Abstract
Introduction
This study explored patients’ and dermatologists’ priority outcomes for treatment to address, clinical outcome assessments (COA) for use in vitiligo clinical trials, and perceptions of within-patient meaningful change in facial and total body vitiligo.
Methods
Semistructured, individual, qualitative interviews were conducted with patients living with non-segmental vitiligo in the USA and with expert dermatologists in vitiligo. Concept elicitation discussions included open-ended questions to identify patient priority outcomes. Vitiligo COAs were reviewed by dermatologists. Tasks were completed by patients to explore their perceptions of meaningful changes in vitiligo outcomes; dermatologists’ opinions were elicited. Data were analyzed using thematic methods; meaningful change tasks were descriptively summarized.
Results
Individuals with vitiligo (N = 60) included adults (n = 48, 63% female) and adolescents (n = 12, 67% female). All Fitzpatrick Skin Types were represented. Eight (13%) were first- or second-generation immigrants to the USA. Expert dermatologists (N = 14) participated from the USA (n = 8), EU (n = 4), India (n = 1), and Egypt (n = 1). All individuals with vitiligo reported experiencing skin depigmentation; an observable clinical sign of vitiligo. Most confirmed that lesion surface area (n = 59/60, 98%) and level of pigmentation (n = 53/60, 88%) were important to include in disease assessments. Following an explanation, participants (n = 49/60, 82%) felt that the Facial Vitiligo Area Scoring Index (F-VASI) measurement generally made sense and understood that doctors would use it to assess facial vitiligo. Most participants felt that a 75% (n = 47/59, 80%) or 9 0% improvement in their facial vitiligo would be indicative of treatment success (n = 55/59, 93%). In the context of evaluating a systemic oral treatment for vitiligo, dermatologists perceived a 75% improvement on the F-VASI as successful (n = 9/14, 64%). Regarding the Total VASI (T-VASI) score, n = 30 participants considered 33% improvement as treatment success; an additional n = 10 endorsed 50% improvement and a further n = 5 endorsed 75% improvement. Clinicians most frequently identified 50% (n = 6/14, 43%) or 75% (n = 4/14, 29%) improvement in T-VASI as successful.
Conclusion
Repigmentation is a priority outcome for patients. The VASI was considered an appropriate tool to assess the extent of vitiligo. A minimum 75% improvement from baseline in the F-VASI and minimum 50% improvement from baseline in the T-VASI were identified as within-patient clinically meaningful thresholds.
Similar content being viewed by others
The Vitiligo Area Scoring Index (VASI) is a clinician-reported outcome that assesses affected body surface area and level of depigmentation. Research to date has identified different treatment-success thresholds through different methods of inquiry. However, a definition for success is still required for evaluating vitiligo treatments. |
This study used innovative, qualitative methods to explore patients’ and dermatologists’ perspectives on priority outcomes for vitiligo treatment to address, clinical outcome assessments (COAs) to measure those outcomes in vitiligo clinical trials, and perceptions of meaningful within-patient changes in vitiligo outcomes. |
The study confirmed that repigmentation is an outcome of priority for vitiligo patients. The VASI was considered an appropriate tool to assess the extent of vitiligo in clinical trials for vitiligo treatments. |
A minimum 75% improvement from baseline in the Facial Vitiligo Area Scoring Index (F-VASI) and minimum 50% improvement from baseline in the T-VASI were identified as clinically meaningful thresholds endorsed by individuals living with vitiligo. |
Introduction
Vitiligo is a chronic autoimmune disease characterized by white macules due to melanocyte destruction [1]. Vitiligo can be limited in extent or involve multiple body sites and large body surface area (BSA) [2]. The Vitiligo Area Scoring Index (VASI) is a clinician-reported outcome (ClinRO) that assesses affected BSA and level of depigmentation [3]. The VASI yields a single score for the body [sometimes referred to as Total Body VASI (T-VASI)]. Recent clinical trials have assessed vitiligo involvement of the face, i.e., the Facial VASI (F-VASI) score, separate from the body, i.e., the T-VASI [4]. The VASI has demonstrated high inter- and intra-observer reliability scores, [5] and the F-VASI and T-VASI have demonstrated strong test–retest reliability, known-groups validity, and responsiveness to change [4].
One hand unit (i.e., the palm plus the volar surface of all fingers; ~ 1% of the total body surface area) is used to measure the extent of vitiligo involvement of several body regions, including the head and neck, hands, upper extremities, trunk, lower extremities, and feet [4]. The extent of depigmentation within each affected lesion is assessed using predefined percentages: 0%, 10%, 25%, 50%, 75%, 90%, or 100%. The T-VASI is calculated using \(\Sigma \left[Hand units\right] \times \left[Residual Depigmentation\right]\), and is summed (\(\Sigma )\) for all body regions. The face, and therefore F-VASI, contributes 3–3.5% of the total BSA [4, 6] and is included in the T-VASI score.
To execute patient-focused drug development, patients’ experiences, perspectives, and priorities must be meaningfully incorporated into the evaluation of medical products [7,8,9,10] via well-defined and reliable (i.e., fit-for-purpose) clinical outcome assessments (COAs). An important component of fit-for-purpose evidence is content validity, i.e., evidence that the COA measures what matters to patients [8]. In the context of vitiligo, it is important for stakeholders to understand: (1) what are the most important vitiligo treatment outcomes for patients living with nonsegmental vitiligo, and (2) the level of improvement that constitutes clinical benefit from the patient perspective. Intuitively we understand that achieving 100% repigmentation would be a clinical treatment success. However, when repigmentation is less than 100%, we need to understand what patients consider to be meaningful treatment benefit [11].
The Vitiligo Global Issues Consensus Conference (VGICC) explored treatment success with dermatologists, patients/caregivers, and healthcare professionals through an eDelphi study. Findings indicated that treatment of a single lesion was successful if repigmentation exceeded 80% and at least 80% of the gained repigmentation was maintained for > 6 months [12]. The International Initiative for Outcomes (INFO) for vitiligo conducted clinician-led workshops with patients or their caregivers. The consensus for the definition of “successful repigmentation” from the patient perspective was 80% to 100% of repigmentation of a single lesion [13]. Furthermore, patients found achieving ≥ 25% repigmentation after 3 months of treatment to be a satisfactory intermediate result, where they would be willing to continue treatment [13]. The face, neck, and hands were considered the most important locations to achieve satisfactory results [13]. Rosmarin et al. [4] explored clinically meaningful change in F-VASI and T-VASI using an anchor-based approach with phase 2 data, and concluded that a 57% reduction in F-VASI and a 42% reduction in T-VASI were considered clinically meaningful. F-VASI75 (75% reduction from baseline) and T-VASI50 (50% reduction from baseline) thresholds were proposed to ensure that phase 3 endpoints set a higher bar for treatment success than those determined by anchor-based analyses.
Research to date has identified different treatment-success thresholds through various methods, and mainly focused on level of repigmentation only. A definition for success is still required for evaluating vitiligo treatments and was a recent topic of discussion in the FDA-led Patient Focused Drug Development (PFDD) Meeting for Vitiligo [11]. A within-patient meaningful change threshold is typically confirmed through anchor-based analyses but can also be informed by qualitative exploration, seeking direct input from patients and experts to explore not only what the threshold should be, but also the impact that this change may have on how patients feel and function[14].
The objectives of this study were to conduct systematic, qualitative, semistructured interviews with individuals living with vitiligo and expert clinicians, to:
-
1.
Identify the vitiligo treatment outcomes of priority that are most meaningful and most important to improve for defining clinical benefit from the patient and clinician perspectives, including the development of a Vitiligo Consequence Model.
-
2.
Further explore the percentage change in repigmentation that patients with vitiligo consider necessary for successful treatment of both the face and body, specifically the F-VASI and T-VASI.
-
3.
Document the impact of vitiligo on how patients feel and function, the results of which are reported elsewhere [15].
-
4.
Meet regulators’ requirement [8] for direct input from vitiligo patients to provide definitive supportive evidence for priority treatment outcomes and what constitutes meaningful changes for vitiligo.
The qualitative evidence generated from this research can be used to: (a) document meaningful outcomes to patients, e.g., addressing depigmentation as an outcome of priority to patients, and (b) establish clinically meaningful changes in outcomes from the patient perspective. The current study was specific to the VASI scoring approach as a whole (including both repigmentation and surface area in the score), and ensures understanding of what a meaningful change is for patients in both their facial vitiligo and their total body vitiligo.
Methods
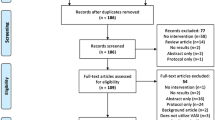
This study was a noninterventional, cross-sectional, qualitative interview study. The study protocol was approved by WIRB-Copernicus Group independent review board (WCG IRB). The methodology is illustrated in Supplementary Material 1.
Interviews with Individuals Living with Vitiligo
Eligibility Criteria
Individuals were eligible to participate if aged ≥ 12 years, US residents, and had nonsegmental, active vitiligo, with lesions on the face and/or body affecting 4–60% of their total BSA with at least 0.25% BSA on their face, according to their most recent clinician assessment. Individuals were excluded if they had segmental or mixed vitiligo, were enrolled in a vitiligo clinical trial, or had active comorbid inflammatory skin disease. Following 4 months of recruitment, the eligibility criteria were amended to include adolescents with either 4–60% BSA impacted by vitiligo or ≥ 0.25% BSA on the face.
Purposive sampling targeted a representative sample, including each of the six Fitzpatrick Skin Types (FSTs) and with different education levels, an important consideration when evaluating outcome measures (Supplementary Material 2).
Recruitment
Participants were identified via specialist recruiters (Global Perspectives), clinical sites (Northwest Dermatology Institute, Oregon and Dawes-Fretzin Dermatology, Indianapolis) or advertisements (via The Global Vitiligo Foundation). Individuals provided written informed consent/assent. Eligibility was confirmed via a clinician-completed case report form (CRF). Demographic information was collected via a self-report screener.
Interview Procedures
Interviews took place between November 2020–March 2021, during the COVID-19 pandemic. To avoid risk, all interviews were conducted remotely. Using a semi-structured interview guide, interviews were conducted by trained, qualitative interviewers and lasted approximately 2 h.
Concept elicitation [16, 17] was utilized to explore the impact of vitiligo. Open-ended questions were designed to elicit concepts for a Vitiligo Consequence Model spontaneously, followed by in-depth probe questions on concepts of interest. Questions explored patients’ perspectives on the priority outcomes of vitiligo for treatment to address, measurement of these outcomes, and the types of changes that they consider meaningful for treatment success.
Next, the F-VASI scoring approach was explained using a visual aid (Fig. 2), utilizing the most recently published definition of the face area [4].The measurement components of the VASI (e.g., affected BSA and level of depigmentation) were described to patients to elicit their feedback as to whether the components measured their priorities.
The interviewer then introduced activities to explore meaningful change representative of clinical benefit from the patient perspective. Participants were asked about times when their vitiligo improved and worsened. Next, they were shown five “before and after treatment” photographs of faces with different improvements in depigmentation. The photos were “real” images (i.e., not digitally altered) of individuals’ facial vitiligo taken before and after participating in a clinical trial. To protect the individuals’ privacy, the images are not included in this publication. Improvement in depigmentation and surface area on the images were determined by two raters, using the VASI scoring system. The photographs of facial vitiligo included representation of at least two FST skin types.
Patients were then shown illustrative graphics for percentage change (from different baseline scores) to facilitate their understanding and inform their decision making (Fig. 3). After viewing the provided examples, patients were asked to consider treatment success for themselves and their own vitiligo experience, e.g., what percentage change (improvement) in depigmentation would be indicative of treatment success?
Interviews with Expert Clinicians
Sampling and Recruitment
International expert clinicians were selected from a list provided by the study sponsor (Pfizer), on the basis of their experience in vitiligo research and clinical trials. All clinicians signed an informed consent form (ICF) before participating.
Interview Procedures
One-hour interviews were conducted remotely using screen share software, allowing international participation and avoiding COVID-19 exposure risks. Interviewers used a semi-structured interview guide including open-ended questions with follow-up probes to explore clinicians’ experience treating individuals with vitiligo. Clinicians discussed vitiligo assessment in clinical practice and clinical trials, including the use of ClinROs (e.g., the VASI). Then, clinicians were asked to state the percentage change from baseline on the F-VASI and T-VASI that they would consider to be a treatment success in the context of a systemic, oral treatment.
Analysis of Interviews
Weekly interviewer meetings were held to discuss interview findings, aid consistency in approach, and inform interview guide updates. All interviews were audio recorded and transcribed verbatim. Transcripts were analyzed using ATLAS.ti version 7.5.
Meaningful change activities were subject to framework analysis, whereby a pre-defined code list was applied to identify percentage changes considered meaningful in F-VASI and T-VASI scores. Frequency counts summarized patients’ responses. The research team identified the percentage improvement that appeared to be indicative of treatment success on the basis of the frequency of responses at each level that most participants perceived as successful and few perceived as unsuccessful.
Steering Committee
A steering committee comprising two clinical experts in vitiligo and a patient advocate guided this research. The steering committee members reviewed the patient interview guide, clinician interview guide and/or interpreted the study results.
Results
Sample
Sixty individuals living with vitiligo (n = 48 adults and n = 12 adolescents) (Table 1) participated. Most participants were female. Representation of lower education levels was achieved. The sample included eight participants who were first- or second-generation living in the USA. No FST group was significantly over- or under-represented; each group accounted for 10–23% of the total sample. Under the expanded enrollment criteria, one adolescent had vitiligo on their body only and one had vitiligo on their face only. Additional sample characteristics are provided in Supplementary Material 3.
Fourteen expert clinicians were recruited, including from the USA (n = 8), Europe (n = 4) and the rest of the world (n = 2); most worked at university-affiliated hospitals, and some had previously developed vitiligo-specific ClinRO measures.
Concept Elicitation
All individuals living with vitiligo (n = 60/60) reported experiencing areas of skin depigmentation, the cardinal clinical sign of vitiligo. Depigmentation was also reported as a key sign by all expert clinicians.
-
“I’ve had pretty much all of my life that I can remember, and it’s, err, large, white areas all over me.” (male, 14 years old)
-
“Non-segmental vitiligo, you will see depigmented patches, so, lack of pigmentation or skin coloring.” (US clinician)
When discussing desired treatment benefits, over half of individuals with vitiligo (n = 39/60, 65%) reported that they would specifically want skin repigmentation to occur, and many reported wanting a decrease in the skin surface area of vitiligo (n = 29/60, 48%), and/or a reduction in the noticeability of vitiligo (n = 23/60, 38%).
-
“Maybe more, um, like, um, like normal skin, rather than having, like, vitiligo.” (female, 13 years old)
-
“Um, well, the pigment reoccurring in the areas where it’s gone away.” (male, 57 years old)
Individuals with vitiligo identified their face (n = 52/60, 87%), hands (n = 42/60, 70%), and legs (n = 21/60, 35%) among the top three most bothersome locations of vitiligo; the face was considered the most important area for a treatment to improve (n = 40/54, 74%). Expert clinicians also identified the face (n = 14/14, 100%) and hands (n = 13/14, 93%) as the areas they perceived to be most bothersome to individuals living with vitiligo.
A Vitiligo Consequence Model is presented in Fig. 1 and full concept elicitation findings are reported separately.
Conceptual Relevance of the VASI
The F-VASI and T-VASI scoring was explained to all individuals living with vitiligo (using the illustrative graphic in Fig. 2). Nearly all confirmed that lesion surface area (n = 59/60, 98%) and level of pigmentation (n = 53/60, 88%) were important disease characteristics to include in vitiligo assessments.
Most participants felt the F-VASI (n = 49/60, 82%) and T-VASI (n = 54/60, 90%) scoring made sense, and understood that doctors would use this to assess the level of vitiligo. When asked if anything was missing from the F-VASI scoring process or the facial definition presented [4], n = 16 patients (n = 16/53 asked, 30%) reported that eyelids and lips should be included in the F-VASI assessment.
All expert clinicians were familiar with use of the VASI in research, although only two used it in clinical practice. Clinicians perceived the VASI to be a validated framework for assessing vitiligo (n = 8), and noted it as an advantage that both affected surface area and level of depigmentation are included in the scoring (n = 5). Noted disadvantages included: the VASI can be time consuming and somewhat difficult to use (n = 7), and the scoring approach may be subject to human error or rater discrepancy (n = 6).
Meaningful Change Thresholds: F-VASI
Participants (n = 59) viewed photographs of individuals with facial vitiligo “before and after treatment,” representing 50%, 75%, and 90% improvements from baseline within different FSTs, to assist their conceptualization of percentages changes on the F-VASI. To protect the privacy of the individuals in the photographs, the images have not been included in this publication.
Participants also viewed illustrative graphics depicting 50%, 75%, and 90% improvement, with each level of change illustrated using three different baseline scores on the F-VASI (example in Fig. 3). After reviewing the graphics, individuals were asked to consider the F-VASI improvement that would be a treatment success in the context of their own vitiligo experience.
Over half of participants (n = 39/59, 66%) felt that a 50% improvement from baseline in their own facial vitiligo would be indicative of treatment success. However, 12 patients (21%) stated that 50% improvement in facial vitiligo would not be indicative of treatment success, as they perceived that there would still be visible vitiligo on their face.
-
“If somebody said, ‘We can reduce the, the depigmentation by 50%,’ I don’t think 50% would really make too much of a difference in terms of my face, um, because it would still leave quite a bit covered. And, again, I don’t know if it would seem so worth it to me.” (female, 48 years old)
Most participants felt that a 75% (n = 47/59, 80%) or 90% improvement (n = 55/59, 93%) would be indicative of treatment success (Table 2). Patients felt that both levels of improvement would lead to less visible areas of vitiligo and subsequently would alleviate the emotional and social impacts experienced.
-
“I feel like at 75% it’s getting to, um, kind of a, a, a big degree of change that it’s almost, kind of, as a whole, being reduced so much. Whereas 50% is, um—it could still be, err, large chunks, um, no matter, kind of, where you started.” (male, 22 years old)
-
[Describing a 90% improvement] “It would mean the world of difference. I’d be able to do so many more things that I don’t do now. No more makeup, no more coverup. Not afraid to go next to somebody. Not afraid, not afraid of the coverup coming off and destroying somebody’s shirt, or whatever. I would be, I would be extremely happy.” (female, 59 years old)
Only 5% of participants felt that a 75% improvement was not indicative of treatment success; noting that it would be an improvement but not a definitive success. The research team concluded that a minimum 75% improvement from baseline was indicative of treatment success on the basis of the frequency of responses at each level that most participants perceived as successful/somewhat successful and few perceived as unsuccessful.
Sub-group analysis compared responses between adults and adolescents (Supplementary Material 4). Adults were less likely to endorse the lower thresholds; however, endorsement of the highest percentage improvement levels was broadly consistent between adults and adolescents.
Most queried participants (n = 24/32, 75%) indicated that they would be happy with a 50% improvement in their facial vitiligo after 12 months of treatment; slightly more would be happy with a 75% improvement (n = 26/32, 81%) or a 90% improvement (n = 24/26, 92%). Participants expected a 75% improvement in their own facial vitiligo would reduce the emotional impact of vitiligo (n = 11), stop vitiligo being noticed by others (n = 4), reduce need for concealment (n = 4), reduce social impacts of vitiligo (n = 3), and/or reduce need for sun protection (n = 3).
-
“Um, more confidence, more self-esteem, more higher self-esteem.” (female, 24)
-
“No more coverup. I’ll be able to socialize a little more.” (female, 59)
Expert clinicians provided the percentage change from baseline in F-VASI that they would consider a treatment success in the context of a systematic oral treatment (Fig. 4). Nine of the 14 clinicians provided the most frequent response of 75% improvement from baseline (range 50–90%). Some clinicians noted that 50% improvement could be achieved through currently available topical treatments, and therefore, a greater improvement should be expected from an oral systemic treatment, considering the potential risks.
F-VASI% and T-VASI% that represents success for a systemic, oral treatment. *Note that for T-VASI Clin_01 proposed a range of 25–50%, the lowest score is shown here. Clin_09 proposed a range of 70–80%, the lowest score is shown here, Clin_07 noted that 75% could be minimally successful, but only if the patient could progress to 90%, therefore the higher score is shown here
Meaningful Change Thresholds: T-VASI
Participants (n = 50) were asked whether a 33%, 50%, or 75% improvement from baseline on the T-VASI would be indicative of a treatment success (Table 2). Most considered 33% improvement (n = 30) as treatment success; an additional n = 10 participants endorsed 50% improvement, and n = 5 participants endorsed 75% improvement. Eleven participants noted that 33% improvement would not be a success. Subgroup analysis compared responses between adults and adolescents (Supplementary Material 4).
Therefore, the research team identified a minimum 50% improvement from baseline as indicative of treatment success on the basis of the frequency of successful/somewhat successful responses compared with the frequency of unsuccessful responses. Participants expected a 50% improvement in their own total body vitiligo to reduce the emotional impacts associated with vitiligo (n = 5), and/or reduce the need to conceal vitiligo with clothing (n = 2), improve intimacy, and reduce sun protection efforts (each n = 1).
Expert clinicians identified the percentage change from baseline in T-VASI that would be considered a treatment success (Fig. 4). The most frequent response was a 50% improvement from baseline (n = 6/14, 43%), followed by a 75% improvement (n = 4/14, 29%). All clinicians who suggested a 50% improvement considered this outcome to be acceptable after 6 months of treatment, although two clinicians said it was only acceptable if an even greater percentage improvement was later achieved (e.g., after 12 months).
Discussion
This study explored meaningful treatment outcomes for patients with nonsegmental vitiligo. The first objective was to identify the vitiligo outcomes that are most meaningful to patients, and the overall priority outcome is repigmentation. Most patients thought it was most important for a treatment to improve the vitiligo on their face. As an observable clinical sign, it is appropriate that vitiligo should be assessed by clinicians with training relevant to the measurement of BSA and depigmentation. The VASI scoring and component measurement concepts (surface area and depigmentation) were confirmed to assess what individuals living with vitiligo consider to be important. Comprehensive training is required for the VASI. While most interviewed clinicians considered it to be a useful assessment tool, some noted the time commitment, difficulty, and risk of human error worth consideration.
The second objective was to explore the percentage change in depigmentation that patients with vitiligo consider necessary for successful treatment. Previous research suggested that a successful treatment would involve 80% repigmentation of a single lesion [12, 13], with limited evidence regarding meaningful change [4] on the F-VASI and T-VASI. In the current study, patients were shown photos of full body regions (face or total body) rather than a single lesion, encouraging them to consider multiple lesions. This may have allowed patients to perceive changes in affected BSA in addition to depigmentation. The results of the current study suggest that a minimum 75% improvement from baseline on the F-VASI can be considered a meaningful treatment success for individuals living with vitiligo, as endorsed by most individuals living with vitiligo (over 6 months or 12 months of treatment) and expert clinicians. Additionally, results suggest that a minimum 50% improvement from baseline on the T-VASI can be considered a meaningful treatment success for individuals living with non-segmental vitiligo; similarly, half of the expert clinicians also endorsed 50% improvement from baseline as a treatment success.
These findings should be considered in the context of current treatment options in vitiligo; expert clinicians discussed what could be achieved with existing narrowband UVB and topical treatments, and suggested that newer, systemic treatments should achieve that same threshold at a minimum. As treatments become more efficacious, the perception and expectation of what is successful and meaningful may also change. Therefore, the VASI success thresholds proposed from this study are not definitive or fixed; instead, the thresholds reflect current perspectives on vitiligo treatment options and a potential future oral, systemic treatment.
Strengths of this study include the involvement of a multi-disciplinary team including clinical experts, COA, and qualitative research experts, and a patient advocate who actively and collaboratively sought to remain patient-centric, inform knowledge gaps, and mitigate potential researcher bias. It is also a strength that qualitative interview methods were utilized to provide insights into the level of change that is truly important and meaningful for the target population in clinical trials [14] and for dermatologist experts in the treatment of vitiligo. Conceptual saturation, defined as the point at which no new concept-relevant information is identified, was achieved, suggesting that an adequate sample of individuals living with vitiligo (N = 60) were included in the study. Furthermore, quota sampling was utilized to ensure representation of key characteristics within the sample (e.g., FSTs, education level, gender). On the basis of these considerations, the sample size is aligned with industry recommendations [18, 19].
Methodological limitations are also noted. The eligibility criteria required at least 0.25% BSA on the face, and all adults and almost all adolescents met this criterion. This may have skewed the body areas ranked as most bothersome, although the findings were aligned with previous research that identified the face and hands as important areas for achieving satisfactory treatment [13]. Demographically, 58% of the sample were white or Caucasian. However, patients in all six FST groups were represented; no FST group was considered to be over- or under-represented, with each ranging between 10% and 23% of the total sample. Additionally, no substantial differences were noted between FST groups. Future research may build upon this study further, and confirm that the meaningful change thresholds identified are generalizable to individuals with vitiligo. However, Ezzedine et al. [20] reports cross-cultural validation of a short-form of the vitiligo impact patient scale (VIPs) for light skin types (FSTs I–III) and for dark skin types (FSTs IV–VI). Furthermore, several studies have observed that individuals of all FSTs with vitiligo experience psychosocial burden [21, 22].
Interview activities relating to the VASI scoring were complex, particularly on the T-VASI where “before-and-after” treatment images were not available. To address this, interviewers spent time explaining each activity in patient-friendly language and allowed participants time to absorb the information. Interviewers challenged any obvious discrepancies in interpretation to seek consistent participant comprehension. While it cannot be guaranteed that all participants understood the complexities of the F-VASI and T-VASI scoring, based on interviewer feedback, patients demonstrated sufficient understanding to meaningfully participate in each activity. Therefore, all data were retained in the analyses. The images representing percentage changes in VASI scores were simple in design (Fig. 3), and the location of the “lesion” remained fixed to allow patients to consider the percentage itself, not the location of the vitiligo. Additionally, owing to time constraints, not all participants discussed each percentage change. A conservative approach was taken to provide exact counts in the results. However, it can be inferred that those patients who think 75% improvement is successful would also consider a 90% improvement is successful.
This study was conducted within a US sample. While first- or second-generation participants living in the USA from the Middle East, Asia, or Africa (Table 1; ~ 13% of total sample) were included, these findings would need to be confirmed in other countries and cultures. In addition, various subcultures within the USA need to be identified and queried to explore differences.
This study qualitatively incorporated patients’ and clinicians’ perspectives to explore a threshold for defining within-patient meaningful change. FDA PFDD Draft Guidance [16] notes that interviews can be complementary to anchor-based methods to inform responder definitions in clinical trials. A next step is to confirm these thresholds quantitatively through anchor-based analyses using appropriate anchor item(s). These thresholds may eventually be useful in clinical practice.
Conclusions
Repigmentation is an outcome of priority for individuals living with vitiligo. The VASI was considered an appropriate tool to assess the extent of vitiligo in clinical trials for vitiligo treatments. A minimum 75% improvement from baseline in the F-VASI and minimum 50% improvement from baseline in the T-VASI were identified as within-patient clinically meaningful thresholds endorsed by individuals living with vitiligo.
References
Ezzedine K, Eleftheriadou V, Whitton M, van Geel N. Vitiligo. Lancet. 2015;386(9988):74–84.
Speeckaert R, van Geel N. Distribution patterns in generalized vitiligo. J Eur Acad Dermatol Venereol. 2014;28(6):755–62.
Hamzavi I, Jain H, McLean D, Shapiro J, Zeng H, Lui H. Parametric modeling of narrowband UV-B phototherapy for vitiligo using a novel quantitative tool: the Vitiligo Area Scoring Index. Arch Dermatol. 2004;140(6):677–83.
Rosmarin D, Pandya AG, Lebwohl M, Grimes P, Hamzavi I, Gottlieb AB, et al. Ruxolitinib cream for treatment of vitiligo: a randomised, controlled, phase 2 trial. Lancet. 2020;396(10244):110–20.
Komen L, Da Graça V, Wolkerstorfer A, De Rie M, Terwee C, van der Veen J. Vitiligo Area Scoring Index and Vitiligo European Task Force assessment: reliable and responsive instruments to measure the degree of depigmentation in vitiligo. Br J Dermatol. 2015;172(2):437–43.
Bae JM, Zubair R, Ju HJ, Kohli I, Lee HN, Eun SH, et al. Development and validation of the fingertip unit for Assessing Facial Vitiligo Area Scoring Index (F-VASI). J Am Acad Dermatol. 2021.
US Food and Drug Administration. Guidance for industry patient-reported outcome measures: use in medical product development to support labeling claims. 2009. https://www.fda.gov/media/77832/download. Accessed 18 Aug 2021.
US Food and Drug Administration. Patient-focused drug development: collecting comprehensive and representative input. 2020. https://www.fda.gov/media/139088/download. Accessed 18 Aug 2021.
Powers JH III, Patrick DL, Walton MK, Marquis P, Cano S, Hobart J, et al. Clinician-reported outcome assessments of treatment benefit: report of the ISPOR clinical outcome assessment emerging good practices task force. Value Health. 2017;20(1):2–14.
Walton MK, Powers JH III, Hobart J, Patrick D, Marquis P, Vamvakas S, et al. Clinical outcome assessments: conceptual foundation—report of the ISPOR clinical outcomes assessment–emerging good practices for outcomes research task force. Value Health. 2015;18(6):741–52.
U.S. Food and Drug Administration. Public meeting on patient-focused drug development for Vitiligo: transcript. 2021. https://www.fda.gov/media/146995/download. Accessed 22 Oct 2021.
Gan EY, Eleftheriadou V, Esmat S, Hamzavi I, Passeron T, Böhm M, et al. Repigmentation in vitiligo: position paper of the Vitiligo Global Issues Consensus Conference. Pigment Cell Melanoma Res. 2017;30(1):28–40.
Eleftheriadou V, Hamzavi I, Pandya A, Grimes P, Harris J, Huggins R, et al. International Initiative for Outcomes (INFO) for vitiligo: workshops with patients with vitiligo on repigmentation. Br J Dermatol. 2019;180(3):574–9.
Staunton H, Willgoss T, Nelsen L, Burbridge C, Sully K, Rofail D, et al. An overview of using qualitative techniques to explore and define estimates of clinically important change on clinical outcome assessments. J Patient Rep Outcomes. 2019;3(1):1–10.
Kitchen HGK, Johnson C, Wyrwich KW, Lukic T, Al-Zubeidi T, Marshall C, Pegram H, King S, King B. A qualitative study to explore the content validity of the Vitiligo Patient Priority Outcome (ViPPO) measures. In: Vitiligo international symposium 2021. 2021.
US Food and Drug Administration. Patient-focused drug development: methods to identify what is important to patients (draft guidance). 2019. https://www.fda.gov/media/131230/download. Accessed 18 Aug 2021.
Patrick DL, Burke LB, Gwaltney CJ, Leidy NK, Martin ML, Molsen E, et al. Content validity—establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO good research practices task force report: part 1—eliciting concepts for a new PRO instrument. Value Health. 2011;14(8):967–77.
Turner-Bowker DM, Lamoureux RE, Stokes J, Litcher-Kelly L, Galipeau N, Yaworsky A, et al. Informing a priori sample size estimation in qualitative concept elicitation interview studies for clinical outcome assessment instrument development. Value Health. 2018;21(7):839–42.
Patrick DL, Burke LB, Gwaltney CJ, Leidy NK, Martin ML, Molsen E, et al. Content validity—establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO Good Research Practices Task Force report: part 2—assessing respondent understanding. Value Health. 2011;14(8):978–88.
Ezzedine K, Ahmed M, Tovar-Garza A, Hajj C, Whitton M, Pandya A, et al. Cross-cultural validation of a short-form of the Vitiligo Impact Patient scale (VIPs). J Am Acad Dermatol. 2019;81(5):1107–14.
Ezzedine K, Sheth V, Rodrigues M, Eleftheriadou V, Harris JE, Hamzavi IH, et al. Vitiligo is not a cosmetic disease. J Am Acad Dermatol. 2015;73(5):883–5.
Grimes PE, Miller MM. Vitiligo: patient stories, self-esteem, and the psychological burden of disease. Int J Women’s Dermatol. 2018;4(1):32–7.
Acknowledgements
The authors thank and acknowledge the individuals living with vitiligo and expert clinicians who participated in this interview study.
Funding
This study was developed under a research contract between Clarivate (formerly DRG Abacus) and Pfizer. This study was sponsored by Pfizer, who are funding the journal’s Rapid Service Fees.
Author Contributions
HK, KWW, CC, TL, TA, CM and HP conceptualized and designed this study and approved the final protocol. CC, HK, TA, CM and HP conducted interviews and collected/analysed the study data. LSD, IHH and BK provided expert review throughout the conduct of the study. All authors interpreted the data, and reviewed/approved this manuscript.
Disclosures
Helen Kitchen, Chloe Carmichael, Tamara Al-zubeidi and Chris Marshall are employees and stockholders of Clarivate, a health economic and outcomes research consultancy. Kathleen Wyrwich is a former Pfizer Inc. employee, and holds Pfizer stock and stock options, and Eli Lilly and Company stock. She is currently employed at Bristol Myers Squibb Company. Linda Deal and Tatjana Lukic are salaried employees and hold stock shares and/or options in Pfizer Inc. Hannah Pegram was an employee of Clarivate at the time this work was conducted. Iltefat Hamzavi has served on advisory boards and/or is a consultant and/or is a clinical trial investigator for Abbvie, Pfizer Inc., Bayer, Lenicura, Incyte, UCB, Boehringer Ingelheim, Estee Lauder, Ferndale Laboratories, Galderma Laboratories, L.P., Loreal, Unigen Inc., Arcutis, Avita, Novartis and Janssen. He is a board member of the Global Vitiligo Foundation. Brett King has served on advisory boards and/or is a consultant and/or is a clinical trial investigator for Abbvie, AltruBio Inc, Almirall, AnaptysBio, Arena Pharmaceuticals, Bioniz Therapeutics, Bristol-Meyers Squibb, Concert Pharmaceuticals Inc, Equillium, Horizon Therapeutics, Eli Lilly and Company, Incyte Corp, Janssen Pharmaceuticals, LEO Pharma, Otsuka/Visterra Inc., Pfizer Inc., Regeneron, Sanofi Genzyme, TWi Biotechnology Inc., and Viela Bio. He is on speaker bureaus for Abbvie, Incyte Corp, LEO Pharma, Pfizer Inc., Regeneron and Sanofi Genzyme.
Compliance with Ethics Guidelines
The study protocol was reviewed and approved by WIRB-Copernicus Group® independent review board (WCG-IRB) on 20th October 2020. Written and verbal informed consent was obtained from every participant before each interview was conducted and before any other study activities.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request, and with permission from the study sponsor.
Author information
Authors and Affiliations
Corresponding author
Additional information
Kathleen W. Wyrwich and Hannah Pegram Affiliation when this study was conducted.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kitchen, H., Wyrwich, K.W., Carmichael, C. et al. Meaningful Changes in What Matters to Individuals with Vitiligo: Content Validity and Meaningful Change Thresholds of the Vitiligo Area Scoring Index (VASI). Dermatol Ther (Heidelb) 12, 1623–1637 (2022). https://doi.org/10.1007/s13555-022-00752-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00752-8