Abstract
Introduction
Microneedling is a cosmetic procedure that leverages the skin’s natural ability to heal in order to promote collagen formation and skin rejuvenation. To provide improved results, the technique can be combined with topical formulations. A new formulation of multiple actives, including omega-3 (n-3) polyunsaturated fatty acids (PUFAs), was designed to accelerate the resolution of inflammation and wound healing following micro-injury treatments, while enhancing the visible appearance of procedure results, including erythema, luminosity and skin texture.
Methods
In this randomised, controlled, split-face study, we examined 32 healthy female participants aged 30–70 years for 4 weeks following microneedling treatment with a novel multiple-active-ingredient formulation or conventional microneedling protocol with a hyaluronic acid control serum. Changes in skin condition were assessed by blinded clinical photography and expert evaluation. Measurements were collected at baseline, 1 h, 1 day, 7 days and 28 days post treatment.
Results
Significantly greater improvements in expert-assessed erythema, luminosity and skin texture were reported following application of the novel multiple-active-ingredient formulation than the hyaluronic acid control serum. This was confirmed by representative VISIA®-CR imaging.
Conclusion
These data provide new evidence for the role of a novel multiple-active-ingredient formulation for improving skin outcomes up to 28 days following microneedling in adults with healthy skin when compared with a hyaluronic acid serum. The n-3 PUFA content of this formulation may drive accelerated inflammation resolution and wound healing alongside the complementary action of the other active ingredients, leading to the observed improvements in erythema, luminosity and skin texture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Micro-injury treatments, such as microneedling, leverage the skin’s natural healing abilities to promote skin rejuvenation; however, they are commonly associated with acute complications including erythema and oedema, and multiple sittings are often required to achieve the desired effect. |
Microneedling techniques are commonly combined with the application of topical formulations that enhance skin rejuvenation and reduce healing time. |
What was the aim of the study? |
The objective of this split-face study was to determine whether topical application of a novel multiple-active formulation before, during and up to 7 days after microneedling can resolve inflammation and accelerate wound healing in adults with healthy skin to amplify luminosity and reduce erythema and tactile skin texture over 28 days compared with conventional microneedling protocol with a hyaluronic acid serum. |
What were the study outcomes/conclusions? |
Significantly greater improvements in expert-assessed erythema, luminosity and skin texture were reported following application of the novel multiple-active-ingredient formulation than the hyaluronic acid control serum. |
What has been learned from the study? |
These data support the topical application of a novel multiple-active-ingredient formulation in combination with microneedling for accelerating inflammation resolution and subsequent wound healing in female adults with healthy skin; however, further evaluation among adult male subjects with healthy skin is needed to ensure broader efficacy and applicability. |
The novel formulation shows promising results for reducing the downtime associated with micro-injury treatments while amplifying the associated benefits of skin luminosity and texture. |
The presence of omega-3 polyunsaturated fatty acids in the novel formulation may have played a key role in improving inflammation resolution alongside the complementary action of the other active ingredients, leading to the observed improvements in skin outcomes. |
Introduction
The skin is the largest organ of the human body, acting as a protective barrier between the body’s internal and the external environment [1]. As such, the skin is integral to maintaining physiological homeostasis of the human body [2]. Skin wound healing, an innate immune response to tissue injury, is critical for facilitating rapid wound closure and prompting restoration of skin barrier function to prevent further damage or infection [3]. The wound-healing process is complex and requires effective and precisely coordinated interplay and communication between a multitude of cell types across four generally accepted phases: haemostasis, inflammation, proliferation and remodelling [2,3,4].
Upon skin injury, haemostasis is initiated by thrombocytes, and degranulation of platelets activates the complement cascade to stimulate inflammatory cells to the site of injury [3, 4]. The inflammatory phase is characterised by the migration of leucocytes, especially neutrophils, monocytes and lymphocytes, to the site of injury [3, 4]. The differentiation of monocytes into macrophages is important for the inflammatory–proliferative phase transition during wound healing. M1 macrophages are associated with phagocytic activity before transforming into the M2 subset, which has a reparative phenotype [2]. The transition of M1 to M2 macrophages is the rate-limiting step in wound healing; if it does not occur, chronic wounds develop that are slow to close [2, 3]. Resolution of inflammation is one of the four well-established outcomes of acute inflammation, along with progression to chronic inflammation, abscess development and scar formation [5]. Similarly to the onset of inflammation, resolution is an active process with an established set of chemical mediators, including omega-3 (n-3) polyunsaturated fatty acids (PUFAs) [5]. PUFAs are integral constituents of the phospholipids that make up all cell membranes [6]; eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), the predominant marine-derived n-3 PUFAs [7], give rise to specialised pro-resolving mediators (SPMs), including resolvins, which are anti-inflammatory and help to resolve inflammation [6, 8]. SPMs regulate inflammation resolution by limiting further neutrophil tissue infiltration, stimulating clearance of leucocytes, and returning host cells to a non-inflammatory state [9]. Increased EPA and DHA and decreased pro-inflammatory arachidonic acid within cell membranes result in an altered expression pattern of anti-inflammatory eicosanoids and resolvins. Therefore, the fatty acid composition of inflammatory cells influences their function [6].
As inflammation subsides, the wound-healing process moves into the proliferative phase, which can take up to 3 weeks post injury [3, 4]. This is characterised by re-epithelialisation, angiogenesis and the formation of granulation tissue to aid wound closure [3]. The remodelling phase follows granulation tissue development; the wound contracts and collagen remodelling occurs, allowing the wound to gradually become stronger with time [4]. Dysregulation of any of the four phases or excessive host responses to the injury results in prolonged wound healing and may lead to scaring [3].
Some cosmetic procedures, particularly micro-injury treatments, leverage the skin’s natural ability to heal for the desired effect [10]. Microneedling is a minimally invasive procedure involving superficial puncturing of the skin at a controlled depth to cause an intrinsic wound-healing cascade that promotes collagen formation and skin rejuvenation [11, 12]. Consequently, microneedling has demonstrated efficacy in improving the appearance of scars resulting from acne [13, 14] and striae alba [15], as well as in the treatment of post-surgical scars during active wound healing [16]. The procedure is frequently used in combination with a topical formulation, such as topical growth factors, platelet-rich plasma, bioactive cytokines, skin-lightening agents or chemical peels to enhance skin rejuvenation and reduce healing time [11, 12]. However, this is often compared with microneedling or topical formulation application alone in patients with dermatological conditions, such as acne scarring and pigmentation [12, 17,18,19], or for the purpose of improving signs of ageing and photoageing [11, 20, 21]. Although microneedling is well tolerated by patients, erythema and oedema can last for days and multiple sittings are often required to achieve the desired effect [12].
To aid the wound-healing process, a novel multiple-active-ingredient formulation has been designed to work synergistically with micro-injury treatments. The formulation contains a complex of active ingredients including n-3 PUFAs, which have previously been studied to establish their role in dermatological inflammation resolution [7]. Considering the anti-inflammatory properties demonstrated by increased n-3 PUFA delivery to cell membranes [6, 8], we hypothesise that its topical application will drive inflammation resolution along with the complementary action of the other active ingredients (beta-glucans, Bacillus ferment, Albatrellus confluens and niacinamide). To the best of our knowledge, no prior studies have assessed the effects of these nutrients in a single formulation following micro-injury skin care treatments. In the present study, we aim to determine whether topical application of the novel multiple-active formulation before, during and up to 7 days after microneedling can resolve inflammation and accelerate wound healing to amplify luminosity and reduce erythema and tactile skin texture over 28 days compared with conventional microneedling protocol with a hyaluronic acid serum.
Methods
Study Design
This single-centre, randomised, controlled, split-face study was conducted between September and October 2021 at Validated Claim Support, LLC, Teaneck, NJ, USA. The study adhered to the principles of Good Clinical Practice and the Declaration of Helsinki and its subsequent amendments. Regarding coronavirus disease 2019, all internal safety procedures adhered to federal and local requirements and regulations to reduce the risk of virus transmission. Ethical approval was granted by the Western Institutional Review Board (IRB; IRB approval number 1262764).
Study Population
Thirty-three healthy females aged between 30 and 70 years with fine lines and/or wrinkles (score of > 3 on a 10-point ordinal scale; “0 = none” to “9 = numerous, deep wrinkles”) provided informed consent to participate in the study.
Procedure
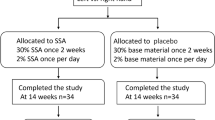
The study was conducted for 4 weeks, with five visits in total. Figure 1 provides a schematic of the study procedure timeline.
Following a washout period of at least 5 days, participants arrived at the test site with clean facial skin and applied no other face products. After approximately 8 min of double-cleansing the face with a gentle skin cleanser and cleansing gel, participants acclimated to the clinic environment for 15 min prior to baseline assessments. All microneedling procedures were conducted by a licensed aesthetician at the clinic. The application of the novel multiple-active-ingredient formulation and the hyaluronic acid (control serum) was randomised. The split-face method was used for product application; the novel formulation was applied to side A and left to penetrate the skin for 2 min. No product was applied to side B. A dermaroller of 1–1.5 mm-sized needles was rolled over the face in two passes using a snake pattern. During the procedure, the multiple-active formulation and the hyaluronic acid serum were used on sides A and B, respectively. Both serums were reapplied to their respective treatment areas after microneedling treatment. The evening after treatment, participants were instructed to apply the novel multiple-active-ingredient formulation to side A and nothing to side B, as per conventional microneedling procedures [12]. For the 7 days post treatment, participants were to use the novel multiple-active-ingredient formulation before sunscreen (sun protection factor 30) and oil-free moisturiser in the morning and before moisturiser in the evening. On the control side, participants were instructed to only use sunscreen and moisturiser in the morning and only moisturiser in the evening. After 7 days, participants were instructed to use sunscreen and moisturiser in the morning and moisturiser only in the evening, on both sides of the face.
Outcomes
Changes in skin condition and clinical photography were assessed with blinded evaluation by a trained objective grader at baseline, and at immediate (1 h and 1 day) and long-term (7 days and 28 days) time points post treatment. Erythema, luminosity and skin texture were graded using a 5-point (erythema: “0 = none” to “4 = red/discoloured appearance”) or 10-point ordinal scale of visual appearance (luminosity: “0 = radiant/luminous/glowing appearance” to “9 = dull/matte/sallow appearance”; skin texture: “0 = smooth, soft surface feel” to “9 = rough, coarse surface feel”).
Clinical photographs of the face were captured at three angles (left, centre and right) using Canfield VISIA®-CR facial imaging system (Fairfield, New Jersey) with standard and cross-polarised light to neutralise any skin shine. Clinical photography was performed by a clinical photographer in a controlled setting. VISIA®-CR imaging was used to provide visual representative examples of differences between treatment groups.
Safety was monitored throughout the study for adverse events (AEs).
Statistical Analysis
Statistical analyses were performed with the IBM SPSS software (IBM Corp, Armonk, NY, USA). Analyses were based on all participants who were randomised to treatment and completed the study (per protocol). Expert-graded skin assessment data were analysed within treatment by Wilcoxon’s signed rank test and between treatment by analysis of covariance with pre-treatment baseline data as a covariate. All statistical analyses employed a significance level of p < 0.05.
Results
Of the 33 participants enrolled in the study, 32 were included in the per-protocol analyses. One participant was excluded from analyses because of incorrect application of the control serum and novel formulation during the microneedling procedure. Demographic details of the per-protocol population are given in Table 1.
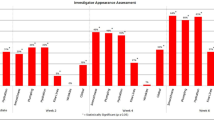
Representative visual examples of differences in erythema, luminosity and skin texture between treatment groups can be found in Fig. 2.
Representative standard light clinical photographs of differences in skin outcomes at baseline (top) versus following microneedling treatment (bottom) with a novel multiple-active-ingredient formulation (left) or conventional microneedling protocol with a hyaluronic acid control serum (right). (i) An increase in erythema is noted at 1 h from baseline across the forehead and cheek with the control serum. (ii) Improvements in luminosity are noted at 1 h with the novel multiple-active-ingredient formulation across the browbone and cheek. (iii) Improvements in skin texture are noted at 28 days with the novel multiple-active formulation across the forehead
Erythema
One hour post treatment with hyaluronic acid serum, a significant increase in erythema was observed (30.0%; p = 0.0082). This was greater than that observed for the novel formulation (17.1%); however, the difference between groups was not significant (p = 0.2926) (Fig. 2i). A significant difference was observed between treatments at day 7 in favour of the novel formulation reducing erythema (−31.7% vs −20.0%; p = 0.0459) (Fig. 3). Decreased erythema was maintained at day 28 for both treatments.
Skin Luminosity
A significant improvement in skin luminosity was observed at all time points for both treatments. A significant difference was observed between treatments in favour of the novel multiple-active-ingredient formulation at 1 h (37.8% vs 15.0%; p = 0.0002) (Fig. 2ii), day 1 (35.4% vs 18.1%; p < 0.0001) and day 7 (30.7% vs 22.8%; p = 0.0159) (Fig. 4).
Skin Texture
A significant improvement from baseline in tactile skin texture was observed at all time points for both treatments. A significant difference was observed between treatments at 1 h (−31.7% vs −7.6%; p = 0.0001), day 1 (−31.0% vs −22.2%; p = 0.0357) and day 28 (−32.4% vs −25.7%; p = 0.0025) (Fig. 2iii) in favour of the novel multiple-active-ingredient formulation (Fig. 5).
Three AEs were reported by three participants, respectively, during the study. Of these, right ankle sprain and mid-back pain with a fall were deemed unrelated to the investigational product. One AE, pimples, was possibly associated with the investigational product.
Discussion
In the present report, we describe evidence for the efficacy of topical application of a novel multiple-active-ingredient formulation in combination with microneedling for accelerating inflammation resolution and subsequent wound healing, which led to the improvement of several skin parameters over 28 days. The current study demonstrates that the topical application of the novel formulation before, during and up to 7 days after microneedling improves expert-graded assessments of erythema, luminosity and skin texture compared with conventional microneedling protocol plus hyaluronic acid serum. The novel formulation shows promising results for reducing the downtime associated with micro-injury treatments while amplifying the associated benefits.
Erythema is a common, expected complication of microneedling, which varies in severity and duration [22]. Given the likelihood of erythema, a significant reduction through the application of topical formulations, as observed with the novel multiple-active-ingredient formulation, is encouraging for improving the recovery time associated with microneedling procedures. The therapeutic administration of n-3 PUFAs is postulated to modulate or regulate local inflammatory processes and stimulate early angiogenesis at wound areas to accelerate the healing rate [7]. For example, EPA and DHA can inhibit several aspects of inflammation and give rise to SPMs, including resolvins and protectins, involved in the resolution of inflammation [23]. As erythema is a consequence of inflammation [24], the reduction in erythema observed in this study may represent accelerated inflammation resolution and improved skin recovery facilitated by the n-3 PUFA content of the multiple-active formulation. A reduction in erythema associated with cutaneous photoageing has been shown following both oral and topical n-3 PUFA application [7]. Additionally, topical application of n-3 PUFAs to human skin to support the sunburn response (an inflammatory reaction clinically characterised by erythema and oedema) led to a reduction in erythema compared with controls [25, 26]. The present study extends these findings to the topical application of n-3 PUFAs for reducing erythema following microneedling of healthy human skin.
The inflammation-resolving role of n-3 PUFAs may also be supported by the fungal-derived extract, Albatrellus confluens, which is a source of the bioactive phenolic compounds grifolin and neogrifolin [27]. These compounds demonstrate antagonistic activity to the heat-sensitive transient receptor vanilloid 1 (TRPV1) in vitro and in vivo [27]; blocking TRPV1 has anti-inflammatory properties, which may improve wound healing to reduce inflammation-associated tissue damage [28]. Consequently, blocking TRPV1 is an established approach for the treatment of sensitive skin [27, 29, 30]. A grifolin-containing formulation has demonstrated efficacy for reducing stinging and burning sensations, reddening and microcirculation upon irritation or thermal stress in adults with sensitive skin [27]. The present study extends these findings to adults without sensitive skin following microneedling. Therefore, inhibiting TRPV1, together with the topical application of n-3 PUFAs, may also be a promising avenue for the treatment of micro-injury-induced inflammatory responses.
Significant improvements in skin luminosity and texture were also observed at immediate and long-term time points following microneedling with the novel multiple-active-ingredient formulation. This may be due to the niacinamide content of the formulation, as niacinamide has been used in the cosmetic field for decades to effectively improve a broad array of skin appearance concerns including brightening of skin tone and texture [31]. However, the positive outcomes observed in this study may also be indicative of accelerated inflammation resolution to allow for faster wound healing and thus a shorter time from microneedling treatment to visible improvements in skin condition. n-3-PUFA-derived resolvins inhibit neutrophil migration and enhance macrophage phagocytosis, which promote inflammation resolution and initiate the proliferative phase of wound healing [32]. Similarly, in vivo studies and clinical trials have shown evidence for beta-glucans as potent inducers of macrophage, keratinocyte and fibroblast activation, migration and proliferation; this allows for accelerated wound closure and therefore a reduced healing time and total cost per treatment [33]. However, the efficacy of the healing process may be affected by the microbial composition of wounds, as a loss of microbial diversity often results in prolonged inflammation and thus delayed healing [34]. Consequently, the advantages of probiotic bacteria for promoting wound healing have been proposed extensively via induction of the immune response, angiogenesis and decreased inflammation [35, 36]. This is reflected by the efficacy of topical probiotics in healthy subjects, with reductions in erythema, oedema and skin sensitivity observed [36]. The visible improvement in skin luminosity and texture in addition to erythema following microneedling may therefore be attributable to the n-3 PUFA content of the novel formulation and the complementary actions of beta-glucans and the Bacillus ferment probiotic, by resolving inflammation faster, restoring skin barrier strength and the skin’s microbiome to improve the skin recovery process. The niacinamide content of the novel formulation may work together with the other active ingredients to amplify the end results.
There are certain limitations to this study. The participants were only followed up for 4 weeks post microneedling treatment, which was relatively short. While these data are promising, it is important to consider that multiple microneedling sittings are required to achieve the desired effect; when using a 1.5-mm dermaroller, there should be at least a 3-week gap between sittings and it takes approximately 3–6 months after treatment to see final results, to allow for collagen deposition [12]. Twice-daily topical application of hyaluronic acid for 28 days post microneedling has been shown to enhance the clinical appearance of the skin among adults with dry facial skin [37]. As the novel multiple-active formulation was applied twice daily for only 7 days after one microneedling sitting in this study, it may be beneficial to explore the continued use of the formulation between monthly sittings. Additionally, as these data confirm the utility of the novel formulation in adults with healthy skin, it may be valuable to explore the effect of the formulation on skin types and conditions for which microneedling has previously demonstrated efficacy, including those with post acne erythema and rosacea [12, 38, 39]. Lastly, as women account for the vast majority of Dermalogica customers, only female participants were included in the study; therefore, results may not be applicable to male skin. There are significant differences in certain biophysical properties of the skin between men and women, such as levels of hydration, sebum production, pigmentation, and skin thickness [40], and while the exploration of these gender-specific factors was not in the remit of this study, they may be an objective in future studies.
Conclusion
Overall, these data provide evidence for the role of a novel multiple-active-ingredient formulation in accelerating inflammation resolution and wound healing following microneedling in adults with healthy skin. While microneedling plus hyaluronic acid serum improved expert-graded assessment of several skin parameters, the addition of the n-3-PUFA-rich formulation led to significantly greater improvements in erythema, luminosity and texture. Considering the anti-inflammatory properties demonstrated by increased delivery of n-3 PUFAs and SPMs to cell membranes [6, 8], their presence in the novel formulation may have played a key role in improving inflammation resolution alongside the complementary action of the other active ingredients, leading to the observed improvements in skin outcomes. Given the positive results of using the novel formulation for microneedling, it would be beneficial to explore the effect of the multiple-active-ingredient formulation following alternative micro-injury treatments such as laser therapy and plasma fibroblast skin tightening to determine the extent to which the formulation could be used within the evolving field of cosmetics and dermatology.
Data Availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Danso MO, Berkers T, Mieremet A, Hausil F, Bouwstra JA. An ex vivo human skin model for studying skin barrier repair. Exp Dermatol. 2015;24(1):48–54.
Sorg H, Tilkorn DJ, Hager S, Hauser J, Mirastschijski U. Skin wound healing: an update on the current knowledge and concepts. Eur Surg Res. 2017;58(1–2):81–94.
Landén NX, Li D, Ståhle M. Transition from inflammation to proliferation: a critical step during wound healing. Cell Mol Life Sci. 2016;73(20):3861–85.
Thiruvoth FM, Mohapatra DP, Kumar D, Chittoria SRK, Nandhagopal V. Current concepts in the physiology of adult wound healing. Plast Aesthet Res. 2015;2:250–6.
Kohli P, Levy BD. Resolvins and protectins: mediating solutions to inflammation. Br J Pharmacol. 2009;158(4):960–71.
Calder PC. Omega-3 fatty acids and inflammatory processes. Nutrients. 2010;2(3):355–74.
Huang TH, Wang PW, Yang SC, Chou WL, Fang JY. Cosmetic and therapeutic applications of fish oil’s fatty acids on the skin. Mar Drugs. 2018;16(8):256.
Calder PC. Eicosapentaenoic and docosahexaenoic acid derived specialised pro-resolving mediators: concentrations in humans and the effects of age, sex, disease and increased omega-3 fatty acid intake. Biochimie. 2020;178:105–23.
Panigrahy D, Gilligan MM, Serhan CN, Kashfi K. Resolution of inflammation: an organizing principle in biology and medicine. Pharmacol Ther. 2021;227:107879.
Jourdan M, Madfes DC, Lima E, Tian Y, Seité S. Skin care management for medical and aesthetic procedures to prevent scarring. Clin Cosmet Investig Dermatol. 2019;12:799–804.
Merati M, Woods C, Reznik N, Parker L. An assessment of microneedling with topical growth factors for facial skin rejuvenation: a randomized controlled trial. J Clin Aesthet Dermatol. 2020;13(11):22–7.
Singh A, Yadav S. Microneedling: advances and widening horizons. Indian Dermatol Online J. 2016;7(4):244–54.
Shen Y-C, Chiu W-K, Kang Y-N, Chen C. Microneedling monotherapy for acne scar: systematic review and meta-analysis of randomized controlled trials. Aesthetic Plast Surg. 2022;46(4):1913–22.
Casabona G, Alfertshofer MG, Kaye KO, et al. Safety and efficacy of microneedling technology in the treatment of acne scars. J Cosmet Dermatol. 2021;20(11):3482–91.
Siadat A, Moeine R, Iraji F, Faghihi G, Hosseini SM. Evaluating the efficacy of microneedling technique in treating striae alba lesions. Arch Dermatol Res. 2023;315(7):2075–8.
Claytor RB, Sheck CG, Chopra V. Microneedling outcomes in early postsurgical scars. Plast Reconstr Surg. 2022;150(3):557e–561e.
Iriarte C, Awosika O, Rengifo-Pardo M, Ehrlich A. Review of applications of microneedling in dermatology. Clin Cosmet Investig Dermatol. 2017;10:289–98.
Mohamed M, Beshay YMA, Assaf HM. Microneedling with glutathione versus microneedling alone in treatment of facial melasma: split-face comparative study. J Cosmet Dermatol. 2023. https://doi.org/10.1111/jocd.15834.
Nandini AS, Sankey SM, Sowmya CS, Sharath Kumar BC. Split-face comparative study of efficacy of platelet-rich plasma combined with microneedling versus microneedling alone in treatment of post-acne scars. J Cutan Aesthet Surg. 2021;14(1):26–31.
Park GH, Kwon HH, Seok J, et al. Efficacy of combined treatment with human adipose tissue stem cell-derived exosome-containing solution and microneedling for facial skin aging: a 12-week prospective, randomized, split-face study. J Cosmet Dermatol. 2023. https://doi.org/10.1111/jocd.15872.
Liang X, Li J, Yan Y, et al. Efficacy of microneedling combined with local application of human umbilical cord-derived mesenchymal stem cells conditioned media in skin brightness and rejuvenation: a randomized controlled split-face study. Front Med (Lausanne). 2022;9: 837332.
Gowda A, Healey B, Ezaldein H, Merati M. A systematic review examining the potential adverse effects of microneedling. J Clin Aesthet Dermatol. 2021;14(1):45–54.
Calder PC. Omega-3 polyunsaturated fatty acids and inflammatory processes: nutrition or pharmacology? Br J Clin Pharmacol. 2013;75(3):645–62.
Sudo M, Fujimoto K. Traveling wave of inflammatory response to regulate the expansion or shrinkage of skin erythema. PLoS ONE. 2022;17(2): e0263049.
Pilkington SM, Watson REB, Nicolaou A, Rhodes LE. Omega-3 polyunsaturated fatty acids: photoprotective macronutrients. Exp Dermatol. 2011;20(7):537–43.
Puglia C, Tropea S, Rizza L, Santagati NA, Bonina F. In vitro percutaneous absorption studies and in vivo evaluation of anti-inflammatory activity of essential fatty acids (EFA) from fish oil extracts. Int J Pharm. 2005;299(1):41–8.
Hettwer S, Bänziger S, Suter B, Obermayer B. Grifolin derivatives from Albatrellus ovinus as TRPV1 receptor blockers for cosmetic applications. Int J Cosmet Sci. 2017;39(4):379–85.
Bagood MD, Isseroff RR. TRPV1: role in skin and skin diseases and potential target for improving wound healing. Int J Mol Sci. 2021;22(11):6135.
Srour J, Bengel J, Linden T, et al. Efficacy of a skin care cream with TRPV1 inhibitor 4-t-butylcyclohexanol in the topical therapy of perioral dermatitis. J Cosmet Dermatol. 2020;19(6):1409–14.
Kueper T, Krohn M, Haustedt LO, Hatt H, Schmaus G, Vielhaber G. Inhibition of TRPV1 for the treatment of sensitive skin. Exp Dermatol. 2010;19(11):980–6.
Boo YC. Mechanistic basis and clinical evidence for the applications of nicotinamide (niacinamide) to control skin aging and pigmentation. Antioxidants (Basel). 2021;10(8):1315.
Menon R, Krzyszczyk P, Berthiaume F. Pro-resolution potency of resolvins D1, D2 and E1 on neutrophil migration and in dermal wound healing. Nano LIFE. 2017;7(1):1750002.
Majtan J, Jesenak M. β-glucans: multi-functional modulator of wound healing. Molecules. 2018;23(4):806.
Johnson TR, Gómez BI, McIntyre MK, et al. The cutaneous microbiome and wounds: new molecular targets to promote wound healing. Int J Mol Sci. 2018;19(9):2699.
Golkar N, Ashoori Y, Heidari R, et al. A novel effective formulation of bioactive compounds for wound healing: preparation, in vivo characterization, and comparison of various postbiotics cold creams in a rat model. Evid Based Complement Alternat Med. 2021;2021:8577116.
Knackstedt R, Knackstedt T, Gatherwright J. The role of topical probiotics on wound healing: a review of animal and human studies. Int Wound J. 2020;17(6):1687–94.
Bravo B, Correia P, Gonçalves Junior JE, Sant’Anna B, Kerob D. Benefits of topical hyaluronic acid for skin quality and signs of skin aging: from literature review to clinical evidence. Dermatol Ther. 2022;35(12):e15903.
Berardesca E, Bonfigli A, Cribier B, et al. A split-face study assessing the clinical benefit, tolerability and subject satisfaction of a dermocosmetic in subjects with rosacea associated with erythema and sensitive skin. Clin Cosmet Investig Dermatol. 2020;13:751–8.
Cohen BE, Elbuluk N. Microneedling in skin of color: a review of uses and efficacy. J Am Acad Dermatol. 2016;74(2):348–55.
Rahrovan S, Fanian F, Mehryan P, Humbert P, Firooz A. Male versus female skin: what dermatologists and cosmeticians should know. Int J Womens Dermatol. 2018;4(3):122–30.
Acknowledgements
We thank the participants of the study. We also thank Validated for the collection and analysis of study data.
Medical Writing and Editorial Assistance.
Medical writing support was provided by Hannah Avery, PhD, of Meditech Media, a medical communications agency. Support for this assistance was funded by Dermalogica, LLC.
Funding
Sponsorship for this study and Rapid Service Fee were funded by Dermalogica, LLC.
Author information
Authors and Affiliations
Contributions
All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for all aspects of the work, and have given their approval for this version to be published. Russell Wong, Angela Murphy, Monica Lira, Mariangela G. de O. Sichmann, Alexis R. Kim, Veronica D. Saechee, Kevin D. Hermanson and Stacy S. Hawkins contributed to the conception and design of the study, as well as the drafting and critical revision of the manuscript. In addition, Russel Wong, Mariangela G. de O. Sichmann, Alexis R. Kim and Veronica D. Saechee also contributed to the acquisition, analysis and interpretation of data; Angela Murphy contributed to the analysis and interpretation of data; and Kevin D. Hermanson and Stacy S. Hawkins contributed to the interpretation of data.
Corresponding author
Ethics declarations
Conflict of Interest
Russell Wong has received honoraria from Dermalogica, LLC. Angela Murphy, Monica Lira, Mariangela G. de O. Sichmann, Alexis R. Kim and Veronica D. Saechee are employees of Dermalogica, LLC. Kevin D. Hermanson and Stacy S. Hawkins are employees of Unilever Research and Development.
Ethical Approval
Ethical approval was granted by the Western Institutional Review Board (IRB; IRB approval number 1262764). The study adhered to the principles of Good Clinical Practice and the Declaration of Helsinki and its subsequent amendments. Written informed consent was obtained for the publication and use of all participants’ images prior to their enrolment in the study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wong, R., Murphy, A., Lira, M. et al. Microneedling with a Novel, n-3-PUFA-Rich Formulation Accelerates Inflammation Resolution to Improve Skin Recovery Outcomes in Adults with Healthy Skin. Dermatol Ther (Heidelb) 13, 3057–3069 (2023). https://doi.org/10.1007/s13555-023-01049-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-01049-0