Abstract
Introduction
Gamma knife radiosurgery is a well established method of treating intracranial metastases. We created a dose algorithm based on our standard clinical practice, taking into account tumor volume, number of metastases, radiosensitivity, and prior whole brain radiation treatment. We performed a phase 2 study to validate this algorithm and to investigate the feasibility of a larger clinical trial.
Methods
A total of 39 patients were prospectively enrolled at Yale New Haven Hospital (YNHH) between April 3, 2014 and November 21, 2016. There were 114 evaluable brain metastases. The pre-defined primary endpoint of this study was the control of all irradiated lesions for each patient. Survival was estimated using the method of Kaplan-Meier. Cox proportional hazard regression was performed to identify factors associated with survival and local control.
Results
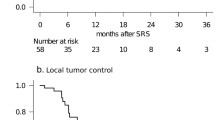
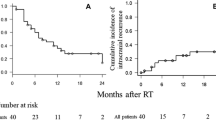
The median patient age of enrolled patients was 64 years (range, 34–88). Of the 114 evaluable lesions, 58 (50.9%) had complete response, 16 (14.0%) had partial response, 33 (28.9%) had stable disease, and 7 (6.1%) had progression at last imaging follow-up. Therefore, there was a per-lesion local control rate of 93.9%. Six (15.3%) patients developed symptomatic radiation necrosis requiring steroids or surgery, with median time to occurrence of 6 months. Median survival after gamma knife was 11.4 months (95% CI 4.9–15.7). Age was the only significant variable in univariate and multivariate analysis. Having a bladder primary (vs. lung) was associated with a higher risk of death, although this was based on only two patients and therefore is of unclear significance.
Conclusion
In this pilot/phase II study, we learned: (1) radiosurgery using radiation doses based on our algorithm provides good local control with low toxicity. (2) Despite the relative commonality of brain metastases, patients with brain metastases are difficult to enroll on clinical trials. (3) A prospective study that encompasses all potentially important clinical variables that go into radiosurgery dose selection will require large amounts of patients. Our findings have important implications for future clinical trials of radiosurgery for brain metastases.



Similar content being viewed by others
References
An Y, Jiang W, Kim BYS, Qian JM, Tang C, Fang P, Logan J, D'Souza NM, Haydu LE, Wang XA, Hess KR, Kluger H, Glitza IC, Mahajan A, Welsh JW, Lin SH, Yu JB, Davies MA, Hwu P, Sulman EP, Brown PD, Chiang VLS, Li J (2017) Stereotactic radiosurgery of early melanoma brain metastases after initiation of anti-CTLA-4 treatment is associated with improved intracranial control. Radiother Oncol 125:80–88
Andrews DW, Scott CB, Sperduto PW, Flanders AE, Gaspar LE, Schell MC, Werner-Wasik M, Demas W, Ryu J, Bahary JP, Souhami L, Rotman M, Mehta MP, Curran WJ Jr (2004) Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet 363:1665–1672
Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, Hatano K, Kenjyo M, Oya N, Hirota S, Shioura H, Kunieda E, Inomata T, Hayakawa K, Katoh N, Kobashi G (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295:2483–2491
Colaco RJ, Martin P, Kluger HM, Yu JB, Chiang VL (2016) Does immunotherapy increase the rate of radiation necrosis after radiosurgical treatment of brain metastases? J Neurosurg 125:17–23
Colaco RJ, Yu JB, Bond JS, Bindra RS, Contessa JN, Knisely JPS, Chiang VL (2016) A contemporary dose selection algorithm for stereotactic radiosurgery in the treatment of brain metastases - An initial report. J Radiosurg SBRT 4:43–52
Goldberg SB, Gettinger SN, Mahajan A, Chiang AC, Herbst RS, Sznol M, Tsiouris AJ, Cohen J, Vortmeyer A, Jilaveanu L, Yu J, Hegde U, Speaker S, Madura M, Ralabate A, Rivera A, Rowen E, Gerrish H, Yao X, Chiang V, Kluger HM (2016) Pembrolizumab for patients with melanoma or non-small-cell lung cancer and untreated brain metastases: early analysis of a non-randomised, open-label, phase 2 trial. Lancet Oncol 17:976–983
Shaw E, Scott C, Souhami L, Dinapoli R, Kline R, Loeffler J, Farnan N (2000) Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90-05. Int J Radiat Oncol Biol Phys 47:291–298
Taylor BF, Knisely JP, Qian JM, Yu JB, Chiang VL (2016) Predicting treatment related imaging changes (TRICs) after radiosurgery for brain metastases using treatment dose and conformality metrics. J Radiosurg SBRT 4:53–60
Vogelbaum MA, Angelov L, Lee SY, Li L, Barnett GH, Suh JH (2006) Local control of brain metastases by stereotactic radiosurgery in relation to dose to the tumor margin. J Neurosurg 104:907–912
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was the work of the authors without funding.
Conflict of interest
James B. Yu has received a research gift from twenty-first Century Oncology. He has received consulting fees from Augmenix Inc. All the other authors report no conflicts of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the Yale HIC and with the 1964 Helsinki declaration on a Yale Human Investigational Committee (HIC) approved study (HIC# 1306012291).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Yu, J.B., Singh, C., Bindra, R.S. et al. Results of a pilot/phase II study of gamma knife radiosurgery for brain metastases and implications for future prospective clinical trials. J Radiat Oncol 8, 39–46 (2019). https://doi.org/10.1007/s13566-018-0370-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13566-018-0370-7