Abstract
Introduction
While multiple treatments are available for moderate to severe psoriasis, patient preferences are rarely systematically studied. This study aims to identify factors associated with choice of a new once-daily oral psoriasis treatment, elicit patient views on treatment characteristics, and rank treatment characteristics by importance.
Methods
This noninterventional, cross-sectional survey study, conducted from December 2021 to June 2022, recruited US adults with moderate to severe psoriasis. Demographics, clinical characteristics, and perspectives on psoriasis treatment were collected. Factors associated with the choice of a new oral treatment were identified using multivariable logistic regression analysis. Treatment characteristics and reasons for treatment choice were ranked using bivariate comparisons.
Results
The study included 882 participants [mean (standard deviation; SD) age, 45.7 (12.8) years; female, 67.7%; White, 74.9%]; 92.7% were currently receiving treatment [mean (SD) duration, 2.9 (4.8) years]. Half of participants rated their psoriasis symptoms over the past week as mild, very mild, or nonexistent; 36.5% as moderate; and 12.7% as severe or very severe. Most (66.5%) indicated willingness to start a new oral treatment; 65.0% indicated that the new oral treatment would cause less anxiety than injections/infusions. Participants were significantly more likely to start the new oral treatment if they were currently receiving a tumor necrosis factor inhibitor [odds ratio (OR): 2.1, 95% confidence interval (CI): 1.4–3.1] or ustekinumab (OR: 2.7, 95% CI: 1.6–5.0) versus apremilast (P < 0.001) or if they reported mild (OR: 3.2, 95% CI: 2.0–4.9), moderate (OR: 5.0, 95% CI: 3.1–8.2), or severe (OR: 7.6, 95% CI: 3.9–15.0) psoriasis symptoms compared with those who reported no symptoms in the past week (P < 0.001).
Conclusion
Most participants indicated willingness to start a new once-daily oral treatment, viewing it as less anxiety provoking than injections/infusions. Current treatment and psoriasis severity affected participants’ willingness to start a new oral treatment.
Plain Language Summary
Patients with psoriasis have multiple treatment options available to them. We surveyed 882 adults with moderate to severe psoriasis in the US to assess their perspectives and the values placed on treatment characteristics that are most important to them when making treatment-related decisions. Participants were assigned to one of five groups based on their psoriasis treatment at the time of the survey: (1) apremilast (oral), (2) a tumor necrosis factor inhibitor (TNFi) treatment (injectable), (3) ustekinumab (injectable), (4) a topical therapy or phototherapy, or (5) over-the-counter medications or participants who were untreated (this group included those who were not currently using a psoriasis treatment). The extent of skin clearance associated with a drug, how a drug is taken, and a drug’s safety profile were among the top-ranked treatment characteristics that are important to survey participants when they choose a psoriasis treatment. Most participants (66.5%) were willing to start a new oral treatment, with 65.0% indicating that the new oral treatment would cause less anxiety than injections or infusions. Participants were more willing to switch to a new oral psoriasis treatment if they were currently receiving an injectable treatment, such as ustekinumab or a TNFi, compared with those who were already taking an oral treatment. These findings suggest that, when prescribing treatments for psoriasis, health care providers should consider the treatment characteristics that are important to their patients and consider that patients generally prefer an oral versus injectable drug.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Several treatments are available for moderate to severe psoriasis, each with specific efficacy, risks, and burden that can influence patients’ treatment decisions. |
This study aimed to identify factors associated with the choice of a new once-daily oral psoriasis treatment, to elicit patient views on treatment characteristics, and to rank treatment characteristics by their importance to patients. |
What was learned from the study? |
Most participants indicated a willingness to start a new once-daily oral treatment, viewing it as provoking less anxiety than treatment requiring injections/infusions, although this willingness was affected by participants’ current treatment and their degree of psoriasis severity. |
Clinical practice should consider the treatment characteristics that are important to patients and take note of a patient’s extent of fear or anxiety related to injectable treatments (reported by > 60% of participants across various treatment groups). |
Our findings suggest that effective oral treatments should be an important focus for future psoriasis care. |
Introduction
Psoriasis is a chronic, immune-mediated condition commonly characterized by scaly plaques on the skin that may cause pain, irritation, and itching [1, 2]. The disease has a large impact on patients’ quality of life (QoL) [3], specifically on patients’ physical, emotional, and social QoL [4, 5]. In the US, > 7.5 million individuals currently live with psoriasis [6], with plaque psoriasis accounting for 80% to 90% of cases [1]. Patients with psoriasis have an increased chance of developing comorbidities such as psoriatic arthritis (PsA), cardiovascular disease, diabetes, depression, or metabolic syndrome [7].
Psoriasis treatments include topical therapies, phototherapy, biologics, and nonbiologic systemic therapies. Topical therapies, considered first-line therapy for patients with mild disease, are used for local treatment of the skin. These include corticosteroids, vitamin D analogs, calcineurin inhibitors, keratolytics, and retinoids that patients apply in the form of creams or ointments directly to affected areas [1]; novel nonsteroidal topical treatments include tapinarof and roflumilast [8]. Phototherapy, or light therapy, is conducted under medical supervision and involves patients regularly exposing their skin to ultraviolet light [1]. For patients with moderate to severe psoriasis, treatments may include systemic therapies in addition to topical treatments [1]. Biologics are administered via subcutaneous injection or intravenous infusion, whereas nonbiologic systemic treatments can be administered orally [1]. Biologics include interleukin (IL)-12 and IL-23 inhibitors, IL-17 inhibitors, IL-23 inhibitors, and tumor necrosis factor inhibitors (TNFis) [1]. Nonbiologic systemic therapies include nontargeted agents, such as methotrexate, cyclosporine, and acitretin, as well as the targeted small-molecule treatments apremilast, a phosphodiesterase-4 inhibitor, and deucravacitinib, an allosteric tyrosine kinase 2 (TYK2) inhibitor [1, 9, 10].
While many treatment options are available for patients with psoriasis, current evidence highlights areas of unmet need, including a lack of alignment between patients’ and dermatologists’ perceptions of treatment options and disease burden [11]. A gap exists in the literature regarding patients’ preferences about treatment, which are driven by their treatment experiences and are important for health care providers to consider in their clinical decision-making [12]. For example, psoriasis studies have found that treatment-related characteristics, such as magnitude of response, probability of response, process attributes (such as frequency or mode of administration), and cost, are important to patients when they make treatment decisions [12,13,14,15]. It is, therefore, of clinical importance to understand how patient preferences drive treatment choice and how this choice varies by the type of treatment a patient currently receives.
The primary objective for this survey study was to identify patient factors associated with the choice of a new once-daily oral psoriasis treatment. The secondary objectives were to rank patients’ reasons for the choice of a new oral psoriasis treatment, assess the prevalence of anxiety related to injections or infusions, and elicit views on treatment characteristics in patients with moderate to severe psoriasis.
Methods
Study Design and Sample
This was a noninterventional, cross-sectional survey study conducted from December 14, 2021, through June 7, 2022, in adult participants with moderate to severe psoriasis in the US. A convenience sample of participants was recruited for the study by Global Perspectives through a panel and through ad hoc teams, using Global Perspectives’ databases. Respondents were eligible if they had a self-reported physician’s diagnosis of moderate or severe psoriasis, were ≥ 18 years of age, resided in the US, and were able to read and understand English. Respondents were ineligible to participate if they self-reported a physician’s diagnosis of mild psoriasis. Participants were assigned to predefined groups based on their treatment at the time of the survey: apremilast (oral), TNFi treatments (injectable), ustekinumab (an injectable IL-12/23 inhibitor), topical therapy or phototherapy, or over the counter (OTC)/untreated (this group included those who were using an OTC treatment, who were not currently receiving psoriasis treatment, or who received treatment in the past but had stopped). The TNFi group included participants receiving certolizumab pegol, etanercept, adalimumab, or infliximab. Any participants who did not fit into these categories were ineligible to participate (e.g., patients receiving secukinumab, brodalumab, ixekizumab, tildrakizumab, or guselkumab). The study protocol, survey, and relevant recruitment materials were evaluated by the RTI institutional review board (RTI Health Solutions; Research Triangle Park, NC) and deemed exempt. This survey study was conducted in accordance with the ethical principles of the Declaration of Helsinki. Participants who were deemed eligible after answering the survey’s screening questions were required to provide electronic consent via a checkbox.
Survey
A targeted literature review was conducted to identify relevant survey concepts, which were then reviewed by experts on the study team. Participants who provided electronic consent were prompted to continue to the survey, which constituted questions about demographics, clinical history, and treatment experiences and preferences. Participants were asked to self-report psoriasis severity over the past week on a 6-point scale from “none” to “very severe,” to indicate their body surface area involvement (BSA) using the 1% hand test [13], to report the frequency of flare-ups in the past 3 months, and to indicate the regions of their body affected by psoriasis.
To assess what treatment characteristics patients value, participants were asked to rank the following characteristics in order of importance: route of administration, dosing frequency, extent of skin clearance, safety profile of treatments, laboratory monitoring requirements, and durability of response. In addition, the survey assessed participants’ views on oral treatments. Participants were presented with a vignette (Fig. 1) describing a hypothetical new once-daily oral psoriasis treatment, including information on treatment administration, efficacy, potential nonserious adverse events, laboratory testing requirements, and out-of-pocket costs. After reviewing the treatment profile, participants were asked to report their expectations around (1) the treatment’s interference with daily life, (2) treatment convenience, (3) anxiety related to treatment, and (4) likelihood to start treatment. Questions about the new oral psoriasis treatment were not asked of participants who had received treatment in the past but who were not currently receiving treatment.
Data Collection
A soft launch of the survey (n = 111) was performed to test the electronic data collection system to determine whether any data collection or programming issues existed prior to full launch. The soft launch data were reviewed, and no adjustments to survey content were made. The survey was programmed and hosted on a secure web-based data collection platform, Qualtrics, which is encrypted and is compliant with the Health Insurance Portability and Accountability Act (HIPAA).
Data Management and Analyses
Survey data were de-identified prior to analysis. For the primary objectives of the study, multivariable logistic regression analysis was conducted to identify which patient factors were associated with the choice of a new oral psoriasis treatment for participants with moderate to severe psoriasis who were using apremilast, TNFi treatments, ustekinumab, or topical therapies and for those in the OTC/untreated group, excluding those who had previously used treatment but were not currently receiving treatment, controlling for participant demographics and clinical characteristics. These potentially associated factors included treatment group; age group; sex; race; Hispanic, Latino, or Spanish ethnicity; psoriasis severity; number of comorbidities of interest; disease duration; treatment duration; baseline PsA; number of flare-ups; and number of body regions affected. Comorbidities of interest included PsA, cardiovascular disease (heart attack, congestive heart failure, or cardiomyopathy), high blood pressure (hypertension), high cholesterol, metabolic syndrome, obesity, type 1 diabetes, type 2 diabetes, inflammatory bowel disease (ulcerative colitis or Crohn’s disease), depression, anxiety, cancer/malignancy, cerebrovascular disease (stenosis, thrombosis, embolism, hemorrhage, or stroke), peripheral vascular disease, and/or uveitis.
For the secondary objectives, bivariate comparisons were conducted to rank reasons for the choice of psoriasis treatment and to compare results across treatment groups. For ranking of treatment characteristics, bivariate comparisons were also conducted across a 6-point severity scale ranging from “none” (no psoriasis symptoms) to “very severe” for psoriasis symptoms over the past week. In addition, bivariate comparisons were conducted to assess the prevalence and extent of anxiety related to injections or infusions and to compare views on a new oral psoriasis treatment of participants in the different treatment groups.
For categorical variables, such as sex and race, frequency and percentage distributions were reported. Statistical comparisons were conducted between cohorts using Pearson chi-square tests or Fisher’s exact tests when any cell size was < 5. For continuous variables, such as age and treatment duration, the mean, standard deviation (SD), median, and ranges were reported.
Results
Participants
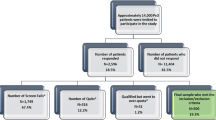
In total, 1236 respondents accessed the survey link, of whom 882 were eligible and completed the survey (Fig. 2). Participants’ mean age was 45.7 (SD, 12.8) years, and the majority were female (67.7%) and White (74.9%) (Table 1). One fifth (n = 179; 20.3%) of participants had PsA (Table S1 in Supplementary Material).
Participants reported being diagnosed with psoriasis for a mean (SD) of 14.9 (11.8) years, while they reported being on psoriasis treatment for a mean of 2.9 years (4.8) years. On average, participants reported 4.5 (11.00) flare-ups of their psoriasis symptoms over the previous 3 months, including the return or worsening of plaques and itch.
At the time of the survey, 818 (92.7%) of the 882 participants were receiving treatment, 47 (5.3%) had received treatment in the past but had stopped, and 17 (1.9%) had never received treatment for their psoriasis. The apremilast (oral) treatment group comprised 344 participants (39.0%), the TNFi group 242 (27.4%), the ustekinumab group 98 (11.1%), the topical therapy/phototherapy group 98 (11.1%), and the OTC/untreated group 100 (11.3%). The OTC/untreated group constituted participants who were receiving treatment with OTC/nonprescription medications (n = 36, 36.0%), who had never received treatment (n = 17, 17.0%), or who had received treatment in the past but had stopped (n = 47, 47.0%).
Choice of a New Oral Psoriasis Treatment
Of the 835 participants who were receiving treatment or had never received treatment, most (66.5%) were willing to start the new oral psoriasis treatment (Table 2). Of the 17 participants who had never received treatment, 88.2% were willing to start a new oral psoriasis treatment compared with 80.6% of OTC treatment users, 75.5% of ustekinumab users, 74.0% of TNFi users, 69.4% of topical therapy users, and 55.2% of apremilast users (P < 0.001).
When asked if they expected that the treatment would be convenient to take, 83.7% of participants responded “yes, definitely” or “probably yes” (Table 3). Additionally, 65.1% responded “yes, definitely” or “probably yes” when asked if the treatment would cause less anxiety than an injection or infusion, and 55.4% of the participants said “yes, definitely” or “probably yes” to a question about whether the new treatment would interfere less with their everyday life compared with their current treatment. Half of participants (50.1%) expected that the new oral psoriasis treatment would reduce their symptoms more than their current treatment.
The multivariable stepwise logistic regression analysis (Table 4) showed that participants receiving injectable TNFi treatments or ustekinumab were more likely to start a new oral psoriasis treatment compared with those receiving apremilast, also an oral treatment [TNFi odds ratio (OR), 2.1, 95% confidence interval (CI), 1.4–3.1, P < 0.001; ustekinumab OR, 2.7, 95% CI, 1.6–4.6, P < 0.001]. Participants who self-identified as Black were more likely to start a new oral psoriasis treatment compared with those who identified as White (OR, 2.4, 95% CI, 1.4–4.2, P = 0.002). Compared with participants reporting no psoriasis symptoms or signs over the past week, those who experienced mild, moderate, or severe psoriasis symptoms in the previous 7 days were more likely to start a new oral psoriasis treatment (mild symptoms: OR: 3.2, 95% CI, 2.0–4.9, P < 0.001; moderate symptoms: OR: 5.0, 95% CI, 3.1–8.2, P < 0.001; and severe symptoms: OR, 7.6, 95% CI, 3.9–15.0, P < 0.001).
Treatment Characteristics of Importance
Among all 882 participants, the extent of skin clearance, route of administration, safety profile of treatments, and dosing frequency were the top-ranked treatment characteristics deemed important to participants (Fig. 3). More than one third (37.1%) ranked the extent of skin clearance as the most important treatment characteristic, and approximately half (53.0%) ranked laboratory monitoring as the least important. Rankings did not vary greatly between the treatment groups (Fig. 4). The most notable difference was that a greater proportion of participants in the OTC/untreated and topical therapy/phototherapy groups ranked the safety profile of treatments as the most important treatment characteristic compared with the apremilast, TNFi treatment, and ustekinumab groups.
Ranking was also assessed across all psoriasis severity levels (“none,” “very mild,” “mild,” “moderate,” “severe,” or “very severe”). The ranking results were similar across severity levels in that the three highest-ranking characteristics were the same (extent of skin clearance, route of administration, and safety); however, they differed in rank order (Fig. 5). Participants who reported no psoriasis symptoms in the past week ranked route of administration as the most important treatment characteristic that they consider when choosing a new psoriasis treatment.
Prevalence of Anxiety Related to Injections or Infusions
Participants receiving an injectable treatment for their psoriasis (TNFi treatments or ustekinumab) at the time of the survey and participants who had received such treatment in the past were asked to assess their treatment-related anxiety. Among 340 current users of a TNFi or ustekinumab, 219 (64.4%) reported experiencing anxiety when receiving or self-administering an injection or infusion for their psoriasis, while 121 (35.6%) did not (Table 5). In the TNFi group (n = 242), 159 (65.7%) reported experiencing anxiety when receiving or self-administering an injection/infusion for their psoriasis, while in the ustekinumab group (n = 98), 60 (61.2%) experienced anxiety. Among six past users of TNFi treatments, five (83.3%) reported experiencing anxiety when receiving or self-administering an injection or infusion for their psoriasis treatment. No past users of ustekinumab were included in the sample.
Discussion
This study highlights the treatment characteristics most important to patients when choosing a new psoriasis treatment and explores how different patient factors affect patients’ views of these characteristics, as related to oral treatments. This study also investigated the extent of anxiety related to injections or infusions and the degree to which it differs between patients using different treatments. While previous studies have assessed treatment characteristics important to patients’ decision-making [16, 17] and treatment preferences [13, 18,19,20,21], few have analyzed patient factors affecting patients’ views on treatments or the extent of anxiety related to injections or infusions in this population. A strength of the current study is that it explored, through the patients’ perspective, which clinical factors and treatment characteristics affect patients’ views on psoriasis treatments.
The demographics and clinical characteristics of participants in this survey were similar to the findings of other studies in this disease space [21, 22] and were generally representative of the population of patients with moderate to severe psoriasis. Almost all of the participants in our study were on treatment at the time of the survey, and the average duration of psoriasis (14.9 years) resembles that seen in other cross-sectional studies in patients with moderate to severe psoriasis [18, 21, 23].
Like other studies in patients with moderate or severe psoriasis, our study found that patients value treatment efficacy over other treatment characteristics [19, 21]. Our findings also show that the relative importance of treatment characteristics varies depending on disease severity, results that are similar to those of other preference studies [12, 13, 15].
Our study identified route of administration as an important treatment characteristic for patients. A large percentage of participants (64.4%) currently on an injectable treatment reported that they felt anxious when receiving it. While few cross-sectional studies have assessed patient-reported anxiety related to injections or infusions, studies have shown that injection-related anxiety is related to treatment nonadherence in patients with other inflammatory diseases requiring injectable therapies [24, 25]. In a study conducted by Murray et al., health care providers indicated that needle phobia plays a role in some patients’ preference for oral treatments [26]. Notably, our results also show that patients are more willing to switch to a new oral psoriasis treatment if they are currently on injectable treatments, such as ustekinumab or a TNFi, compared with those already on oral treatments. This finding is novel because it shows that even among patients receiving infrequent biologic injections, such as ustekinumab, many are willing to switch to a new oral therapy. These findings suggest that clinicians should consider patient preference for oral treatments when prescribing treatments for psoriasis.
This large, real-world survey study provides an account of how patients’ treatment experience and the impact of psoriasis, including disease severity and comorbidities, play a role in treatment choice. The large sample size of individuals with moderate to severe psoriasis allows for statistical comparisons between the different treatment groups and increases the generalizability of the results. Certain limitations should be considered when interpreting these results. Because this is a survey study, participants were asked to self-report their treatment history, diagnosis, and disease severity. In addition, the individuals who choose to participate in an online panel may differ in terms of their characteristics and experiences from those who did not choose to be included on such a panel. However, the demographics of this panel of survey participants are similar to those in the real world. Lastly, the survey was conducted before the approval of deucravacitinib and did not include biologics such as secukinumab, brodalumab, ixekizumab, tildrakizumab, or guselkumab; therefore, the treatments represented in the analysis do not reflect the full therapeutic armamentarium currently available. Inclusion of second-generation biologics with a low frequency of administration but with a favorable benefit/risk profile may impact the ranking of treatment attributes and patient preference for the new, once-daily oral treatment. Interpretation of results should be limited to patients who would be potential users of oral treatments or first-generation biologics, such as a TNFi or ustekinumab.
Conclusion
Overall, this study provides a detailed report of perspectives, views, and values on treatment characteristics that are most important to patients when making treatment-related decisions. Extent of skin clearance, route of administration, and safety profile were among the top-ranked treatment characteristics important to patients when they are choosing a psoriasis treatment. Clinical practice should consider the treatment characteristics that are important to patients and take note of the extent of anxiety related to injections or infusions. Our results suggest that effective oral treatments should be an important focus for future psoriasis care.
Data Availability
The Bristol Myers Squibb policy on data sharing may be found at https://www.bms.com/researchers-and-partners/independent-research/data-sharing-request-process.html.
References
Armstrong AW, Read C. Pathophysiology, clinical presentation, and treatment of psoriasis: a review. JAMA. 2020;323(19):1945–60.
Bakshi H, Nagpal M, Singh M, Dhingra GA, Aggarwal G. Treatment of psoriasis: a comprehensive review of entire therapies. Curr Drug Saf. 2020;15(2):82–104.
Griffiths CEM, Jo SJ, Naldi L, Romiti R, Guevara-Sangines E, Howe T, et al. A multidimensional assessment of the burden of psoriasis: results from a multinational dermatologist and patient survey. Br J Dermatol. 2018;179(1):173–81.
Korman NJ, Zhao Y, Pike J, Roberts J. Relationship between psoriasis severity, clinical symptoms, quality of life and work productivity among patients in the USA. Clin Exp Dermatol. 2016;41(5):514–21.
Armstrong AW, Schupp C, Wu J, Bebo B. Quality of life and work productivity impairment among psoriasis patients: findings from the National Psoriasis Foundation survey data 2003–2011. PLoS ONE. 2012;7(12): e52935.
Armstrong AW, Mehta MD, Schupp CW, Gondo GC, Bell SJ, Griffiths CEM. Psoriasis prevalence in adults in the United States. JAMA Dermatol. 2021;157(8):940–6.
Elmets CA, Leonardi CL, Davis DMR, Gelfand JM, Lichten J, Mehta NN, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities. J Am Acad Dermatol. 2019;80(4):1073–113.
Del Toro NP, Wu JJ, Han G. New treatments for psoriasis: an update on a therapeutic frontier. Cutis. 2023;111(2):101–4.
Armstrong A, Xia Q, John AR, Patel V, Seigel L. Treatment patterns for targeted therapies, non-targeted therapies, and drug holidays in patients with psoriasis. Dermatol Ther (Heidelb). 2022;12(9):2087–103.
Sotyktu [package insert]. Princeton: Bristol-Myers Squibb Company; 2022.
Lebwohl M, Langley RG, Paul C, Puíg L, Reich K, van de Kerkhof P, et al. Evolution of patient perceptions of psoriatic disease: results from the understanding psoriatic disease leveraging insights for treatment (UPLIFT) survey. Dermatol Ther (Heidelb). 2022;12(1):61–78.
Florek AG, Wang CJ, Armstrong AW. Treatment preferences and treatment satisfaction among psoriasis patients: a systematic review. Arch Dermatol Res. 2018;310(4):271–319.
Alcusky M, Lee S, Lau G, Chiu GR, Hadker N, Deshpande A, et al. Dermatologist and patient preferences in choosing treatments for moderate to severe psoriasis. Dermatol Ther (Heidelb). 2017;7(4):463–83.
Schaarschmidt ML, Schmieder A, Umar N, Terris D, Goebeler M, Goerdt S, et al. Patient preferences for psoriasis treatments: process characteristics can outweigh outcome attributes. Arch Dermatol. 2011;147(11):1285–94.
Schaarschmidt ML, Herr R, Gutknecht M, Wroblewska K, Gerdes S, Sticherling M, et al. Patients’ and physicians’ preferences for systemic psoriasis treatments: a nationwide comparative discrete choice experiment (PsoCompare). Acta Derm Venereol. 2018;98(2):200–5.
Tan J, Stacey D, Fung K, Barankin B, Bissonnette R, Gulliver W, et al. Treatment decision needs of psoriasis patients: cross-sectional survey. J Cutan Med Surg. 2010;14(5):233–9.
Kim J, Kim DJ, Ortenzio FS, Dare L, Frank C, Kost RG, et al. Patients with psoriasis and personalized trade-offs in treatment decisions—lessons learned from focus groups. JAMA Dermatol. 2016;152(6):720–2.
Feldman SR, Moeller AH, Idemyr STE, Gonzalez M. Relative importance of mode of administration in treatment preferences among plaque psoriasis patients in the United States. J Health Econ Outcomes Res. 2016;4(2):141–57.
Gorelick J, Shrom D, Sikand K, Renda L, Burge R, Dworkin C, et al. Understanding treatment preferences in patients with moderate to severe plaque psoriasis in the USA: results from a cross-sectional patient survey. Dermatol Ther (Heidelb). 2019;9(4):785–97.
Gonzalez JM, Johnson FR, McAteer H, Posner J, Mughal F. Comparing preferences for outcomes of psoriasis treatments among patients and dermatologists in the U.K.: results from a discrete-choice experiment. Br J Dermatol. 2017;176(3):777–85.
Feldman SR, Poulos C, Gilloteau I, Mange B, Boehm K, Boeri M, et al. Exploring determinants of psoriasis patients’ treatment choices: a discrete-choice experiment study in the United States and Germany. J Dermatol Treat. 2022;33(3):1511–20.
Armstrong AW, Robertson AD, Wu J, Schupp C, Lebwohl MG. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation surveys, 2003–2011. JAMA Dermatol. 2013;149(10):1180–5.
Feldman SR, Mathias SD, Schenkel B, Colwell HH, McQuarrie K, Randazzo B, et al. Development of a patient-reported outcome questionnaire for use in adults with moderate-to-severe plaque psoriasis: the Psoriasis Symptoms and Signs Diary. J Dermatol Dermatol Surg. 2016;20(1):19–26.
Washington F, Langdon D. Factors affecting adherence to disease-modifying therapies in multiple sclerosis: systematic review. J Neurol. 2022;269(4):1861–72.
Turner AP, Williams RM, Sloan AP, Haselkorn JK. Injection anxiety remains a long-term barrier to medication adherence in multiple sclerosis. Rehabil Psychol. 2009;54(1):116–21.
Murray S, Crowley J, Gooderham MJ, Kivitz A, Chandran V, Péloquin S, et al. Healthcare providers face numerous challenges in treating patients with psoriasis: Results from a mixed-methods study. J Psoriasis Psoriatic Arthritis. 2022;7(1):35–43.
Acknowledgements
The authors thank the participants of the study and thank Global Perspectives for their assistance in participant recruitment and in hosting the survey.
Medical Writing, Editorial, and Other Assistance
Medical writing assistance was provided by Beth Lesher, PharmD, BCPS, and Catherine Mirvis, BA, of OPEN Health Evidence & Access and funded by Bristol Myers Squibb. Debdeep Chattopadhyay, PhD, and Marieke Heisen, PhD, of OPEN Health Evidence & Access provided critical review of the manuscript.
Funding
This study was sponsored by Bristol Myers Squibb, which also funded the journal’s Rapid Service Fee.
Author information
Authors and Affiliations
Contributions
April W. Armstrong, Sayeli Jayade, Sanika Rege, Namita Joshi, Vardhaman Patel, Samaneh Kalirai, Daniel Wolin, Kimberly Boyle, Dipen Patel, and Lauren Seigel contributed to the study design. Sayeli Jayade, Sanika Rege, Namita Joshi, Daniel Wolin, and Kimberly Boyle participated in data analysis. April W. Armstrong, Sayeli Jayade, Sanika Rege, Namita Joshi, Vardhaman Patel, Samaneh Kalirai, Daniel Wolin, Kimberly Boyle, Dipen Patel, and Lauren Seigel had full access to the data and contributed to data interpretation and to the drafting, critical review, and revision of the manuscript, with the support of medical writers provided by Bristol Myers Squibb. April W. Armstrong, Sayeli Jayade, Sanika Rege, Namita Joshi, Vardhaman Patel, Samaneh Kalirai, Daniel Wolin, Kimberly Boyle, Dipen Patel, and Lauren Seigel granted approval of the final manuscript for submission.
Corresponding author
Ethics declarations
Conflict of Interest
April W. Armstrong is a research investigator, scientific advisor, and/or speaker for AbbVie, Almirall, Arcutis, ASLAN, Beiersdorf, Boehringer Ingelheim, Bristol Myers Squibb, Dermavant, Dermira, EPI, Incyte, Janssen, Leo, Lilly, Mindera Health, Nimbus, Novartis, Ortho Dermatologics, Pfizer, Regeneron, Sanofi, Sun Pharma, and UCB. April W. Armstrong was an employee of University of Southern California at the time of this study. She is currently an employee of the University of California Los Angeles, Los Angeles, CA, USA. Sayeli Jayade is an employee of OPEN Health, which received consulting fees from Bristol Myers Squibb in connection with this study. Sanika Rege, Dipen Patel, and Namita Joshi were employees of OPEN Health at the time of this study. Vardhaman Patel, Samaneh Kalirai, and Lauren Seigel are employees of Bristol Myers Squibb and may be shareholders in the company. Daniel Wolin and Kimberly Boyle are employees of RTI Health Solutions, which received consulting fees from Bristol Myers Squibb in connection with this study.
Ethical Approval
The study protocol, survey, and relevant recruitment materials were evaluated by the RTI institutional review board and deemed exempt. This survey study was conducted in accordance with the ethical principles of the Declaration of Helsinki. Participants who were deemed eligible after answering the survey’s screening questions were required to provide electronic consent via a checkbox.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Armstrong, A.W., Jayade, S., Rege, S. et al. Evaluating Treatment Choice in Patients with Moderate to Severe Psoriasis in the United States: Results from a US Patient Survey. Dermatol Ther (Heidelb) 14, 421–439 (2024). https://doi.org/10.1007/s13555-023-01089-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-01089-6