Abstract
Introduction
Topical treatments (TT) are widely used in psoriasis management. While psoriasis itself has been associated with diminished quality of life and mental well-being, the impact of TT remains underexplored. This study aimed to evaluate the burden of TT on the daily lives of patients with psoriasis, the convenience of the TT, and the choice criteria.
Methods
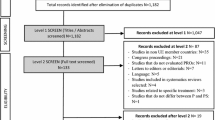
Patients were recruited across five countries (France, Germany, Italy, Spain, UK) by Wefight and the International Federation of Psoriasis Associations (IFPA) to complete a 29-item online survey.
Results
A total of 766 patients completed the survey (54% female, mean age of 53 years). The mean body surface area covered by psoriasis was 7%, predominantly on the scalp and elbows. Participants had been living with psoriasis for a mean duration of 18 years. Of the respondents, 34% reported feeling affected by their TT in their daily routines and activities. Those feeling affected were more likely to have a more complex disease, be using more treatments, or be diagnosed more recently compared to those less affected. Among those most affected by their TT, 27% reported a strong impact on mental health, 30% on sexual life, and 25% on physical activities, compared to 7%, 6% and 4% in those least affected, respectively. Both cohorts considered tolerability factors such as “does not cause itching/burning” and “good tolerability” as most important when choosing a topical. However, only least affected participants regarded convenience factors such as “does not run off,” “ease of application,” “does not leave stains” among others equally as important.
Conclusion
Overall, one-third of patients report a significant burden of TT on their daily lives. These patients have different criteria of choice, highlighting the importance of communication between physicians and patients to tailor treatment to individual preferences, thereby enhancing adherence and treatment outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Topical treatments (TT) are the mainstay of psoriasis management but their impact on the daily lives of patients is underexplored. |
The aim of this study was to evaluate the burden of TT on the daily lives of patients with psoriasis, the convenience of the TT, and criteria of choice. |
What was learned from this study? |
Around one-third of patients are more affected by their TT in their daily lives, particularly those with more complex disease, using more treatments, and those diagnosed more recently. |
Those most and least affected by their TT both considered tolerability most important when choosing a TT. Conversely, only those least affected regarded convenience as an important criterion. |
To improve adherence and treatment outcomes, physicians should consider patient needs and preferences when prescribing topical treatment. |
Introduction
Psoriasis is a chronic inflammatory skin disease that is estimated to affect up to 125 million people worldwide, up to one-third of whom will develop psoriatic arthritis [1,2,3]. The condition affects both males and females, although presentation often occurs earlier in females [4]. Additionally, prevalence varies between continents, ranging from 0.14% in East Asia to 1.99% in Australasia, with high rates in Western (1.92%) and Central (1.83%) Europe, as well as North America (1.50%) [1].
Treatments for psoriasis include topical treatments (TT) such as vitamin D analogues and corticosteroids, as well as phototherapy, systemic therapies such as methotrexate, cyclosporin, and acitretin, and biological therapies [4]. A TT can be used as a monotherapy, but is often used in combination with other TT to increase efficacy [4]. TT are recommended as a first-line intervention and are the most commonly used treatments for mild-to-moderate psoriasis (affecting < 10% of body surface area) [5, 6]. TT are also preferred for psoriasis that affects sensitive areas, such as the face, flexures, or genitals [6]. Although systemic therapy is recommended for moderate-to-severe psoriasis, many patients remain on TT, either alone or as a combination therapy [7].
Despite the widespread use of TT, several issues exist with these treatments. Firstly, treatment regimens often prove to be complicated and inconvenient, with longer daily treatment times negatively affecting patient quality of life (QoL) [8]. Patients can be deterred by drug formulation, particularly the smell, messiness, or aesthetics, or by side effects such as itching, burning, and dryness [9]. Finally, TT may not always meet the efficacy expectations of patients, leading to feelings of dissatisfaction [9]. These collective issues can contribute towards low primary and secondary adherence to treatment [10]. Previous research has reported suboptimal adherence rates to TT, with almost half of prescriptions going unfilled (primary adherence) and up to 95% not being used as prescribed (secondary adherence) [5, 11,12,13,14,15,16,17,18]. In patients who do fill their prescriptions, a median of just 35% of the recommended dose is used [13]. Given that adherence is one of the biggest barriers to treatment success, it is pertinent to improve patient adherence to TT [19].
Overall patient satisfaction plays a crucial role in adherence to TT, which ultimately affects treatment efficacy and patient QoL [20, 21]. Factors such as ability to lead a normal life, cost considerations, probability of benefit, and the duration of treatment collectively shape patient satisfaction [22]. Many patients are willing to make trade-offs among these factors to prioritize those most important to them [22]. Therefore, patient preferences should be considered when prescribing TT to optimize adherence and treatment outcomes [10, 23].
A second, relatively understudied area that may impact adherence is the burden of TT. The substantial burden of psoriasis itself is well-documented, with patients reporting feelings of stigmatization, a low satisfaction with life, and depressive symptoms [24,25,26]. The disease has also been associated with a severe deterioration in QoL as well as mental health disorders, including depression and anxiety [24, 27,28,29]. Regarding the burden of TT, Blome et al. previously reported the association between time required for treatment and reduced QoL [8]; however, the burden of TT on the daily lives of psoriasis patients has not been reported. Therefore, we sought to evaluate the overall burden of TT in patients with psoriasis, including the effect of the treatment on areas such as mental health, social life, and time management. Additionally, we aimed to understand whether the burden of TT influences patients’ criteria of choice. This evaluation was conducted through a patient survey, incorporating the criteria of choice described by Vasconcelos et al. with selected domains adapted for inclusion in our study [23].
Materials and Methods
Participant Recruitment
Participants from five European countries (France, Germany, Italy, Spain and UK) were recruited via the Wefight network and through the International Federation of Psoriasis Associations (IFPA). Recruitment took place between 27 January and 24 March 2023. To be eligible for the study, participants had to be at least 18 years of age, must have been diagnosed with psoriasis (with or without psoriatic arthritis), and must have used at least one TT within the last month.
Survey Design
Participants were invited to take part in a 10-min online survey containing 29 questions on their demographic and clinical characteristics, treatment satisfaction, criteria of choice, and impact on daily life (Electronic Supplementary Material 1).
Ethics
This research follows the European Pharmaceutical Market Research Association (EphMRA) code of conduct and, as such, does not require Clinical Research Ethics Committee or Independent Review Board approval. According to the General Data Protection Regulation (GDPR) guidelines, respondents gave voluntary, informed consent to data collection and use, based on a clear explanation of the purpose of the data collection and the use(s) to which the data will be put.
Statistical Analysis
Statistical significance between the averages of two groups was calculated using a Student’s t-test. The Z-test was used for proportions. Both tests were run using 95% confidence intervals. Derived importance was determined using a Shapley value regression between treatment association with criterion of choice as the independent variable and treatment satisfaction as the dependent variable.
Results
Participant Demographics
A total of 766 patients were recruited for the study, of whom 412 (53.7%) were female, 352 (46.0%) were male, and two (0.3%) were non-binary (Table 1). On a country basis, 152 participants were from France, 165 from Germany, 150 from Italy, 150 from Spain, and 149 from the UK. The mean age of participants was 53 (range 19–87) years, with the majority falling into the 45–54 years (24%), 55–64 years (25%), and 65+ (23%) age ranges.
The mean estimate for body surface area covered by psoriasis was 7%, and the mean number of affected body locations was 4.1, with many patients reporting psoriasis on the scalp (59%), elbows (48%), ears (29%), and knees (29%). Patients had been living with the disease for a mean duration of 18 years and were using a mean number of 2.1 treatments (topical in all and in some combined with systemic and/or phototherapy), with the majority of patients using topical creams (65%) and ointments (46%).
The main type of TT used by patients was corticosteroids (41%) followed by a combination of calcipotriol/betamethasone dipropionate (28%), and emollients (22%). More than one TT was used by 40% of participants. The main channel used by participants to seek information about their TT was healthcare professionals such as dermatologists or general practitioners (72%).
Burden of TT on All Patients
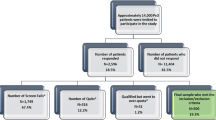
When participants were asked “Does the use of topical treatment affect your ability to take part in daily activities and routine?” around one-third (34%) answered “yes, to a great extent,” or “yes, somewhat” (Fig. 1a).
The burden of topical treatment (TT) on daily activities and routine (a) and other aspects of daily life (b). a Participants were asked “does the use of topical treatment affect your ability to take part in daily activities and routine?”. b Participants were asked to “rate each of the following criteria from 0 to 10, depending on the negative impact your topical treatments had on them in the past 4 weeks.” ST yes Sub-total of participants who answered “yes, to a great extent” or “yes, somewhat.” N = 766
The burden of TT on other areas of daily life was scored on a scale of 0 to 10, with 0–2 classed as none to low impact, 3–7 classed as slight to important impact, and 8–10 indicating a strong to very strong impact. For mental health, sexual life, physical activities, leisure activities, relationships with loved ones, and work life, between 9% and 14% of participants reported a strong to very strong impact of TT (Fig. 1b). Between 49% and 63% of participants reported no impact to low impact of TT on each of these areas.
When participants were asked more specific questions about the impact of their TT on mental health, 55% felt that their TT was noticeable to others (of whom 42% did not feel stigmatized and discriminated against and 13% did), 43% reported feeling different to others, and 19% had been mocked by a friend or colleague because their TT was noticeable (Fig. 2a). Regarding clothing, 42% have avoided wearing clothes they would like to wear, 40% have previously stained clothes or sheets because they did not wait long enough after applying the TT, and 37% reported that their TT influences the type of clothes they wear (Fig. 2b). Certain physical activities were impacted, with 41% of participants having experienced feeling stressed about going to the swimming pool and 26% being worried about taking part in sports (Fig. 2c). Participants reported that their social life was less impacted, with just 22% having declined a social event because they would not have time to get ready (Fig. 2d). The average time between applying TT and getting dressed was 9 min, with 81% of participants expressing satisfaction with this waiting time. When asked about time management, 17% had experienced being considered someone who is always late and 16% had experienced being late for work (Fig. 2e).
The burden of TT on specific areas of daily life. Participants were asked questions based on mental health (a), clothing (b), physical activities (c), social life (d), time management (e). ST yes Sub-total of participants who answered “yes, but I don’t feel stigmatized and discriminated against” or “yes, and I feel stigmatized and discriminated against” for “topical noticeable to others” and “yes, sometimes/somewhat” or “yes, many times/to a great extent” for all other questions. N = 766
When participants were asked “Have you ever had to stop using, use less, or change your TT because you felt that its application was not comfortable?”, almost one-third (29%) answered “yes” (Fig. 3). The top five reasons for doing this were “it was greasy” (34%), “it caused itching/burning” (29%), “it was not well absorbed” (21%), “skin was sticky after application” (20%), and “it was not easy/convenient to apply” (20%).
Proportion of participants who had previously stopped, decreased use of or changed TT (a) and their reasons (b). a Participants were asked “have you ever had to stop using, use less, or change your topical treatment because you felt that its application was not comfortable?” N = 766. b Participants that answered “yes” to the previous question were asked “when you think about the last time you stopped using/used less/switched because you felt that its application was not comfortable, what was (were) the main reason(s)?” N = 222
Burden of TT in Participants Most and Least Affected by Their Treatment in Their Daily Lives
Participants were grouped into most and least affected by their TT using their answer to “Does the use of topical treatment affect your ability to take part in daily activities and routine?” Those who answered “yes, to a great extent” or “yes, somewhat” (34%) were classed as most affected by their TT in their daily activities and routine, while those who answered “not so much” or “not at all” (66%) were classed as least affected by their TT in their daily activities and routine.
Of the participants least affected by their TT in their daily lives, 53% were female and 47% were male (Table 2). The mean time since diagnosis was 20 years. The mean body surface area covered by psoriasis was 4%, with the scalp (59%) and elbows (46%) being the most affected; all other areas were affected in one-quarter of patients or less. The mean number of treatments was 1.8, the majority being topical creams (61%) or ointments (42%). Only 9% of participants used oral treatments, 3% used biotherapy, and 3% used phototherapy.
The proportion of males and females most affected by their TT in their daily lives was 55% and 44%, respectively. These participants had a significantly lower mean time since diagnosis (15 years) and a significantly higher mean body surface area covered by psoriasis (13%). The scalp (59%) and elbows (50%) remained the most affected areas in this cohort, but the ears, hands, knees, and feet were also affected in 30–40% of these participants. This cohort also used a significantly higher mean number of treatments (2.7). Topical creams (73%) and ointments (53%) remained the most used treatments, but a significantly higher number of participants used oral treatments (21%), biotherapy (15%), and phototherapy (13%).
Participants who were most affected by their TT in their daily lives reported a significantly greater impact on various aspects of their life than those least affected (Fig. 4), including on their sexual life (30% vs. 6% with an 8 to 10 rating on a scale of 10, respectively) and their mental health (27% vs. 7% with an 8 to 10 rating, respectively). Of those most affected by their TT, 75% felt that their current treatment was noticeable to others, and 73% reported feeling different to others, compared to just 43% and 27% of those least affected by their TT, respectively. Regarding physical activities, 25% of those most affected by their TT reported a strong to very strong impact (8 to 10 rating), compared to 4% of those least affected by their TT. Of those most affected by their TT, 66% had experienced being stressed about going to the pool and 54% had experienced being worried about taking part in sports. Both impacts were significantly higher in this cohort than in the cohort of participants least affected by their TT, of whom 28% reported feeling stressed about going to the pool and 13% had felt worried about taking part in sports. Finally, when asked about clothing, 69% of those most affected by their TT avoided clothes that they would like to wear, compared to 28% of those least affected by their TT. Similarly, 64% of those most affected by their TT had experienced staining of their clothes because they did not wait long enough following application, compared to 29% of those least affected by their TT.
Comparison of TT burden in participants most and least affected by their TT in their daily lives. Participants were grouped based on their answer to “does the use of topical treatment affect your ability to take part in daily activities and routine?” Those who answered “yes, to a great extent” or “yes, somewhat” (34%) were classed as most affected by their TT in their daily activities and routine, while those who answered “not so much” or “not at all” (66%) were classed as least affected by their TT in their daily activities and routine. Their answers to questions on the burden of TT were then compared. Upwards arrow indicates significantly higher impact for patients most affected than for patients least affected (p < 0.05)
Drivers of Choice in all Participants
Stated importance of choice criteria was determined by asking participants “In your opinion, how important are each of the following criteria when choosing a topical treatment for your psoriasis? 10 means very important and 0 means not important at all.” The most important factor was that the TT “does not cause itching/burning” with 80% of participants scoring it at ≥ 8 (Fig. 5a), followed by “good tolerability” (79%), “does not run off” (74%), “does not leave stains on clothes and/or sheets” (73%), and “ease of application” (73%).
Stated importance (a) and derived importance (b) of criteria of choice when choosing TT. a Participants were asked “in your opinion, how important are each of the following criteria when choosing a topical treatment for your psoriasis? 10 means very important and 0 means not important at all.” b Participants were asked “overall, how satisfied are you with your current topical treatment?” and “please rate each of the following criteria from 0 to 10, depending on whether it applies to the topical treatment options you are currently using for your psoriasis. 10 means that it applies very well and 0 means it doesn’t apply at all.” Derived importance was then calculated using a Shapley value regression with criterion of choice as the independent variable and treatment satisfaction as the dependent variable. N = 766
We also calculated derived importance to identify additional factors that are important, but that the participant may not consciously recognize. Participants were asked “please rate each of the following criteria from 0 to 10, depending on whether it applies to the topical treatment options you are currently using for your psoriasis. 10 means that it applies very well and 0 means it doesn’t apply at all” and “overall, how satisfied are you with your current topical treatment?” The participants’ scores were then used to determine the relative contribution of each criterion to satisfaction.
The derived importance score for each criterion of choice adds up to a total of 100. The top three most important factors were “good moisturizing properties” (19), “good absorption” (10), and “does not cause itching/burning” (9) (Fig. 5b).
“Good absorption” and “does not cause itching/burning” were the only two criteria rated highly in both stated and derived importance, making them important key drivers of choice (Fig. 6). “Good moisturizing properties” was rated highly in derived importance but not stated importance, making it an unconscious driver of choice.
Key driver analysis of TT criteria of choice. Factors that are high in both stated and derived importance fall into the key drivers category. Those that are high in derived importance but low in stated importance fall into the unconscious drivers category. Those that are high in stated importance but low in derived importance are essential factors, while those that are low in both stated and derived importance are low priority
Drivers of Choice in Participants Most and Least Affected by Their TT in Their Daily Lives
Using stated importance, the top five criteria of choice in participants most affected by their TT in their daily lives were “does not cause itching/burning” (73%), “good tolerability” (72%), “does not leave stains on clothes and/or sheets” (67%), “good moisturizing properties” (66%), and “good absorption” (65%).
The top five criteria of choice in participants least affected by their TT in their daily life were “does not cause itching/burning” (84%), “good tolerability” (83%), “does not run off” (78%), “ease of application” (76%), and “does not leave stains on clothes and/or sheets” (76%).
These results show that all patients rate tolerability (i.e. “does not cause itching/burning” and “good tolerability”) as the most important criteria of choice regardless of how much their TT affects them in their daily lives. In those most affected by their TT, all other factors of choice were rated as important by < 70% of participants. Conversely, those least affected by their TT also rated convenience factors such as “does not run off,” “ease of application” and “does not leave stains” as highly important (Fig. 7).
Top five criteria of choice in participants most and least affected by their TT in their daily lives. Participants were grouped based on their answer to “does the use of topical treatment affect your ability to take part in daily activities and routine?” The stated importance of criteria of choice were then compared. Downwards arrow indicates significantly lower importance than the other group (p < 0.05). Upwards arrow indicates significantly higher importance than the other group (p < 0.05)
Discussion
The objective of this study was to evaluate the burden of TT on the daily lives of patients with psoriasis, the convenience of the TT, and criteria of choice. Our findings reveal that certain aspects of daily life are more affected by TT. For example, over 40% of participants expressed concerns that their TT was noticeable to others, that they felt different to others, that they felt stressed about going to the pool, and that they avoided clothes they would like to wear. Interestingly, while a significant proportion of participants reported feeling stressed about going to the pool, only around one-quarter expressed similar worries about taking part in other sports. This difference might stem from a greater sense of exposure during swimming, as opposed to other sports in which they can typically conceal their body and therefore their use of TT.
Fewer than 20% of participants reported instances of being late for work, being considered someone who is always late, being mocked by friends or colleagues, and feeling stigmatized and discriminated against. Notably, despite many participants feeling that their TT was noticeable to others and often feeling different from others, very few felt stigmatized and discriminated against, possibly because most participants had never encountered being mocked by friends or colleagues. A previous study demonstrated that lower level of social support is correlated with a higher level of perceived stigmatization [30]. Therefore, those who have never been mocked by those closest to them may feel comforted by their support network, lowering feelings of stigmatization even though they believe that their TT is noticeable.
Overall, two-thirds of patients with psoriasis reported little effect of their TT on their daily lives. Fewer than 15% of participants reported a strong effect on mental health, sexual life, physical activities, leisure activities, relationships, and work life. However, certain patient demographics are more affected, particularly those with a more recent diagnosis, higher body surface area covered with psoriasis, and those using multiple treatments. Patients with a larger surface area covered by psoriasis are more likely to have it in areas that are harder to conceal, leading them to believe that their TT is more noticeable to others. Similarly, those using a higher number of treatments may also feel that their TT is difficult to conceal and, as a result, may express concerns about participating in physical activities and avoiding clothes they want to wear. Exercise has long been associated with improved mental health [31], while clothing choice may have an impact on an individual’s self-esteem, making it unsurprising that these patients report a strong impact of TT on mental health.
It is well-established that psoriasis is linked to depression, anxiety, and suicide ideation [24, 27,28,29, 32]. However, the impact of TT in particular on mental health has been underexplored in previous studies. Our study reveals that 27% of those who feel affected by their TT also experience a strong impact on their mental health. Previous research has found that patients with severe disease, and consequently a lower QoL, are less likely to adhere to treatment [17]. Therefore, patients experiencing a strong impact on their mental health may also be less likely to adhere to TT, exacerbating the effect of the disease on QoL.
To improve adherence to TT, especially in those experiencing high treatment burdens, effective communication between the patient and healthcare provider is critical. This is supported by the observation that adherence increases 2 days prior to a physician visit and remains high for the following 2 days [33]. Therefore, regular follow-up visits may improve adherence and provide patients with the opportunity to voice any concerns about the burden of the TT or their treatment preferences.
To evaluate which properties of TT patients found important, we examined both stated and derived importance of tolerability and convenience measures and whether criteria of choice differed between those most and least affected by their TT.
For those most affected by their TT in their daily lives, tolerability factors were crucial, while convenience factors were of comparatively lesser importance. This may be explained by the observation that these patients are usually on more treatments, potentially already experiencing inconvenience and not regarding convenience factors as critical. Alternatively, these patients often have more complex disease and may be more willing to endure some inconvenience for a tolerable treatment that does not cause side effects or exacerbate their symptoms. Finally, the disease may already affect these patients’ lives, given its association with a lower QoL [24], therefore they may not consider inconvenience from their TT as a significant factor in comparison.
In patients who state that they are less affected in their daily lives, tolerability remains the most important factor, but convenience also holds significant weight when choosing a TT. For example, though the patient might not consciously consider it, factors like good moisturizing properties play a vital role in treatment choice. The significance of convenience in these patients may be explained by their lower disease severity, making them more willing to switch TT to find one that is both tolerable and convenient. Furthermore, if their disease has little effect on their daily lives, they are unlikely to choose a TT that would impact their lives. This is supported by Florek et al., who reported that patients wanted to lead a normal everyday life while on treatment and did not want treatments that were incompatible with their lifestyle [22].
Our findings align with those of van Cranenburgh et al., who assessed the importance of specific domains of satisfaction (i.e., efficacy, tolerability, convenience, communication, information, and organization). They found that, after efficacy, tolerability was the second most important domain, closely followed by convenience [34]. Therefore, when developing new TT, consideration should be given to convenience factors, in addition to the usual focus on safety and efficacy, to create an optimal product.
Previous research has found that patients are generally satisfied with the convenience of their TT [34,35,36]. However, patients treated with a TT monotherapy were less satisfied overall than those using a combination of topical corticosteroids and vitamin D analogues [36]. This suggests that there is still room for improvement in prescribing practices.
It is important to note that no single topical will meet the expectations of all patients with psoriasis. Armstrong et al. demonstrated that treatment goals vary by demographics, including age, gender, and disease severity [37]. While there were common goals between groups, such as having confidence in the therapy, those with lower disease severity rated “to get better skin quickly” as an important goal while those with a higher disease severity prioritized “to find a clear diagnosis and therapy.” Our finding that tolerability is most important in both groups, but that convenience plays a bigger role in patients who are less affected by their TT in daily life supports these findings.
Current treatment selection is often based on patient and psoriasis characteristics, rather than on a personalized approach [38, 39]. While personalization of biologic therapies is possible using biomarkers [38], the possibility of personalized approaches for TT has been understudied. Our findings suggest that patients exhibit strong preferences that vary based on perceived burden of treatment on their daily lives. Therefore, the personalization of TT may begin by considering the patient’s preferences alongside patient and disease characteristics to provide a holistic treatment approach [38, 39].
As reported in Okubo et al., misalignment in treatment goals occurs in over two-thirds of physician–patient pairs, meaning that effective communication is required to bridge the gap in treatment goals [40]. Before prescribing, physicians should ensure that the TT aligns with the patient’s treatment goals. They should also take into consideration unconscious drivers, particularly the importance of “good moisturizing properties.” This should help to improve overall patient satisfaction and adherence to TT, consequently improving treatment efficacy and QoL [20, 21].
Strengths and Limitations
The survey design used in our study allowed for easy data collection from five European countries. This makes the results more generalizable to the overall psoriasis population than if data were collected from a single country. Additionally, the survey considered many areas of QoL, providing a comprehensive view of the burden of TT on patients with psoriasis.
The multi-country approach of the study is limited by variations in how patients across different countries may perceive and interpret questions. For example, there may be disparities in the understanding of terms such as ‘biotherapy’ or patients may have placed importance on different factors when evaluating overall QoL. This difference in interpretation could potentially result in an inaccurate depiction of the overall picture. Future studies should ideally employ validated instruments to minimize the risk of misinterpretation between countries.
The study is also limited by the lack of neutral responses to questions such as “overall, how satisfied are you with your current topical treatment?” By removing the neutral option, we expected that patients would give more consideration to the question, but it could be the case that this may have affected the accuracy of the response, particularly for patients without strong opinions on the topic.
The online survey may introduce selection bias, as older patients are less likely to participate [41]. Therefore, we may not be able to generalize the data to older subsets of patients. Additionally, the dataset was entirely patient reported, so disease characteristics may be less reliable than if reported by a physician.
Conclusion
In this study we have demonstrated that two-thirds of patients with psoriasis are not affected by their TT in their daily lives. However, one-third of patients, including those diagnosed more recently, those with a higher body surface area covered by psoriasis, and those using more treatments, are more likely to feel affected by their TT. This subset of patients reports a strong impact of their TT on their mental health, sexual life, and physical activities. We have also shown that patients who are most affected by their TT prioritize tolerability of TT, while those who are less affected consider convenience factors as well. To increase patient satisfaction, and therefore adherence, physicians should consider patient needs and preferences prior to prescribing.
Data Availability
All data generated or analyzed during this study are included in this published article as supplementary information files.
Change history
30 May 2024
A Correction to this paper has been published: https://doi.org/10.1007/s13555-024-01168-2
References
Parisi R, Iskandar IYK, Kontopantelis E, Augustin M, Griffiths CEM, Ashcroft DM. National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study. BMJ. 2020;369:m1590.
National Psoriasis Foundation. Psoriasis statistics. 2022. https://www.psoriasis.org/psoriasis-statistics/. Accessed 20 Oct 2023.
Mease PJ, Gladman DD, Papp KA, et al. Prevalence of rheumatologist-diagnosed psoriatic arthritis in patients with psoriasis in European/North American dermatology clinics. J Am Acad Dermatol. 2013;69(5):729–35.
Raharja A, Mahil SK, Barker JN. Psoriasis: a brief overview. Clin Med (Lond). 2021;21(3):170–3.
Devaux S, Castela A, Archier E, et al. Adherence to topical treatment in psoriasis: a systematic literature review. J Eur Acad Dermatol Venereol. 2012;26(Suppl 3):61–7.
Torsekar R, Gautam MM. Topical therapies in psoriasis. Indian Dermatol Online J. 2017;8(4):235–45.
Horn EJ, Fox KM, Patel V, Chiou C-F, Dann F, Lebwohl M. Are patients with psoriasis undertreated? results of National Psoriasis Foundation survey. J Am Acad Dermatol. 2007;57(6):957–62.
Blome C, Simianer S, Purwins S, et al. Time needed for treatment is the major predictor of quality of life in psoriasis. Dermatology. 2010;221(2):154–9.
Tan X, Feldman SR, Chang J, Balkrishnan R. Topical drug delivery systems in dermatology: a review of patient adherence issues. Expert Opin Drug Deliv. 2012;9(10):1263–71.
Bewley A, Page B. Maximizing patient adherence for optimal outcomes in psoriasis. J Eur Acad Dermatol Venereol. 2011;25(Suppl 4):9–14.
Belinchón I, Rivera R, Blanch C, Comellas M, Lizán L. Adherence, satisfaction and preferences for treatment in patients with psoriasis in the European Union: a systematic review of the literature. Patient Prefer Adherence. 2016;10:2357–67.
Storm A, Andersen SE, Benfeldt E, Serup J. One in 3 prescriptions are never redeemed: primary nonadherence in an outpatient clinic. J Am Acad Dermatol. 2008;59(1):27–33.
Storm A, Benfeldt E, Andersen SE, Serup J. A prospective study of patient adherence to topical treatments: 95% of patients underdose. J Am Acad Dermatol. 2008;59(6):975–80.
Fouéré S, Adjadj L, Pawin H. How patients experience psoriasis: results from a European survey. J Eur Acad Dermatol Venereol. 2005;19(Suppl 3):2–6.
Brown KK, Rehmus WE, Kimball AB. Determining the relative importance of patient motivations for nonadherence to topical corticosteroid therapy in psoriasis. J Am Acad Dermatol. 2006;55(4):607–13.
Richards HL, Fortune DG, O’Sullivan TM, Main CJ, Griffiths CE. Patients with psoriasis and their compliance with medication. J Am Acad Dermatol. 1999;41(4):581–3.
Zaghloul SS, Goodfield MJD. Objective assessment of compliance with psoriasis treatment. Arch Dermatol. 2004;140(4):408–14.
Teixeira A, Teixeira M, Almeida V, et al. Does the vehicle matter? real-world evidence on adherence to topical treatment in psoriasis. Pharmaceutics. 2021;13(10):1539.
Alinia H, Moradi Tuchayi S, Smith JA, et al. Long-term adherence to topical psoriasis treatment can be abysmal: a 1-year randomized intervention study using objective electronic adherence monitoring. Br J Dermatol. 2017;176(3):759–64.
Carroll CL, Feldman SR, Camacho FT, Balkrishnan R. Better medication adherence results in greater improvement in severity of psoriasis. Br J Dermatol. 2004;151(4):895–7.
Puig L, Carrascosa JM, Belinchón I, et al. Adherence and patient satisfaction with topical treatment in psoriasis, and the use, and organoleptic properties of such treatments: a Delphi study with an expert panel and members of the Psoriasis Group of the Spanish Academy of Dermatology and Venereology. Actas Dermosifiliogr. 2013;104(6):488–96.
Florek AG, Wang CJ, Armstrong AW. Treatment preferences and treatment satisfaction among psoriasis patients: a systematic review. Arch Dermatol Res. 2018;310(4):271–319.
Vasconcelos V, Teixeira A, Almeida V, et al. Patient preferences for attributes of topical anti-psoriatic medicines. J Dermatolog Treat. 2019;30(7):659–63.
Kowalewska B, Cybulski M, Jankowiak B, Krajewska-Kułak E. Acceptance of Illness, satisfaction with life, sense of stigmatization, and quality of life among people with psoriasis: a cross-sectional study. Dermatol Ther (Heidelb). 2020;10(3):413–30.
Jankowiak B, Kowalewska B, Krajewska-Kułak E, Khvorik DF. Stigmatization and quality of life in patients with psoriasis. Dermatol Ther (Heidelb). 2020;10(2):285–96.
Zięciak T, Rzepa T, Król J, Żaba R. Stigmatization feelings and depression symptoms in psoriasis patients. Psychiatr Pol. 2017;51(6):1153–63.
Cohen BE, Martires KJ, Ho RS. Psoriasis and the risk of depression in the US population: National Health and Nutrition Examination Survey 2009–2012. JAMA Dermatol. 2016;152(1):73–9.
Dalgard FJ, Gieler U, Tomas-Aragones L, et al. The psychological burden of skin diseases: a cross-sectional multicenter study among dermatological out-patients in 13 European countries. J Invest Dermatol. 2015;135(4):984–91.
Wu JJ, Feldman SR, Koo J, Marangell LB. Epidemiology of mental health comorbidity in psoriasis. J Dermatol Treat. 2018;29(5):487–95.
van Beugen S, van Middendorp H, Ferwerda M, et al. Predictors of perceived stigmatization in patients with psoriasis. Br J Dermatol. 2017;176(3):687–94.
Taylor CB, Sallis JF, Needle R. The relation of physical activity and exercise to mental health. Public Health Rep. 1985;100(2):195–202.
Liang SE, Cohen JM, Ho RS. Psoriasis and suicidality: a review of the literature. Dermatol Ther. 2019;32(1): e12771.
Feldman SR, Camacho FT, Krejci-Manwaring J, Carroll CL, Balkrishnan R. Adherence to topical therapy increases around the time of office visits. J Am Acad Dermatol. 2007;57(1):81–3.
van Cranenburgh OD, de Korte J, Sprangers MAG, de Rie MA, Smets EMA. Satisfaction with treatment among patients with psoriasis: a web-based survey study. Br J Dermatol. 2013;169(2):398–405.
Finch T, Shim TN, Roberts L, Johnson O. Treatment satisfaction among patients with moderate-to-severe psoriasis. J Clin Aesthet Dermatol. 2015;8(4):26–30.
Ninosu N, Hoelker S, Kappenstein M, Buettner S, Peitsch WK, Schaarschmidt M-L. Treatment satisfaction of patients with psoriasis with topical therapy in a real-world setting: unmet need for higher effectiveness. J Dermatol Treat. 2023;34(1):2200570.
Armstrong A, Edson-Heredia E, Zhu B, et al. Treatment goals for psoriasis as measured by patient benefit index: results of a National Psoriasis Foundation survey. Adv Ther. 2022;39(6):2657–67.
Camela E, Potestio L, Fabbrocini G, Ruggiero A, Megna M. New frontiers in personalized medicine in psoriasis. Expert Opin Biol Ther. 2022;22(12):1431–3.
Camela E, Potestio L, Fabbrocini G, Pallotta S, Megna M. The holistic approach to psoriasis patients with comorbidities: the role of investigational drugs. Expert Opin Investig Drugs. 2023;32(6):537–52.
Okubo Y, Tsuruta D, Tang AC, et al. Analysis of treatment goal alignment between Japanese psoriasis patients and their paired treating physicians. J Eur Acad Dermatol Venereol. 2018;32(4):606–14.
Eysenbach G, Wyatt J. Using the internet for surveys and health research. J Med Internet Res. 2002;4(2): e13.
Acknowledgements
Medical Writing/Editorial Assistance
Medical writing assistance was provided by Lauren Owens and Anne Legendre. Funding for this support was provided by Almirall.
Funding
Funding for this study and the Rapid service fee was provided by Almirall.
Author information
Authors and Affiliations
Contributions
All authors contributed to study concept and design and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Anthony Bewley has served as a consultant to Abbvie, Almirall, Celgene, Galderma, Janssen, Leo Pharma, Lilly, Novartis, Sanofi, and UCB; has participated in advisory boards for Psoriasis Association, Changing Faces, ISG, and NES; has received grants from EADV and travel grants from Janssen, Leo Pharma and Almirall; has participated in guidelines committees of BAD; is working as an editor for the book Practical Psychodermatology, as president for ESDaP and as a chair for APPGOS. Lauren Hiribane was an employee of Wefight during the study. Jordi Galván is an employee of Almirall. Sicily Mburu has no individual conflict of interest and is an employee of IFPA. The authors report no other conflicts of interest in this work.
Ethical Approval
This research follows the European Pharmaceutical Market Research Association (EphMRA) code of conduct which outlines the European guidelines on market research and, as such, does not require Clinical Research Ethics Committee or Independent Review Board approval. According to the GDPR guidelines, respondents gave voluntary, informed consent to data collection and use, based on a clear explanation of the purpose of the data collection and the use(s) to which the data will be put.
Additional information
Original online version of this article was revised: Few text corrections, corrections to tables updated.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bewley, A., Hiribarne, L., Galván, J. et al. Burden of Topical Treatments in Psoriasis and Preferred Criteria of Choice: A Survey-Based Evaluation of Patients in Europe. Dermatol Ther (Heidelb) 14, 1497–1514 (2024). https://doi.org/10.1007/s13555-024-01132-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-024-01132-0