5, and 7 cycles. Serum hormone levels, reactive oxidative stress (ROS), 8-hydroxy-2’-deoxyguanosine (8-OHdG), total antioxidant capacity (T-AOC), and superoxide dismutase (SOD) in the mouse ovary and uterus were analyzed by ELISA. The morphology of the ovary and endometrium, ovarian apoptosis, and expressions of the vascular endothelial growth factor (VEGF), leukemia inhibitory factor (LIF), PI3K, AKT, Bax, and Bcl-2 in the ovarian and uterine tissues were tested by hematoxylin–eosin (HE) staining, immunohistochemistry, and western blot. The results showed that repeated COS significantly decreased the hormone level (estradiol, progesterone and anti-Müllerian hormone), high-quality of the MII oocyte ratio, oocyte and embryo number, antioxidant capacity (T-AOC, SOD activity), and the protein level of Bcl-2, LIF, and VEGF, but increased the oxidative damage (ROS, 8-OHdG content), embryo fragment ratio, and expression of pro-apoptotic protein Bax. In addition, the expressions of p-PI3K and p-AKT also decreased with the increase of COS cycle. In conclusion, repeated COS causes ovarian and uterus damage possibly through the PI3K/AKT signaling pathway, and this finding may provide some experimental basis for guiding clinical treatment.






Similar content being viewed by others
Data availability
Availability of the data can be obtained from the corresponding author on reasonable requirements.
References
de Mouzon J, Chambers GM, Zegers-Hochschild F, et al. International committee for monitoring assisted reproductive technologies world report: assisted reproductive technology 2012. Hum Reprod. 2020;35(8):1900–13.
Ma YC, Zhao ZM, Hao GM, et al. Effects of multicycle gonadotropin-releasing hormone antagonist protocols on oxidative stress of follicular fluid and ovarian granulosa cells. Hum Cell. 2021;34(5):1324–34.
Shapiro BS, Richter KS, Harris DC, et al. Ramatic declines in Implantation and pregnancy rates in patients who undergo repeated cycles of in vitro fertilization with blastocyst transfer after one or more failed attempts. Fertil Steril. 2001;76(3):538–42.
Rabinson J, Ashkenazi J, Homburg R, et al. Repeated in vitro fertilization cycle attempts in patients undergoing controlled ovarian hyperstimulation with use of gonadotropin-releasing hormone antagonists. Fertil Steril. 2009;91(4):1473–5.
Kalthur G, Salian SR, Nair R, et al. Distribution pattern of cytoplasmic organelles, spindle integrity, oxidative stress, octamer-binding transcription factor 4 (Oct4) expression and developmental potential of oocytes following multiple superovulation. Fertil Steril. 2009;91(4 Suppl):1473–5.
Xiao P, Nie JY, Wang XF, et al. Melatonin alleviates the deterioration of oocytes from mice subjected to repeated superovulation. J Cell Physiol. 2019;234(8):13413–22.
Ma YC, Hao GM, Cui N, et al. Effects of Bushen-Tiaojing-Fang on the pregnancy outcomes of infertile patients with repeated controlled ovarian stimulation. Sci Rep. 2021;11(1):15233.
Xie JK, Wang Q, Zhang TT, et al. Repeated superovulation may affect mitochondrial functions of cumulus cells in mice. Sci Rep. 2016;6:31368.
Tang SB, Yang LL, Zhang TT, et al. Multiple superovulations alter histone modifications in mouse early embryos. Reproduction. 2019;157(6):511–23.
Ireland JLH, Scheetz D, Jimenez-Krassel F, et al. Antral follicle count reliably predicts number of morphologically healthy oocytes and follicles in ovaries of young adult cattle. Biol Reprod. 2008;79(6):1219–25.
Zhang JJ, Lai ZW, Shi LY, et al. Repeated superovulation increases the risk of osteoporosis and cardiovascular diseases by accelerating ovarian aging in mice. Aging (Albany NY). 2018;10(5):1089–102.
Matsumoto H, Ma WG, Daikoku T, et al. Cyclooxygenase-2 differentially directs uterine angiogenesis during implantation in mice. J Biol Chem. 2002;277(32):29260–7.
Cheng EH, Liu JY, Lee TH, et al. Requirement of leukemia inhibitory factor or epidermal growth factor for pre-implantation embryogenesis via JAK/STAT3 signaling pathways. PLoS ONE. 2016;11(4): e0153086.
Senapati S, Wang F, Ord T, et al. Superovulation alters the expression of endometrial genes critical to tissue remodeling and placentation. J Assist Reprod Genet. 2018;35(10):1799–808.
Zuo X, Li LM, Sun L. Plantamajoside inhibits hypoxia-induced migration and invasion of human cervical cancer cells through the NF-κB and PI3K/akt pathways. J Recept Signal Transduct Res. 2021;41(4):339–48.
Karuputhula NB, Chattopadhyay R, Chakravarty B, et al. Oxidative status in granulosa cells of infertile women undergoing IVF. Syst Biol Reprod Med. 2013;59(2):91–8.
Bedaiwy MA, Elnashar SA, Goldberg JM, et al. Effect of follicular fluid oxidative stress parameters on intracytoplasmic sperm injection outcome. Gynecol Endocrinol. 2012;28(1):51–5.
Younis A, Clower C, Nelsen D, et al. The relationship between pregnancy and oxidative stress markers on patients undergoing ovarian stimulations. J Assist Reprod Genet. 2012;29(10):1083–9.
Thaker R, Mishra V, Gor M, et al. The role of stimulation protocol, number of oocytes retrieved with respect to follicular fluid oxidative stress and IVF outcome. Hum Fertil (Camb). 2020;23(1):23–31.
Nie XW, Dai YJ, Zheng Y, et al. Establishment of a mouse model of premature ovarian failure using consecutive superovulation. Cell Physiol Biochem. 2018;51(5):2341–58.
Liu B, Wang JL, Wang XM, et al. Reparative effects of lycium barbarum polysaccharide on mouse ovarian injuries induced by repeated superovulation. Theriogenology. 2020;145:115–25.
Jinno M, Ozaki T, Iwashita M, et al. Measurement of endometrial tissue blood flow: a novel way to assess uterine receptivity for implantation. Fertil Steril. 2001;76(6):1168–74.
Winship A, Correia J, Zhang JG, et al. Leukemia inhibitory factor (LIF) inhibition during mid-gestation impairs trophoblast invasion and spiral artery remodelling during pregnancy in mice. PLoS ONE. 2015;10(10): e0129110.
Boudjenah R, Molina-Gomes D, Wainer R, et al. The vascular endothelial growth factor (VEGF) +405G/C polymorphism and its relationship with recurrent implantation failure in women in an IVF programme with ICSI. J Assist Reprod Genet. 2012;29(12):1415–20.
Camargo-Díaz F, García V, Ocampo-Bárcenas A, et al. Colony stimulating factor-1 and leukemia inhibitor factor expression from current-cycle cannula isolated endometrial cells are associated with increased endometrial receptivity and pregnancy. BMC Womens Health. 2017;17(1):63.
Ozornek MH, Bielfeld P, Krussel JS, et al. Epidermal growth factor and leukemia inhibitory factor levels in follicular fluid Association with in vitro fertilization outcome. J Reprod Med. 1999;44(4):367–9.
Arici A, oral E, Bahtiyar O, et al. Leukaemia inhibitory factor expression in human follicular fluid and ovarian cells 115. Hum Reprod. 1997;12(6):1233–9.
Zhao Y, Agarwal VR, Mendelson CR, et al. Transcriptional regulation of CYP19 gene (aromatase) expression in adipose stromal cells in primary culture. J Steroid Biochem Mol Biol. 1997;61(3–6):203–10.
Abdollahi M, Salehnia M, Salehpour S, et al. Analysis of apoptosis in cultured human vitrified ovarian tissue in the presence of leukemia inhibitory factor. J Reprod Infertil. 2018;19(4):193–202.
Danforth DR, Arbogast LK, Ghosh S, et al. Vascular endothelial growth factor stimulates preantral follicle growth in the rat ovary. Biol Reprod. 2003;68(5):1736–41.
Haidari K, Salehnia M, Rezazadeh VM. The effect of leukemia inhibitory factor and coculture on the in vitro maturation and ultrastructure of vitrified and nonvitrified isolated mouse preantral follicles. Fertil Steril. 2008;90(6):2389–97.
Tiwari M, Prasad S, Tripathi A, et al. Apoptosis in mammalian oocytes: a review. Apoptosis. 2015;2(8):1019–25.
Zhang D, Han M, Zhou MJ, et al. Down-regulation of S100P induces apoptosis in endometrial epithelial cell during GnRH antagonist protocol. Reprod Biol Endocrinol. 2021;19(1):99.
Jin X, Han CS, Yu FQ, et al. Anti-apoptotic action of stem cell factor on oocytes in primordial follicles and its signal transduction. Mol Reprod Dev. 2005;70(1):82–90.
Rossé T, Olivier R, Monney L, et al. Bcl-2 prolongs cell survival after Bax-induced release of cytochrome c. Nature. 1998;391(6666):496–9.
Combelles CMH, Albertini DF. Assessment of oocyte quality following repeated gonadotropin stimulation in the mouse. Bio Reproduction. 2003;68(3):812–21.
Shapiro BS, Richter KS, Harris DC, et al. Dramatic declines in implantation and pregnancy rates in patients who undergo repeated cycles of in vitro fertilization with blastocyst transfer after one or more failed attempts. Fertil Steril. 2001;76(3):538–42.
Silberstein T, Trimarchi JR, Gonzalez L, et al. Pregnancy outcome in in vitro fertilization decreases to a plateau with repeated cycles. Fertil Steril. 2005;84(4):1043–5.
Funding
This work was supported by the National Natural Science Foundation of China (No. 81774359, 82174419), Natural Science Foundation of Hebei Province (No. H2020423077), and the open projects of Hebei Key Laboratory of Integrative Medicine on Liver-kidney Patterns (No. A202104).
Author information
Authors and Affiliations
Contributions
HD and JC performed study design. SZ, YM, QZ, ML, ZY, YS, CS, HS, and GH collected the data of the experiment. SZ and YM supervised the study. SZ and YM prepared the figures. All authors validated the study. SZ and YM wrote the original paper. BG revised the paper.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
This study was approved by the Animal Ethics Committee of Hebei University of Chinese Medicine (No. DWLL2018036).
Consent for publication
Data have been approved for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, S., Ma, Y., Zuo, Q. et al. Repeated controlled ovarian stimulation-induced ovarian and uterine damage in mice through the PI3K/AKT signaling pathway. Human Cell 36, 234–243 (2023). https://doi.org/10.1007/s13577-022-00829-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13577-022-00829-8