Abstract
Introduction
Hidradenitis suppurativa (HS) has been linked to higher cardiovascular risk (CVR) due to its inflammatory burden. There is little evidence on how biologic treatment could modify the cardiovascular risk of patients with HS. The aims of the present study were to explore the modification of CVR in patients under adalimumab treatment and to explore the potential factors associated with CVR improvement.
Methods
A prospective longitudinal study was performed. A cohort of patients with HS treated with adalimumab was followed up. Carotid intima–media thickness (IMT) and other clinical and biochemical CVR factors were collected at baseline and 32 weeks after starting the treatment.
Results
Twenty-seven patients with severe HS were included. Overall, there were no differences in IMT between baseline (633 μm) and 32 weeks follow-up (634 μm). However, 40.7% (11/27) of the patients presented an improvement in IMT. This group (IMT responders) had a higher prevalence of dyslipidemia, diabetes mellitus, higher HbA1c levels, consumed more tobacco, and had higher BMI at baseline. Moreover, these patients had lower IHS4 scores at baseline and tended to have a greater IMT basal value, indicating a higher burden of subclinical atherosclerosis.
Conclusions
Adalimumab treatment might benefit a subset of patients with HS in terms of cardiovascular risk reduction. In light of the results of the present study patients with classical cardiovascular risk factors, and those with higher burden of subclinical atherosclerosis and with less inflammatory load, may be more likely to improve their IMT during adalimumab treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Hidradenitis suppurativa has been associated with higher cardiovascular risk. No studies have evaluated cardiovascular risk reduction in patients with hidradenitis suppurativa under active treatment. |
The study aimed to evaluate if TNF blockade could lead to an improved cardiovascular risk in patients with severe hidradenitis suppurativa. |
What was learned from the study? |
Adalimumab treatment might benefit a subset of patients in terms of cardiovascular risk reduction, specifically patients with classical cardiovascular risk factors, subclinical atherosclerosis, and less inflammatory load. |
TNF blockade could be of interest to improve cardiovascular risk in selected patients with hidradenitis suppurativa. |
Introduction
Hidradenitis suppurativa (HS) is a chronic follicular disorder characterized by the development of painful nodules, abscesses, and fistulae in apocrine gland areas. Its treatment is still challenging, and is mainly based on topical and oral antibiotics, oral retinoids, biologic drugs, and surgery. Moreover, this entity has been previously associated with higher cardiovascular risk because of the great associated inflammatory burden [1, 2] or endothelial dysfunction [3], as demonstrated for other skin diseases such as psoriasis [4]. One accessible technique for cardiovascular risk stratification in patients with HS and other diseases is the carotid intima–media thickness (IMT), which reflects the burden of subclinical atherosclerosis and is therefore linked to higher risk of cardiovascular events [5,6,7,8].
Adalimumab is one of the standard treatments for patients with severe HS [9]. It acts through the inhibition of tumor necrosis factor (TNF) and therefore leads to a decrease in the inflammatory lesions in patients [1]. As a result of its anti-inflammatory effect, it has been hypothesized that adalimumab might be of benefit to patients with inflammatory diseases and higher cardiovascular risk [4]. Despite this hypothesis, no studies have addressed the issue of cardiovascular risk improvement in patients with severe HS who receive adalimumab treatment.
Given that cardiovascular disorders are currently the leading cause of mortality [10], deeper knowledge about the possible implication of adalimumab treatment in cardiovascular risk improvement in patients with HS is of great interest. Moreover, further characterization of the subsets of patients who might benefit from this therapy could lead to a more holistic approach to the disease treatment. Therefore, the aim of this study are to (a) explore the evolution of cardiovascular risk by means of carotid IMT in a cohort of patients with HS under adalimumab treatment; and (b) explore potential clinical and biochemical factors associated with cardiovascular risk improvement in these patients.
Methods
Design
A prospective longitudinal study was performed. A cohort of patients with HS treated with adalimumab was followed up to explore if TNF blockade could improve the cardiovascular risk of patients with HS, and to evaluate potential clinical and blood biomarkers associated with cardiovascular risk improvement in this population.
Patients
Patients were collected from the Hidradenitis Suppurativa Clinic of the Hospital Universitario Virgen de las Nieves.
Ethics
This study was approved by the Institutional Review Board of the Hospital Universitario Virgen de las Nieves and is in accordance with the Declaration of Helsinki.
Inclusion Criteria
The inclusion criteria were (a) patients with clinical diagnosis of HS; (b) patients suffering from severe HS who started biologic treatment with adalimumab according to international guidelines for HS [9]; (c) informed consent from the patient of the legal representatives to be included in the study.
Exclusion Criteria
The exclusion criteria were (a) refusal from the patient or legal representative to participate in the study; (b) patients suffering from HS who were not candidates to be treated with adalimumab.
Variables of Interest
Main Variables
The patients were assessed two times: firstly, the day of the initiation of their biologic treatment; secondly, 32 weeks after, as previously performed in similar studies [4]. The main variables considered included those associated with cardiovascular risk assessment and those related to disease severity.
-
(A)
Cardiovascular risk factors were evaluated by performing blood tests, clinical examination, and carotid artery ultrasonography:
-
(a)
Carotid intima–media thickness (IMT): IMT was assessed in both carotid arteries of the patients by using ultrasonography as previously described [4]. Briefly, left, right, and mean IMT were recorded using a high-resolution ultrasound (Esaote MyLab Gold 25) with a 12-mHz sounding line running specific software for measuring ITM (Esaote QIMT Software). The definitive value of the IMT measurements was obtained by calculating the average of six valid measurements taken from the sonographic scanning. To explore potential predictors of IMT reduction patients were classified qualitatively in terms of IMT reduction as IMT responders (improvement of IMT between week 0 and week 32 of at least 1 µm) and IMT non-responders (patients not meeting the “IMT responders” criteria).
-
(b)
Clinical data: Patients were explored to assess the body mass index (BMI), the metabolic syndrome criteria (ATPIII criteria) [11], and tobacco consumption (cigarettes/day).
-
(c)
Other blood biomarkers: Different measurements were performed in patients following an 8-h fasting period. Recorded blood parameters included basal glucose, basal insulin, HOMA score, glycated hemoglobin, triglycerides, HDL and LDL cholesterol, transaminases, albumin, parathyrin, vitamin D, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP).
-
(a)
-
(B)
Disease severity was assessed using disease activity indexes:
-
(a)
The International HS Severity Scoring System (IHS4) was used to assess inflammatory activity. It was calculated using the following formula: (number of nodules × 1) + (number of abscesses × 2) + (number of fistulas × 4) [12]. The reduction of 55% in the IHS4 score was also collected (IHS4-55) [13].
-
(b)
The Hurley classification was used to assess structural damage. It consists of three stages (I, presence of abscesses without fistulous tracts or scars; II, recurrent abscesses and single or multiple fistulae and scars widely separated between them; III, abscesses and confluent fistulas with large areas of extensive scarring) [14].
-
(a)
Other Variables
Sociodemographic, biometric, and clinical variables, including age, sex, comorbidities, and previous treatments for HS, were recorded by clinical interview and physical examination.
Statistical Analysis
Descriptive statistics were used to evaluate the characteristics of the sample. The Shapiro–Wilk test was used to assess the normality of the variables. Continuous variables are expressed as mean and standard deviation (SD). Qualitative variables are expressed as relative and absolute frequency distributions. The χ2 test or Fisher’s exact test, as appropriate, was used to compare nominal variables, and Student’s t test or Wilcoxon–Mann–Whitney test was used to compare between nominal and continuous data. To explore possible associated factors, simple linear regression was used for continuous variables. The β coefficient and SD were used to predict the log odds of the dependent variable. Significantly associated variables (p < 0.05) or those showing trends towards statistical significance (p < 0.20) were included in multivariate analysis. Statistical significance was considered if p values were less than 0.05. Statistical analyses were performed using JMP version 9.0.1 (SAS institute, North Carolina, USA).
Results
Sociodemographic and Basal Clinical Features of the Sample
Twenty-seven patients with severe HS were included in the study. The male to female ratio was 2:1, and the mean age of the sample was 37 years old (SD 13.68). Family history of HS was present in 37% (10/27) of the patients, Table 1. Basal IHS4 mean score was 19.48 (SD 8.11), which indicated severe disease. Furthermore, 51.8% (14/27) of the patients were classified as Hurley III stage. Patients had suffered from HS for a mean of 21.96 years (SD 10.31). Detailed information about comorbidities can be seen in Table 1.
Distribution of Cardiovascular Risk Markers in the Sample
Previously diagnosed prevalence of diabetes mellitus and dyslipidemia was 3.7% (1/27) and 7.4% (2/27), respectively (Table 2). Basal glycemia, basal insulin, and mean HOMA index indicated a high prevalence of insulin resistance in the sample: mean HOMA index was close to the threshold of 3 which is considered to diagnose insulin resistance. Obesity had a high prevalence in the sample and appeared in 33.3% (9/27) of the patients with a mean BMI of 39.60 (SD 8.25). High blood pressure had been diagnosed in 11.1% (3/27) of patients, and 48% of patients were smokers (13/27). Finally, 26% (13/50) of the patients met criteria for metabolic syndrome.
Evolution of Disease Severity and Other Clinical Features After Adalimumab Treatment
After 8-month treatment with adalimumab, disease severity improved in the sample. Basal IHS4 score (19.48, SD 8.11) decreased at 32 weeks (9.03, SD 9.83) (p < 0.01). IHS4-55 response was obtained in 70.3% (19/27) of the patients. On the other hand, no significant differences were found over time in terms of BMI (p = 0.42), HOMA index (p = 0.37), HbA1c levels (p = 0.75), CRP levels (p = 0.62), erythrocyte sedimentation rate (p = 0.42), or vitamin D levels (p = 0.50).
Evolution of Carotid IMT Under Adalimumab Treatment and Predictors of IMT Responders
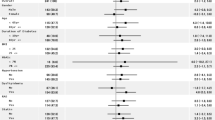
Overall there were no differences in mean IMT between baseline (633.92 µm) and 32 weeks follow-up (634.39 µm) (p = 0.98). However, there was a subset of 40.7% (11/27) of the patients who were IMT responders, i.e., they showed an improvement in IMT over time. The non-IMT responders group increased their mean IMT value from 606 to 668 µm over time, whereas the IMT responders group had a significant decrease of IMT over time, from 673 to 585 µm (p < 0.001). A univariate analysis was performed to detect basal clinical and biochemical characteristics which were associated with the cardiovascular risk improvement group (Table 3). In this regard, some variables showed tendency towards statistical significance: patients who had an IMT improvement when compared to those without it were more likely to have some characteristics. This group had a higher prevalence of dyslipidemia (p = 0.05), diabetes mellitus (p = 0.18), and had higher HbA1c levels (p = 0.12) at baseline. Moreover, these patients had higher BMI (p = 0.19), higher levels of CRP (p = 0.17), consumed more tobacco (p = 0.14), and had less basal inflammatory burden (p = 0.22). Finally, patients who improved IMT tended to have a greater IMT basal value (p = 0.08), but no relationship was found between inflammation reduction (IHS4-55 achievement) and IMT reduction (p = 0.72). Interestingly, those patients who did not improve IMT over time showed tendency towards higher 32-week CRP levels (difference 3.96, p = 0.58) and higher 32-week IHS4 scores (difference 1.75, p = 0.65). A correlation analysis showed similar results for quantitative variables (Fig. 1).
Discussion
Adalimumab treatment might benefit a subset of patients with HS in terms of cardiovascular risk reduction. In light of the results of the present study, those patients with less severe disease, those with classical cardiovascular risk factors (such as glycemic disorders, diabetes mellitus, high blood pressure, higher BMI, or tobacco consumption), and those with higher burden of subclinical atherosclerosis would more likely to improve their IMT under adalimumab treatment. On the contrary, those patients with higher inflammatory load after treatment could be more prone to have a lack of improvement of IMT.
HS has been previously linked to increased cardiovascular risk [1, 2, 15]. The biological association of both entities is connected with the already known link between inflammation and atherosclerosis. In this regard, a chronic inflammatory burden could accelerate the atheroma plaque formation process, therefore resulting in an early appearance of cardiovascular events [16].
Regarding cardiovascular risk measurement, apart from classical cardiovascular risk factors and clinical scores [17, 18], carotid IMT measurement by means of ultrasound has become a practical tool to stratify cardiovascular risk [6]. Moreover, IMT has already been associated with other classic CVR factors, such as insulin resistance and glycemic disorders [15], as well as with poorer cardiovascular outcomes in a variety of populations [19,20,21]. On the other hand, the low rate of smokers in our study could lead to bias due to the limited sample size. Moreover, as the patients suffered from a severe disease, this could have led to a reduced smoking rate as the patients might be concerned with the importance of smoke avoidance.
Our study aimed to assess IMT evolution over time in patients with HS under adalimumab treatment. However, although global evaluation showed no differences in IMT over time, we identified the profile of patients who had an improvement in IMT after 32 weeks of adalimumab treatment.
Similar studies have been performed for other skin and non-skin diseases. Martínez-López et al. [4] studied the evolution over time of IMT and insulin in patients with psoriasis under treatment with biologic drugs (anti-TNF and anti-IL12/23) and classic systemic psoriasis drugs (such as methotrexate). This study showed how patients under anti-TNF treatment improved their insulin levels, but had no changes in IMT after 32 weeks of treatment. However, as in our study, sample size could have been insufficient for detecting significant differences, and these authors did not perform any stratified analysis for defining an “IMT-improvement group”. More recent studies have demonstrated the potential benefit of anti-TNF treatment in terms of IMT improvement in other inflammatory diseases, such as rheumatoid arthritis, regardless of the specific drug employed [22].
Finally, in light of the results of this pilot study, IMT could be a predictive biomarker of CVR in patients with HS. As previously described [23], there are many useful ultrasonographic markers in HS, such as dermal vascularization. Moreover, other measurements such as CRP or ESR seem to be predictive biomarkers. Future studies for IMT would be of great interest.
The main limitations of the present study are the limited sample size, which could have limited the detection of significant differences, and the lack of a control group.
Conclusions
Adalimumab treatment seems to be potentially associated with cardiovascular risk improvement in HS who have cardiovascular risk factors and subclinical atherosclerosis. Further investigation on this issue might be of great interest to improve treatment guidelines taking into account not only disease severity and comorbidities but also cardiovascular risk stratification.
References
Cuenca-Barrales C, Montero-Vilchez T, Salvador-Rodríguez L, Sánchez-Díaz M, Arias-Santiago S, Molina-Leyva A. Implications of hidradenitis suppurativa phenotypes in cardiovascular risk and treatment decisions: a retrospective cohort study. Dermatology. 2021;237(5):727–32.
Hung C-T, Chiang C-P, Chung C-H, Tsao C-H, Chien W-C, Wang W-M. Increased risk of cardiovascular comorbidities in hidradenitis suppurativa: a nationwide, population-based, cohort study in Taiwan. J Dermatol. 2019;46(10):867–73.
González-López MA, Ocejo-Viñals JG, López-Sundh AE, et al. Biomarkers of endothelial dysfunction and atherosclerosis in hidradenitis suppurativa. J Dermatol. 2022;49(10):1052–6.
Martinez-Lopez A, Blasco-Morente G, Perez-Lopez I, Tercedor-Sanchez J, Arias-Santiago S. Studying the effect of systemic and biological drugs on intima-media thickness in patients suffering from moderate and severe psoriasis. J Eur Acad Dermatol Venereol. 2018;32(9):1492–8.
Rezaieyazdi Z, Sedighi S, Salari M, et al. Investigation of the association between carotid artery intima-media thickness (IMT) and cardiac risk factors in patients with systemic lupus erythematosus. Curr Rheumatol Rev. 2020;16(2):125–33.
Smrzova A, Horak P, Skacelova M, et al. Intima media thickness measurement as a marker of subclinical atherosclerosis in SLE patient. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014;158(3):404–11.
González-López MA, Hernández JL, Lacalle M, et al. Increased prevalence of subclinical atherosclerosis in patients with hidradenitis suppurativa (HS). J Am Acad Dermatol. 2016;75(2):329–35.
González-López MA, Lacalle M, Mata C, et al. Carotid ultrasound is useful for the cardiovascular risk stratification in patients with hidradenitis suppurativa. PLoS ONE. 2018;13(1):e0190568.
Zouboulis CC, Desai N, Emtestam L, et al. European S1 guideline for the treatment of hidradenitis suppurativa/acne inversa. J Eur Acad Dermatol Venereol. 2015;29(4):619–44.
Glovaci D, Fan W, Wong ND. Epidemiology of diabetes mellitus and cardiovascular disease. Curr Cardiol Rep. 2019;21(4):21.
Marchesini G, Forlani G, Cerrelli F, et al. WHO and ATPIII proposals for the definition of the metabolic syndrome in patients with type 2 diabetes. Diabet Med. 2004;21(4):383–7.
Zouboulis CC, Tzellos T, Kyrgidis A, et al. Development and validation of the International Hidradenitis Suppurativa Severity Score System (IHS4), a novel dynamic scoring system to assess HS severity. Br J Dermatol. 2017;177(5):1401–9.
Tzellos T, van Straalen KR, Kyrgidis A, et al. Development and validation of IHS4–55, an IHS4 dichotomous outcome to assess treatment effect for hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2022. https://doi.org/10.1111/jdv.18632.
Ovadja ZN, Schuit MM, van der Horst CMAM, Lapid O. Inter- and intrarater reliability of Hurley staging for hidradenitis suppurativa. Br J Dermatol. 2019;181(2):344–9.
Sánchez-Díaz M, Salvador-Rodríguez L, Montero-Vílchez T, Martínez-López A, Arias-Santiago S, Molina-Leyva A. Cumulative inflammation and HbA1c levels correlate with increased intima-media thickness in patients with severe hidradenitis suppurativa. J Clin Med. 2021;10(22):5222.
Mazidi M, Katsiki N, Mikhailidis DP, Banach M. Association of ideal cardiovascular health metrics with serum uric acid, inflammation and atherogenic index of plasma: a population-based survey. Atherosclerosis. 2019;284:44–9.
Koliaki C, Liatis S, Kokkinos A. Obesity and cardiovascular disease: revisiting an old relationship. Metabolism. 2019;92:98–107.
Sans S, Fitzgerald AP, Royo D, Conroy R, Graham I. Calibrating the SCORE cardiovascular risk chart for use in Spain. Rev Esp Cardiol. 2007;60(5):476–85.
de Oliveira AN, Simões MM, Simões R, Malachias MVB, Rezende BA. Cardiovascular risk in psoriasis patients: clinical, functional and morphological parameters. Arq Bras Cardiol. 2019;113(2):242–9.
Im CH, Kim NR, Kang JW, et al. Inflammatory burden interacts with conventional cardiovascular risk factors for carotid plaque formation in rheumatoid arthritis. Rheumatology (Oxford). 2015;54(5):808–15.
Naqvi TZ, Lee M-S. Carotid intima-media thickness and plaque in cardiovascular risk assessment. JACC Cardiovasc Imaging. 2014;7(10):1025–38.
Anghel D, Sîrbu CA, Hoinoiu E-M, et al. Influence of anti-TNF therapy and homocysteine level on carotid intima-media thickness in rheumatoid arthritis patients. Exp Ther Med. 2022;23(1):59.
Der Sarkissian S, Hessam S, Kirby JS, et al. Identification of biomarkers and critical evaluation of biomarker validation in hidradenitis suppurativa: a systematic review. JAMA Dermatol. 2022;158(3):300–13.
Acknowledgements
We thank the participants in the study for their disinterested collaboration, which has allowed us to advance in the study of the disease.
Funding
No funding or sponsorship was received for this study or publication of this article.
Disclosures
Manuel Sánchez-Díaz has nothing to disclose. Luis Salvador-Rodríguez has nothing to disclose. Carlos Cuenca-Barrales has nothing to disclose. Salvador Arias-Santiago has nothing to disclose. Alejandro Molina-Leyva has nothing to disclose.
Author Contributions
Manuel Sánchez-Díaz, Luis Salvador-Rodríguez and Carlos Cuenca-Barrales collected the data. Salvador Arias-Santiago and Alejandro Molina-Leyva reviewed the research. Manuel Sánchez-Díaz, Luis Salvador-Rodríguez and Alejandro Molina-Leyva wrote the manuscript. Manuel Sánchez-Díaz, Carlos Cuenca-Barrales and Alejandro Molina-Leyva performed the statistical analysis. Carlos Cuenca-Barrales and Salvador Arias-Santiago performed the manuscript revision. Salvador Arias-Santiago and Alejandro Molina-Leyva designed the project.
Compliance with Ethics Guidelines
This study was approved by the Research Ethics Committee of the Virgen de las Nieves Hospital. The patients in this manuscript have given written informed consent to publication of their case details. This study is in accordance with the Declaration of Helsinki.
Data Availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sánchez-Díaz, M., Salvador-Rodríguez, L., Cuenca-Barrales, C. et al. Potential Predictors of Cardiovascular Risk Improvement in Patients with Hidradenitis Suppurativa Treated with Adalimumab: A Pivotal Study of Factors Associated with Carotid Intima–Media Thickness Reduction. Dermatol Ther (Heidelb) 13, 817–826 (2023). https://doi.org/10.1007/s13555-023-00898-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-00898-z