Abstract
Introduction
Alopecia areata (AA) is an autoimmune skin disease presenting as nonscarring hair loss. Information on the epidemiology of AA, especially the occurrence of AA and its subtypes within the general population, is scarce. The study aimed to estimate the incidence rates and prevalence of hospital-treated AA and its subtypes in Denmark and to examine the demographic and clinical characteristics of patients with AA, including comorbidities and use of prescription medications.
Methods
This was a cohort study based on data from administrative and health registers in Denmark in 1995–2016. The study included individuals who were (1) registered with a hospital inpatient or hospital-based outpatient clinic diagnosis of AA between 1995 and 2016 in the Danish National Patient Registry covering encounters at all Danish hospitals, (2) alive and resided in Denmark anytime between 1995 and 2016, (3) aged ≥ 12 years, and (4) resided uninterrupted in Denmark during the 12 months before the first AA diagnosis during the study period.
Results
During the study period, 2778 individuals with an incident hospital-based diagnosis of AA were identified; 63.1% were female and 28.7% of the patients were aged ≥ 50 years. Over the study period, the overall incidence rate for any hospital-treated AA per 100,000 person-years was 2.62 (95% confidence interval [CI], 2.53–2.72), and the overall prevalence in 2016 was 71.7 (95% CI 69.4–74.1) per 100,000 persons. Both incidence rate and prevalence increased over time. Prevalence of most hospital-treated comorbidities or history of medication use was below 10% and was similar in the alopecia totalis (AT)/alopecia universalis (AU) and non-AT/AU subtypes of AA.
Conclusion
This cohort study reported incidence rates and prevalence over time and characteristics of individuals with hospital-treated AA in Denmark, which are in agreement with those previously reported in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Given the emergence of new treatment options, information on the occurrence of alopecia areata (AA) and its subtypes in various populations and care settings is of greater interest. |
This study evaluated the incidence rates and prevalence of hospital-treated AA and its subtypes in Denmark, as well as patients’ demographic and clinical characteristics. |
What was learned from this study? |
In 1995–2016, there were 2778 patients with incident hospital-treated AA in Denmark. A majority of patients were female and < 50 years of age, and prevalence of hospital-treated comorbidities was low. |
The overall incidence rate of AA was 2.62 per 100,000 person-years, and the overall prevalence in 2016 was 71.7 per 100,000 persons. Incidence rate and prevalence of AA increased over time. |
Hospital-treated patients with AA are likely to represent a more severe spectrum of disease than patients with AA treated outside the hospital. |
Introduction
Alopecia areata (AA) is an autoimmune disease with an underlying immunoinflammatory pathogenesis [1]. AA presents as nonscarring hair loss ranging from small patches (alopecia focalis) to complete scalp (alopecia totalis [AT]) or scalp, face, and body hair loss (alopecia universalis [AU]) [2, 3]. AA is the second most common cause of hair loss, affecting approximately 147 million individuals worldwide [4], with a lifetime risk of all subtypes of approximately 2% [5, 6]. AA unfavorably affects social interactions, quality of life, and employment [7]. The clinical course of the disease may be unpredictable and is marked by remission, progression, or persistence [8, 9].
Studies examining the epidemiology of AA, especially measuring the occurrence of AA and its subtypes within the general population, are scarce. Studies from the United Kingdom (UK), United States of America (USA), and Republic of Korea (South Korea) have reported incidence rates of AA ranging from approximately 20 to 200 per 100,000 person-years and prevalence estimates ranging from 0.21% to 0.58% [6, 10,11,12,13]. In Denmark, Eaton et al. [14, 15] reported a prevalence of AA of 0.21 per 1000 persons in 2001 and 0.27 per 1000 persons in 2006. However, incidence rates of AA in the Danish population over time have not been examined.
The aims of this study were to update the estimates of the incidence rates and prevalence of hospital-treated AA and its subtypes in Denmark and to describe the demographic and clinical characteristics (including hospital-treated comorbidities and use of prescription medications) among patients with hospital-treated AA. We addressed these aims in a cohort study based on data from Danish population-based registries.
Methods
Setting and Data Sources
This study was conducted in Denmark, a country with a population of approximately 5.8 million people with universal access to tax-funded healthcare. Most life and health events and services are routinely recorded in national registries and databases along with information on migration and deaths [16]. We based the study on five such databases: (1) Danish Civil Registration System (CRS) (data on pseudonymized identifier, residence, and vital status) [17], (2) Danish National Patient Registry (DNPR) (diagnoses from inpatient admissions to all Danish hospitals since 1977 and all outpatient specialist clinic and emergency room visits since 1995) [18], (3) Danish Cancer Registry (includes records of incident primary malignancies in Denmark since 1943 with mandatory reporting since 1987) [19], (4) Danish Cause of Death Registry [20], and (5) Danish National Health Services Prescription Database (DNHSPD) (data on dispensing of reimbursed prescription drugs since 2004; treatments during hospitalizations are not included in this data source) [21]. The study was in accordance with the Declaration of Helsinki.
Individuals were identified through their civil registration number, which is assigned at birth and stored in the Danish CRS, along with date of birth, residency status, and dates of immigration, emigration, and death. The CRS permitted accurate individual linkage among all registries used in this study. Moreover, the CRS allows almost complete follow-up of the Danish population [17].
Study Population
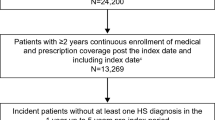
The source population were residents of Denmark between 1995 and 2016. The study population included individuals who were (1) registered with a hospital inpatient or outpatient diagnosis of AA between 1995 and 2016 in the DNPR, (2) alive and resided in Denmark anytime between 1995 and 2016, (3) aged ≥ 12 years at cohort entry date, and (4) resided uninterrupted in Denmark during the 12 months before the first AA diagnosis. The age restriction was applied to focus on the patient populations that had been included in recent studies of novel systemic treatments [22,23,24]. The cohort entry date was the date of AA diagnosis recorded in a Danish hospital. Individuals with a hospital diagnosis of AA before 1995 or alopecia of other etiologies (i.e., traction and scarring alopecia, other nonscarring hair loss, or cicatricial alopecia [scarring hair loss]) were excluded from the study.
The AA subtypes were categorized into AT/AU or non-AT/AU using combinations of International Classification of Diseases, 10th Revision (ICD-10) codes (Table S1). Patients falling into more than one subtype based on the first recorded ICD-10 codes at the AA cohort entry date were classified as AT/AU if they had the respective code; otherwise, they were classified as non-AT/AU.
Statistical Analyses
The incidence rates of hospital-treated AA were computed per 100,000 person-years among persons alive and in Denmark with no prior diagnoses of AA recorded in the DNPR starting on 01 January 1995. Incidence rates were stratified by AA subtype, age group, and sex. The annual incidence rates were computed per 100,000 persons in each calendar year between 1995 and the end of the study period, using midyear population aged ≥ 12 years as the denominator. The denominators (annual age- and sex-stratified population sizes) were obtained from official population statistics published by Statistics Denmark [25]. Incidences were reported with 95% confidence intervals (CIs).
The annual prevalence of hospital-treated AA and subtypes was computed using the midyear population size of each calendar year between 1995 and the end of the study period as the denominator and the number of persons alive and with a prior or current diagnosis of hospital-treated AA between 1977 and a full given calendar year in the numerator.
Hospital diagnoses of AA were based on inpatient stays between 1977 and 1994 and on outpatient or inpatient encounters thereafter. Since ICD-8 codes did not allow for stratification according to the AA subtype, prevalence calculations for AA subtypes were based on diagnoses from 1994 and later. All recorded AT/AU and non-AT/AU diagnoses were included in the prevalence calculations. Consequently, individuals with both diagnoses were included in calculations for both subgroups. Prevalence was stratified by age group and sex and reported with 95% CIs.
Patients with an incident diagnosis of hospital-treated AA from 1995 onward were described according to their demographic and clinical characteristics. Categorical variables were summarized using frequency and percentage, and continuous variables were summarized using medians with quartiles. Comorbidities (i.e., those recorded before the cohort entry date) were assessed using the entire available look-back period to 1977 for hospital diagnoses in the DNPR and 2004 for medication use registered in the DNHSPD. Overall hospital comorbidity burden was assessed using the Charlson Comorbidity Index (CCI). Conditions included in the CCI were identified in the DNPR. In addition, we reported prevalences of prespecified autoimmune and atopic diseases not included in the CCI. The definitions of the study variables are provided in the Table S1.
Ethical Approval
According to Danish law, studies based exclusively on registry (secondary) data are exempt from ethical approval or informed consent. This study was reported to the Danish Data Protection Agency, via registration with Aarhus University, record number 2016-051-000001/serial number 605.
Results
Incidence Rate and Prevalence of Hospital-Treated AA
Between 1995 and 2016, the overall incidence rate for hospital-treated AA per 100,000 person-years was 2.62 (95% CI 2.53–2.72). Figure 1 shows the annual incidence rates of AA and its subtypes from 1995 to 2016. In 2016, the year of the most recent data, the overall incidence rate for any hospital-treated AA per 100,000 person-years was 4.04 (95% CI 3.52–4.64). The incidence of the AT/AU subtype was 0.41 (95% CI 0.27–0.63) and for the non-AT/AU subtype was 3.63 (95% CI 3.14–4.20). The highest incidence rates for any AA and its subtypes were observed among the 12- to 17-year-old individuals. Regardless of the subtype, female patients had a higher incidence of AA than male patients (Table 1).
In 1995, the prevalence per 100,000 persons of any AA was 15.4 (95% CI 14.2–16.6). The annual prevalence increased continuously over the calendar time to 71.7 (95% CI 69.4–74.1) per 100,000 persons in 2016. In 2016, the prevalence of the AT/AU subtype was 19.6 (95% CI 18.4–20.9) and for the non-AT/AU type was 62.0 (95% CI 59.8–64.2). Figure 2 shows the calendar year-specific prevalence of AA and its subtypes. The 2016 prevalence was highest among the 18- to 50-year-old persons and in female patients regardless of the subtype (Table 1).
Characteristics of Patients with Hospital-Treated AA
In 1995–2016, 4089 individuals with a hospital diagnosis of AA were recorded in the DNPR. Of these, 2778 were identified as patients aged ≥ 12 years with incident AA (Fig. 3). Among the 2778 individuals with hospital-treated AA, 63.1% were female and 28.7% of patients were aged ≥ 50 years at the AA cohort entry date.
AT/AU vs. Non-AT/AU
The distribution of subtypes was 17% AT/AU (n = 472) and 83% non-AT/AU (n = 2306). Demographic characteristics were similar between patients with AT/AU and non-AT/AU subtypes. The median age at the AA cohort entry date was 42 years and 39 years for AT/AU and non-AT/AU respectively, with 90% of the AT/AU cohort and 89% of the non-AT/AU cohort being aged ≥ 18 years. The proportions of female patients were higher in both AT/AU (57.4%) and non-AT/AU (64.3%) cohorts.
The prevalence of most hospital comorbidities or history of medication use was below 10% (Table 2) and, with few exceptions, the prevalence of comorbidities was similar in both AA subtypes. Seventy-seven percent of patients had no hospital-treated comorbidities measured by CCI (i.e., low CCI score). Hearing loss and surgery in the last 6 months both occurred in a higher percentage of patients with AT/AU (5.3% and 3.6%, respectively) than in patients with non-AT/AU (2.7% and 1.9%, respectively). The most prevalent medications used among the AA cohort were antihypertensives (17.1%) and systemic steroids (14.7%). The prevalence of most autoimmune and atopic diseases among the AA cohort was low, except for atopic dermatitis (5.1%) and asthma (6.8%). Prevalence of autoimmune diseases according to AA subtypes are not reportable in compliance with the Danish data privacy rules. A list of comorbidities and number of patients by subtype is presented in Table 2.
Discussion
In this population-based cohort study in Denmark, we observed the overall incidence rate for any hospital-treated AA per 100,000 person-years of 2.62 (95% CI 2.53–2.72) and the overall prevalence in 2016 of 71.7 (95%% CI 69.4–74.1) per 100,000 persons. The prevalence of both AT/AU and non-AT/AU subtypes increased over time. The prevalence of most major comorbidities and prescription medication use was low and similar across the AT/AU and non-AT/AU subtypes.
Few previous studies have explored the epidemiology of AA. A Danish study similar to the current study but based on a shorter study period (2007–2016) and examining fewer comorbidities reported a similar or the same prevalence of comorbidities as in our study. This study examined all individuals with an AA diagnosis in the DNPR but did not stratify according to subtype [26]. Similar estimates were observed for several autoimmune or atopic diseases, including asthma (7.3% vs 6.8% in our study), Crohn’s disease (1.6% vs 1.3% in our study), ulcerative colitis (1.7% in both studies), and vitiligo (1.2% vs 6.8% in our study). A study based on claims data from the USA reported an association between the AT/AU subtype and higher occurrence of some autoimmune and inflammatory conditions [27]. Sensorineural hearing loss is a known disease manifestation of several autoimmune disorders and has been reported in patients with AA [28]. With regards to the higher prevalence of patients with AT/AU with a history of surgery in the previous 6 months in the present study, postsurgical stress could be associated with hair loss and thus it cannot be ruled out that some AA diagnoses represent misdiagnosed telogen effluvium.
Two other Danish studies by Eaton et al. [14, 15], based on the same data sources, reported estimated lifetime prevalence of hospital-treated AA of 0.21 per 1000 population in 2001 and 0.27 per 1000 population in 2006. These studies also used hospital-based diagnoses recorded in the DNPR; therefore, patients with AA diagnosed and treated outside an inpatient or outpatient hospital setting are not included in these estimates. Estimates according to AA subtypes were not assessed.
The reported incidence rate for all AA types in 2016 of 4.0 per 100,000 is lower than that in previous reports. A UK study, based on general practice data, found an incidence rate of AA of 26 per 100,000 person-years [11]. The USA Rochester Epidemiology Project, based on data from 1990 to 2009, reported an AA incidence rate (20.9 per 100,000 person-years) similar to the one reported in the UK study [29]. A South Korean study reported AA incidence ranging from 192.8 to 205.9 per 100,000 person-years from 2006 to 2015 [10]; however, the reported incidence of AT/AU ranged from 0.166 to 0.295 per 100,000 person-years and was similar to the AT/AU incidence rate observed in this study (0.41 per 100,000 person-years) [30].
The previously reported estimates of prevalence also differ from our results. The UK study reported a 2018 point prevalence of AA of 0.58%, which was likewise higher than the prevalence of 71.7 per 100,000 persons (0.072%) reported in this study for the year of 2016 [11]. A USA-based study by Benigno et al. [12] reported a 2017 annual prevalence of AA in a clinician-evaluated survey of patients of 0.21% (95% CI 0.17–0.25%). A recent USA study based on claims data reported estimates in line with those results, with a 2019 prevalence of AA of 0.222% (95% CI 0.221–0.223%). The 2019 prevalence of AT/AU was 0.019% (95% CI 0.018–0.019%) [13].
The approximately 10-fold lower prevalence and incidence for all AA types reported in Denmark compared with UK-, USA-, and South Korean-based estimates are likely explained by the potentially large number of patients with AA diagnosed and treated in general practice and therefore not included in this study.
Approximately 63% of all the incident cases were women, indicating female predominance, as has been observed in previous reports, including a Danish study from 2022 by Andersen et al. [13, 31,32,33] based on data from the Danish Skin Cohort (based on the DNPR, with dermatologist-verified skin diseases). The proportion of female patients with AA in the current study was slightly lower in the AT/AU subtype (approximately 57%) than in the non-AT/AU subtype (64%). Our findings are in line with sex differences reported for autoimmune disorders in general [29]. Furthermore, hair loss may be a greater social and emotional concern for women [30], leading to more frequent AA-related healthcare contacts among female than male patients [13]. However, some other studies have reported no female predominance in AA [5, 6]. This may be due to differences in data sources or due to true differences in the populations. The low prevalence of most comorbidities is expected given the age of the study population and capture of only hospital-based diagnoses by the data sources.
In our study, the annual prevalence of any AA increased over time by calendar year, with a larger increase observed for non-AT/AU. The incidence rate for AA overall remained relatively stable until an increase started in 2009. The reason for the time-related increases is unknown but has been reported previously in other studies [6, 10, 14, 34]. This finding could be due to an increase in the incidence of risk factors of AA, an increase in diagnostic activity due to increased awareness or more interactions with the healthcare system among individuals with AA [35]. For example, an increase in incidence over the last decades has been reported for many atopic and autoimmune diseases [36,37,38].
Limitations
In Denmark, AA is primarily diagnosed and treated in general practice, with only more severe cases leading to a hospital referral. Diagnoses from general practice are not captured in the Danish registries. This study focused on hospital-treated AA only, and their incidence and prevalence may be different in patients with AA not seen at hospitals. Furthermore, identification of the AA cohort based on hospital diagnoses has likely resulted in overrepresentation of AA cases that were severe enough to require a hospital encounter (inpatient stays or visits to hospital-based outpatient clinics) or occurred in individuals with other morbidities leading to hospital encounters. This could lead to selection bias whereby the population of this study differs from the total population of Danish patients with AA with respect to prevalence of comorbidities and distributions of other patient characteristics. We did not have information on the clinical course of AA, and prevalence estimates assume that none of the patients recovered from AA. Furthermore, data on outpatient dispensing were limited to reimbursed drugs and only available from 2004 onwards. Finally, DNPR diagnoses of AA have not been validated; however, the positive predictive value of diagnosis codes in the DNPR is typically around 80% [15, 18, 32].
Conclusion
This population-based cohort study provides estimates of increasing incidence and prevalence of all AA subtypes and the characteristics of patients with hospital-treated AA and its subtypes in Denmark in 1995–2016 but are likely underestimating the true incidence and prevalence.
Data Availability
The individual-level data used for these analyses cannot be shared under the current study permissions. Interested parties can apply for the source data from the data custodians at the Danish Health Data Authority.
References
Strazzulla LC, Wang EHC, Avila L, et al. Alopecia areata: disease characteristics, clinical evaluation, and new perspectives on pathogenesis. J Am Acad Dermatol. 2018;78(1):1–12.
Hordinsky MK. Overview of alopecia areata. J Investig Dermatol Symp Proc. 2013;16(1):S13-15.
MacLean KJ, Tidman MJ. Alopecia areata: more than skin deep. Practitioner. 2013;257(1764):29–32, 3.
National Alopecia Areata Foundation. 2022. https://www.naaf.org/faqs. Accessed 2022-05-07.
Villasante Fricke AC, Miteva M. Epidemiology and burden of alopecia areata: a systematic review. Clin Cosmet Investig Dermatol. 2015;8:397–403.
Mirzoyev SA, Schrum AG, Davis MDP, Torgerson RR. Lifetime incidence risk of alopecia areata estimated at 2.1% by Rochester Epidemiology Project, 1990–2009. J Investig Dermatol. 2014;134(4):1141–2.
Muntyanu A, Gabrielli S, Donovan J, et al. The burden of alopecia areata: a scoping review focusing on quality of life, mental health and work productivity. J Eur Acad Dermatol Venereol. 2023;37(8):1490–520.
Harries MJ, Sun J, Paus R, King LE Jr. Management of alopecia areata. BMJ. 2010;341:c3671.
Darwin E, Hirt PA, Fertig R, Doliner B, Delcanto G, Jimenez JJ. Alopecia areata: review of epidemiology, clinical features, pathogenesis, and new treatment options. Int J Trichol. 2018;10(2):51–60.
Lee JH, Kim HJ, Han KD, et al. Incidence and prevalence of alopecia areata according to subtype: a nationwide, population-based study in South Korea (2006–2015). Br J Dermatol. 2019;181(5):1092–3.
Harries M, Macbeth AE, Holmes S, et al. The epidemiology of alopecia areata: a population-based cohort study in UK primary care. Br J Dermatol. 2022;186(2):257–65.
Benigno M, Anastassopoulos KP, Mostaghimi A, et al. A large cross-sectional survey study of the prevalence of alopecia areata in the United States. Clin Cosmet Investig Dermatol. 2020;13:259–66.
Mostaghimi A, Gao W, Ray M, et al. Trends in prevalence and incidence of alopecia areata, alopecia totalis, and alopecia universalis among adults and children in a US employer-sponsored insured population. JAMA Dermatol. 2023;159:411–8.
Eaton WW, Rose NR, Kalaydjian A, Pedersen MG, Mortensen PB. Epidemiology of autoimmune diseases in Denmark. J Autoimmun. 2007;29(1):1–9.
Eaton WW, Pedersen MG, Atladottir HO, Gregory PE, Rose NR, Mortensen PB. The prevalence of 30 ICD-10 autoimmune diseases in Denmark. Immunol Res. 2010;47(1–3):228–31.
Laugesen K, Ludvigsson JF, Schmidt M, et al. Nordic health registry-based research: a review of health care systems and key registries. Clin Epidemiol. 2021;13:533–54.
Schmidt M, Pedersen L, Sørensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–9.
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–90.
Gjerstorff ML. The Danish Cancer Registry. Scand J Public Health. 2011;39(7 Suppl):42–5.
Helweg-Larsen K. The Danish register of causes of death. Scand J Public Health. 2011;39(7 Suppl):26–9.
Johannesdottir SA, Horvath-Puho E, Ehrenstein V, Schmidt M, Pedersen L, Sorensen HT. Existing data sources for clinical epidemiology: the Danish National Database of Reimbursed Prescriptions. Clin Epidemiol. 2012;4:303–13.
Hordinsky M, Hebert AA, Gooderham M, et al. Efficacy and safety of ritlecitinib in adolescents with alopecia areata: results from the ALLEGRO phase 2b/3 randomized, double-blind, placebo-controlled trial. Pediatr Dermatol. 2023;40:1003–9.
King B, Zhang X, Harcha WG, et al. Efficacy and safety of ritlecitinib in adults and adolescents with alopecia areata: a randomised, double-blind, multicentre, phase 2b–3 trial. Lancet. 2023;401(10387):1518–29.
Liu LY, King BA. Ruxolitinib for the treatment of severe alopecia areata. J Am Acad Dermatol. 2019;80(2):566–8.
Danmarks Statistik. https://www.statistikbanken.dk/statbank5a/default.asp?w=1920. Accessed 8 Apr 2024.
Egeberg A, Anderson S, Edson-Heredia E, Burge R. Comorbidities of alopecia areata: a population-based cohort study. Clin Exp Dermatol. 2021;46(4):651–6.
George P, Jagun O, Liu Q, et al. Prevalence of autoimmune and inflammatory diseases and mental health conditions among an alopecia areata cohort from a US administrative claims database. J Dermatol. 2023;50(9):1121–8.
Lien KH, Ger TY, Chi CC. Association of alopecia areata with sensorineural hearing loss: a systematic review and meta-analysis. Dermatology. 2023;239(4):523–32.
Ngo ST, Steyn FJ, McCombe PA. Gender differences in autoimmune disease. Front Neuroendocrinol. 2014;35(3):347–69.
Marks DH, Penzi LR, Ibler E, et al. The medical and psychosocial associations of alopecia: recognizing hair loss as more than a cosmetic concern. Am J Clin Dermatol. 2019;20(2):195–200.
Lundin M, Chawa S, Sachdev A, Bhanusali D, Seiffert-Sinha K, Sinha AA. Gender differences in alopecia areata. J Drugs Dermatol. 2014;13(4):409–13.
Andersen YMF, Nymand L, DeLozier AM, Burge R, Edson-Heredia E, Egeberg A. Patient characteristics and disease burden of alopecia areata in the Danish Skin Cohort. BMJ Open. 2022;12(2):e053137.
Uzuncakmak TK, Engin B, Serdaroglu S, Tuzun Y. Demographic and clinical features of 1,641 patients with alopecia areata, alopecia totalis, and alopecia universalis: a single-center retrospective study. Skin Appendage Disord. 2021;7(1):8–12.
Soh BW, Kim SM, Kim YC, Choi GS, Choi JW. Increasing prevalence of alopecia areata in South Korea. J Dermatol. 2019;46(9):e331–2.
Chubak J, Dalmat RR, Weiss NS, Doria-Rose VP, Corley DA, Kamineni A. Informative presence in electronic health record data: a challenge in implementing study exclusion criteria. Epidemiology. 2023;34(1):29–32.
Barahmani N, Schabath MB, Duvic M. History of atopy or autoimmunity increases risk of alopecia areata. J Am Acad Dermatol. 2009;61(4):581–91.
Lerner A, Patricia W, Matthias T. The world incidence and prevalence of autoimmune diseases is increasing. Int J Celiac Dis. 2015;3:151–5.
Thomsen SF. Epidemiology and natural history of atopic diseases. Eur Clin Respir J. 2015. https://doi.org/10.3402/ecrj.v2.24642.
Medical Writing and Editorial Assistance
Carolyn Maskin, PhD, provided medical writing and editorial assistance. This was provided by Nucleus Global and was funded by Pfizer Inc.
Funding
This study was supported by Pfizer Inc via institutional research funding to and administered by Aarhus University. The journal’s Rapid Service Fee was funded by Pfizer Inc.
Author information
Authors and Affiliations
Contributions
Sissel Brandt Toft Sørensen led the writing. Vera Ehrenstein, Oladayo Jagun, Prethibha George, and Samuel H. Zwillich conceived and designed the study. Vera Ehrenstein participated in acquisition of the data. All authors drafted the manuscript and revised it critically for important intellectual content. The authors thank Dr. Uffe Heide-Jørgensen for performing the statistical analysis for the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
At the time of study completion, Prethibha George and Oladayo Jagun were employees of Pfizer Inc and may hold stock or stock options in Pfizer Inc; Prethibha George has no current affiliation. Robert Wolk, Lynne Napatalung, and Samuel H. Zwilich are employees of and may hold stock or stock options in Pfizer Inc. All other authors are employees of their respective institutions.
Ethical Approval
According to Danish law, studies based exclusively on routinely collected registry data are exempt from ethical approval or informed consent. This study was reported to the Danish Data Protection Agency, via registration with Aarhus University, record number 2016-051-000001/serial number 605.
Additional information
Prior Presentation: This manuscript was previously presented at the 51st Annual European Society for Dermatological Research Meeting from September 28, 2022, to October 1, 2022, in Amsterdam, the Netherlands. Further information can be found at https://doi.org/10.26226/m.62fa009023ef91001a663ba3.
Oladayo Jagun: Affiliation at the time of the study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sørensen, S.B.T., George, P., Jagun, O. et al. The Epidemiology of Hospital-Treated Alopecia Areata in Denmark, 1995–2016. Dermatol Ther (Heidelb) 14, 993–1006 (2024). https://doi.org/10.1007/s13555-024-01145-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-024-01145-9