Abstract
Background
The International Psoriasis Council (IPC) recommends an approach that considers body surface area (BSA), involvement in special areas, and treatment history for classifying patients as candidates for topical or systemic treatment. This study aimed to quantify the burden of psoriasis by describing BSA distribution, special area involvement, and treatments in a real-world population.
Methods
This retrospective cohort study included patients with psoriasis from the Optum® deidentified Electronic Health Records database with a BSA value (< 3%, 3–10%, and > 10%) recorded between 1 March 2014 and 1 September 2020. Treatments and special area involvement (face, scalp, palms/soles, nails, genitals) were identified within 90 days of the BSA value and stratified by BSA category.
Results
Among eligible patients (N = 5120), mean age was 51.4 years and 49.3% were women. The majority of patients (78.9%) were treated with any topical. Proportions of patients with BSA < 3%, 3–10%, and > 10% were 23.4%, 41.9%, and 34.6%, respectively; proportions with 0, 1, and 2+ special areas were 21.6%, 31.6%, and 45.7%, respectively; and 44.4%, 45.7%, and 45.9% of patients with BSA < 3%, 3–10%, and > 10%, respectively, had 2+ special areas.
Conclusion
The IPC classification can likely identify many more patients who may benefit from systemic therapy than BSA alone.
Graphical Abstract

Similar content being viewed by others
Why carry out this study? |
Although numerous treatments exist for psoriasis, nontreatment and undertreatment remain serious problems in the USA for those with special area involvement. |
Using real-world data, this study sought to quantify the burden of psoriasis in a real-world population by describing BSA distribution, special area involvement, and treatment options. |
What was learned from the study? |
Nearly half of the patients had two or more special areas affected at baseline; scalp and palms/soles were the most common special areas. |
The majority of patients with special areas were treated with topicals, while less than half of patients with more than two special areas were treated with more targeted therapies such as biologics or apremilast. |
These findings suggest that real-world treatment patterns do not yet reflect the current recommendations to identify patients who may benefit from systemic treatment and that an unmet need remains. |
Digital Features
This article is published with digital features, including a graphical abstract, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.24925254.
Introduction
Psoriasis is a chronic inflammatory disease of the skin that manifests as red, scaly plaques occurring most often on the elbows, knees, scalp, and lower back [1]. Multiple comorbidities are associated with this immune-mediated skin disease, which can lead to substantial reduction in quality of life [2]. Approximately 7.6 million adults, with an estimated prevalence of 3.0% in the USA, suffer from psoriasis [3, 4]. The economic burden of psoriasis is substantial, with an estimated annual cost of $112 billion in the USA [4].
The diagnosis of psoriasis is based largely on characteristic clinical features and rarely requires histological confirmation [5]. The severity categories for psoriasis have been essential tools for clinicians in making treatment decisions [6]. Psoriasis is categorized as mild, moderate, or severe on the basis of body surface area (BSA), Physician’s Global Assessment (PGA), and the Psoriasis Area and Severity Index (PASI) [6]. However, these measurements use different criteria to classify disease severity, and most do not account for the impact of special areas. Because of this, these measures may underestimate disease severity. When objectively assessing disease severity, physicians must also consider special areas such as the face, palms, soles, genitals, and scalp, as well as a patient’s treatment history and the impact of psoriasis on a patient’s quality of life [6].
Psoriasis in special areas significantly reduces quality of life. In the EMBRACE clinical study, with inclusion criteria requiring patients to have at least one special area involved and Dermatology Life Quality Index (DLQI) > 10, mean BSA at baseline was 7% (moderate disease severity) and yet DLQI was 18.3, signifying a very large impact on quality of life [7]. Approximately half of patients with psoriasis are estimated to have scalp psoriasis [8]. Patients with severe scalp involvement may present with mild body involvement, resulting in an underestimation of the severity of their disease. Mild psoriasis is treated with topical therapy, which is difficult to apply to the scalp with hair, resulting in low adherence rates [9]. Approximately 20% of patients with psoriasis have facial involvement, which significantly contributes to poor quality of life [10]. Genital skin involvement, which is estimated to affect up to 65% of patients [11], is often overlooked and thus commonly undiagnosed and untreated [12]. Palmoplantar psoriasis is often resistant to treatment and contributes to functional impairment in patients [13,14,15]. Because special areas represent a small portion of the overall BSA, patients with psoriasis in these difficult-to-treat areas may not be categorized as having disease that is severe enough to warrant systemic therapy.
Recently, the International Psoriasis Council (IPC) recommended an approach considering BSA, special area involvement, and treatment history to classify patients’ disease severity [6]. The panel noted that classification of disease severity should be patient centered, which can best be accomplished by considering these additional aspects of the disease alongside traditional objective measures. The IPC has indicated that patients with BSA > 10%, involvement in special areas, or failure of topical therapy are candidates for systemic therapy based on this approach [16].
Despite the availability of numerous treatments for psoriasis, nontreatment or undertreatment remains a serious problem in the USA [4]. Topical therapy is the standard of care for the treatment of mild-to-moderate psoriasis, whereas patients with moderate-to-severe disease require systemic therapy [17]. Although topical therapies are typically the first line of treatment for psoriasis, they are often inadequate in patients with psoriasis in special areas [7]. The objective of this study was to quantify the burden of psoriasis by describing BSA distribution, special area involvement, and treatments in a real-world population.
Methods
Study Design and Participants
This retrospective cohort study utilized the Optum® deidentified EHR dataset and included patients who had a BSA value recorded between 1 March 2014 and 1 September 2020. The index date was the first BSA value identified in the data (Fig. 1. The baseline period included the 365 days before the index date. Patients age ≥ 18 years on the index date, with at least one psoriasis diagnosis within 90 days before and after the index date, and with ≥ 365 days of continuous enrollment in the Optum® EHR dataset before and after the index date were included. The ‘initial treatment’ was defined as the treatment within 90 days prior to and after the index date and could include multiple treatments. Baseline characteristics were defined in the 365 days prior to the index date. If multiple values or measures were available for a characteristic, the measure prior to and most proximal to the index date was used. Optum® uses natural language processing (NLP) computing technology to extract critical facts from physician notes into usable datasets. The NLP data in this study provided detailed data on BSA values and special area involvement for patients with psoriasis.
Institutional Review Board approval to conduct this study was not necessary, as this study used deidentified patient records and did not involve the collection, use, or transmittal of individually identifiable data. The datasets generated during and/or analyzed during the current study are not publicly available as they were licensed by the authors’ institution to use for this study. This observational study based on secondary data from a healthcare claims and EHR database does not include any data collected from clinical trial participants (the purview of the Declaration of Helsinki).
Statistical Analysis and Outcomes
Summary statistics were calculated for patient characteristics using frequency and percentage for categorical or binary variables and mean and standard deviation for continuous variables. Initial treatments and special area involvement (face, scalp, palms/soles, nails, and genitals) were identified within 90 days of the BSA value and stratified by BSA categories. The distribution of BSA categories and number of special areas (0, 1, or 2+) were reported by initial treatment categories, including topicals only, conventional synthetic disease-modifying antirheumatic drugs (csDMARDs), biologics, and apremilast.
Results
A total of 5120 patients were eligible, with 23.4%, 41.9%, and 34.6% falling into BSA categories of < 3%, 3–10%, and > 10%, respectively (Table 1). The overall mean (SD) age was 51.4 (14.8) years, and age was similar across different levels of disease severity. The majority of included patients were white (83.2%) and almost half were female (49.3%). In addition, female patients were more likely to be in low BSA categories, while male patients generally had more severe conditions. More patients in the BSA < 3% category had commercial insurance as compared with patients with BSA 3–10% and patients with BSA > 10% (63.3% versus 60.1% and 56.0%, respectively) (Table 1). Although patients with BSA < 3% had lower mean (SD) body mass index (BMI) [30.4 (7.03) kg/m2] compared with patients with BSA 3–10% [31.7 (7.79) kg/m2] and patients with BSA > 10% [33.3 (8.72) kg/m2], all three groups were in the obesity range (BMI ≥ 30.0 kg/m2). The most common comorbidities at baseline were hypertension (21.9%) and hyperlipidemia (17.8%); it is worth noting that these occurred less frequently in patients with BSA < 3% compared with patients with BSA 3–10% and patients with BSA > 10% (Table 1). Furthermore, patients in the BSA < 3% category had a higher proportion of “never smokers” compared with the other two patient categories (47.0% versus 44.0% and 41.9%, respectively) (Table 1). At baseline, the majority of patients overall (78.9%) were treated with topicals, 31.1% were treated with biologics, and 17.8% were treated with csDMARDs. Among patients with BSA < 3%, 3–10% and > 10%, the proportions on topicals at baseline were 69.9%, 81.5%, and 81.8%, respectively; the proportions on biologics were 35.8%, 28.5%, and 31.2%, respectively; and the proportions on csDMARDs were 18.7%, 16.5%, and 18.7%, respectively.
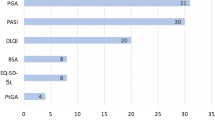
Psoriasis in special areas was prevalent in this real-world population (Fig. 2). At baseline, nearly half of patients (45.7%) had two or more special areas affected. Only 21.6% of patients had no special area involvement (Fig. 2A). Across BSA categories of < 3%, 3–10%, and > 10%, the proportions with 2+ special areas were similar at 44.4%, 45.9%, and 45.7%, respectively (Fig. 2B). The most frequently recorded special areas at baseline were scalp (43.3%) and palms/soles (37.4%) (Fig. 2C). The proportions of patients with special areas of the face (25.1%), genitals (24.9%), and nails (21.8%) were similar in this population.
Data were analyzed from 4470 patients on the basis of the initial treatment identified in the database (patients could have multiple initial treatments) (Table 2). The majority of patients were initially treated with biologics (n = 1764) or topicals only (n = 1733), followed by patients initially treated with csDMARDs (n = 680) or apremilast (n = 481). Mean (SD) age was lower [49.2 (14.07) years] in patients who had biologics as initial treatment compared with patients who had apremilast [52.0 (14.48) years], topicals [52.1 (15.27) years] or csDMARDs [53.1 (14.92) years] as initial treatment. Female patients were the majority in the apremilast and csDMARDs initial treatment groups (55.3% and 52.8%, respectively) and the minority in the topicals and biologics treatment groups (49.9% and 46.7%, respectively). In all initial treatment groups, patients were predominantly white (82.7%, 87.7%, 82.6%, and 78.7% for biologics, apremilast, topicals, and csDMARDs, respectively). The most prevalent other inflammatory disease (apart from psoriasis) in all initial treatment groups was psoriatic arthritis (20.4%, 18.4%, 17.0%, and 4.4% for biologics, csDMARDs, apremilast, and topicals, respectively).
Fewer patients with topicals as initial treatment (28.7%) had BSA > 10% compared with patients who had biologics (38.4%), csDMARDs (42.8%), or apremilast (43.9%) as initial treatments (Fig. 3A). A larger proportion (54.1%) of patients with csDMARDs as the initial treatment had 2+ special areas, compared with patients who had topicals (48.3%), biologics (43.8%), or apremilast (43.5%) (Fig. 3B).
Discussion
This retrospective cohort study of patients with psoriasis and a recorded BSA value aimed to quantify the burden of psoriasis by describing BSA distribution, special area involvement, and treatment in a real-world population. This study is one of the first to categorize the prevalence of special area involvement by BSA and by initial treatment and adds to the evidence regarding undertreatment of psoriasis. In addition, in this study BSA values were independent of special area involvement, suggesting that although specialized scores enable a more accurate assessment of disease severity in special areas, the dilemma remains whether to include these special area scores in scores such as PASI, PGA, BSA, and DLQI [18]. Overall, the proportion with involvement of 2+ special areas was approximately 45% across BSA categories. We also found that a large proportion (78.9%) of patients in the overall population (not considering special areas) were treated with topicals while less than 50% of patients with 2+ special areas were being treated with biologics (43.6%) or apremilast (43.5%); 62.6% were treated with csDMARDs in this patient population. Joint American Academy of Dermatology and National Psoriasis Foundation Guidelines recognize that topical treatment of intertriginous areas or hair-bearing skin, including special areas such as the groin and scalp, can be challenging [19] because the active ingredients may not reach the skin and there are safety concerns associated with the long-term use of topical treatments such as corticosteroids [19]. IPC recommends systemic therapy be considered for patients who have special areas or who have failed topical treatment. However, not all systemics have data in patients with low skin involvement in the presence of special areas, so treatment selection criteria ought to be carefully considered and informed by a data-driven approach. Psoriasis severity categories have been important for clinicians when treating patients; however, treatment history and special areas may be overlooked in severity classifications, leading to the undertreatment of those with more severe disease [6].
In this study, the prevalence of scalp psoriasis was slightly lower than that reported previously (43% versus 45–56%) [8]. Approximately 1 in 4 patients in this study had face psoriasis, which is slightly higher than the prevalence of 1 in 5 reported in earlier research [10]. Epidemiologic studies have reported a prevalence range of 20–40% for nail psoriasis and 20–30% for genital involvement [8, 11]. While on the lower end, the prevalence reported herein for nail psoriasis (22%) falls within this range, whereas the prevalence of genital psoriasis (25%) falls in the middle of the reported ranges. For palms and soles, this study found more than double the prevalence rate reported in other epidemiological studies (37% versus 12–16%) [8]. This may be because it included patients with BSA values that are typical of more severe disease. As treatment pathways for these special areas continue to evolve, ongoing monitoring of prevalence rates is important to assess the effectiveness of new recommendations and whether real-world practice aligns with current guidelines.
Presence of psoriasis in special areas can have a significant impact on patient quality of life and should be a reminder to assess the need for systemic treatment individually for each patient. As a patient’s quality of life cannot be completely determined with one measure, it is important to work with the patient to determine how satisfied they are with the treatment, which can require escalating the treatment on the basis of the patient's preference; depending on the patient’s comfort level, it may be necessary to work with them to determine the best treatment modality as well [19]. In addition, the importance of individualized treatment choices for patients with psoriasis is reinforced by the ample prevalence of cardiometabolic comorbidities overall, including hypertension (21.9%), hyperlipidemia (17.8%), and type 2 diabetes (9.8%) at baseline, and the suggestion of an increasing prevalence of these comorbidities with increasing BSA severity [20]. Several studies have documented the discordance between patient- and physician-reported severity [6]. Routine severity measures often underestimate the severity of psoriasis, resulting in undertreatment [6]. One observational, longitudinal cohort study found that the discordance between patient and physician assessments of severity was associated with a patient’s mental health status. This study found that individuals who screened positive for depression or anxiety were more than twice as likely to overestimate the severity of their psoriasis compared with their physician’s assessment (relative risk ratio: depression, 2.7; 95% CI 1.6–4.5; anxiety, 2.1; 95% CI 1.3–3.4) [21]. This may influence clinical decision-making inappropriately if not considered in the right context, highlighting the importance of a multidisciplinary approach to psoriasis care as well as screening for anxiety and depression concurrently, to ensure that treatments are tailored to address the disease activity as well as mental health comorbidity [21]. Analysis of data from a cross-sectional study of more than 100 patients with psoriasis found that a greater extent of disagreement between physician- and patient-reported severity was associated with significantly greater quality-of-life impairment (P = 0.001) [22, 23]. This discordance, and the subsequent impact on quality of life, highlights the need for personalized approaches to psoriasis treatment in real-world practice. For patients with psoriasis, new targeted treatments hold promise, but many factors, including efficacy, safety, and affordability, must be considered in selecting the optimal treatment for each patient [5].
This study is subject to some limitations. First, this retrospective cohort study includes patients with both incident and prevalent psoriasis and therefore is reflective of a cross-sectional nature of the disease and not of patients who are first diagnosed or initiating treatment for the first time. Also, information from the electronic health records capture only the portion of care that was provided at the visit and do not provide further information on the actual use of treatment. In this Optum® deidentified Electronic Health Record (EHR) dataset, we found that of 446,519 psoriasis patients, only 2.3% had a BSA value available in the data. This suggests that most patients with psoriasis do not have a recorded BSA value, so the representativeness of the population evaluated here with a recorded BSA value is unknown.
Strengths of this study include a relatively large psoriasis patient population with BSA values available and a pioneering approach, as this is one of the first studies to investigate and categorize the prevalence of special area involvement by BSA and by initial treatment. The findings are informative for clinical practice, as they may help healthcare providers accurately assess disease severity, enabling patients with psoriasis and special area involvement to receive systemic treatment. Lastly, this study may inform future research on psoriasis, including investigations into the reasons for undertreatment and possible strategies to mitigate it.
Conclusion
In real-world clinical practice, many patients with special area involvement have low skin involvement, and the proportion with multiple special areas may be independent of BSA category. In addition, many patients treated with topicals only have a high degree of special area involvement. These findings suggest that real-world treatment patterns do not yet reflect the IPC recommendations to identify patients who may benefit from systemic treatment. The high burden of special area involvement highlights the potential unmet need for systemic treatment in patients with psoriasis.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available due to restrictions, which were used under license for this study.
References
Parisi R, Iskandar IYK, Kontopantelis E, Augustin M, Griffiths CEM, Ashcroft DM. National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study. BMJ. 2020;369: m1590.
Armstrong AW, Mehta MD, Schupp CW, Gondo GC, Bell SJ, Griffiths CEM. Psoriasis prevalence in adults in the United States. JAMA Dermatol. 2021;157:940–6.
Rachakonda TD, Schupp CW, Armstrong AW. Psoriasis prevalence among adults in the United States. J Am Acad Dermatol. 2014;70:512–6.
Armstrong AW, Koning JW, Rowse S, Tan H, Mamolo C, Kaur M. Under-treatment of patients with moderate to severe psoriasis in the United States: analysis of medication usage with health plan data. Dermatol Ther (Heidelb). 2017;7:97–109.
Lebwohl M. Psoriasis. Lancet. 2003;361:1197–204.
Strober B, Ryan C, van de Kerkhof P, van der Walt J, Kimball AB, Barker J, et al. Recategorization of psoriasis severity: Delphi consensus from the International Psoriasis Council. J Am Acad Dermatol. 2020;82:117–22.
Mrowietz U, Barker J, Conrad C, Jullien D, Gisondi P, Flower A, et al. Efficacy and safety of apremilast in patients with limited skin involvement, plaque psoriasis in special areas, and impaired quality of life: results from the EMBRACE randomized trial. J Eur Acad Dermatol Venereol. 2023;37:348–55.
Merola JF, Li T, Li WQ, Cho E, Qureshi AA. Prevalence of psoriasis phenotypes among men and women in the USA. Clin Exp Dermatol. 2016;41:486–9.
Frez ML, Asawanonda P, Gunasekara C, Koh C, Loo S, Oon HH, et al. Recommendations for a patient-centered approach to the assessment and treatment of scalp psoriasis: a consensus statement from the Asia scalp psoriasis study group. J Dermatolog Treat. 2014;25:38–45.
Alpsoy E, Polat M, FettahlıoGlu-Karaman B, Karadag AS, Kartal-Durmazlar P, YalCın B, et al. Internalized stigma in psoriasis: a multicenter study. J Dermatol. 2017;44:885–91.
Meeuwis KAP, Potts Bleakman A, van de Kerkhof PCM, Dutronc Y, Henneges C, Kornberg LJ, et al. Prevalence of genital psoriasis in patients with psoriasis. J Dermatolog Treat. 2018;29:754–60.
Beck KM, Yang EJ, Sanchez IM, Liao W. Treatment of genital psoriasis: a systematic review. Dermatol Ther (Heidelb). 2018;8:509–25.
Merola JF, Qureshi A, Husni ME. Underdiagnosed and undertreated psoriasis: nuances of treating psoriasis affecting the scalp, face, intertriginous areas, genitals, hands, feet, and nails. Dermatol Ther. 2018;31:e12589.
Alajlan AM, Qadoumi TA. Palmoplantar psoriasis successfully treated with risankizumab. Cureus. 2021;13:e17434.
Al-Mutairi N, Abdalla TO, Nour TM. Resistant palmoplantar lesions in patients of psoriasis: evaluation of the causes and comparison of the frequency of delayed-type hypersensitivity in patients without palm and sole lesions. Med Princ Pract. 2014;23:561–7.
Blauvelt A, Gondo GC, Bell S, Echeverría C, Schmitt-Egenolf M, Skov L, et al. Psoriasis involving special areas is associated with worse quality of life, depression, and limitations in the ability to participate in social roles and activities. J Psoriasis Psoriatic Arthritis. 2023;8(3):100–6.
Takeshita J, Gelfand JM, Li P, Pinto L, Yu X, Rao P, et al. Psoriasis in the US Medicare population: prevalence, treatment, and factors associated with biologic use. J Invest Dermatol. 2015;135:2955–63.
Nicolescu AC, Ionescu MA, Constantin MM, Ancuta I, Ionescu S, Niculet E, et al. Psoriasis management challenges regarding difficult-to-treat areas: therapeutic decision and effectiveness. Life (Basel, Switzerland). 2022;12(12):2050.
Elmets CA, Korman NJ, Prater EF, Wong EB, Rupani RN, Kivelevitch D, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with topical therapy and alternative medicine modalities for psoriasis severity measures. J Am Acad Dermatol. 2021;84:432–70.
Gelfand JM, Yeung H. Metabolic syndrome in patients with psoriatic disease. J Rheumatol Suppl. 2012;89:24–8.
Carr E, Mahil SK, Brailean A, Dasandi T, Pink AE, Barker JN, et al. Association of patient mental health status with the level of agreement between patient and physician ratings of psoriasis severity. JAMA Dermatol. 2021;157:413–20.
Sommer R, Augustin M, Hilbring C, Ständer S, Hubo M, Hutt HJ, et al. Significance of chronic pruritus for intrapersonal burden and interpersonal experiences of stigmatization and sexuality in patients with psoriasis. J Eur Acad Dermatol Venereol. 2021;35:1553–61.
da Silva N, Augustin M, Hilbring C, von Stülpnagel CC, Sommer R. Patient-physician (dis)agreement on their reports of body surface area affected by psoriasis and its associations with disease burden. J Eur Acad Dermatol Venereol. 2022;36:e995–7.
Acknowledgements
Medical Writing and Editorial Assistance
Writing support was funded by Amgen Inc. and provided by Samantha Rivera, MS, of Peloton Advantage, LLC, an OPEN Health company.
Funding
This study was sponsored by Amgen Inc. The sponsor is funding the Rapid Service Fee.
Author information
Authors and Affiliations
Contributions
Mary E. Horner: Study concept, interpretation, writing. Kate K. Orroth: Conceptualization, design, investigation, supervision, methodology, writing. Junjie Ma: Study concept and design; data analysis. Yinkang Duan: Data analysis. Myriam Cordey: Conceptualization, design, investigation, supervision of research, writing.
Corresponding author
Ethics declarations
Conflict of Interest
Mary E. Horner: Consultant for Amgen Inc. Kate K. Orroth: Employee and stockholder of Amgen Inc. Junjie Ma: Employee and stockholder of Amgen Inc. Yinkang Duan: Consultant for Amgen Inc. Myriam Cordey: Employee and stockholder of Amgen Inc.
Ethical Approval
Institutional Review Board approval to conduct this study was not necessary, as this study used deidentified patient records and did not involve the collection, use, or transmittal of individually identifiable data. This observational study based on secondary data from a health care claims and EHR database does not include any data collected from clinical trial participants (the purview of the Declaration of Helsinki).
Additional information
Prior Presentation: Data from this study were included in an accepted abstract at the American Academy of Dermatology conference in 2023
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Horner, M.E., Orroth, K.K., Ma, J. et al. Redefining Disease Severity with Special Area Involvement and Reflecting on Treatment Patterns in a Real-World Psoriasis Population. Dermatol Ther (Heidelb) 14, 187–199 (2024). https://doi.org/10.1007/s13555-023-01065-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-01065-0