Abstract
Introduction
Since the 2012 Multinational Assessment of Psoriasis and Psoriatic Arthritis (MAPP) survey, several systemic treatments for psoriasis (PsO) and/or psoriatic arthritis (PsA) have been approved. The population-based UPLIFT survey was conducted to understand how perceptions of treatment-related outcomes have evolved, particularly for patients with mild to moderate PsO and/or PsA and their dermatologists.
Methods
This population- and web-based survey was conducted from 2 March to 3 June 2020, in North America, Europe, and Japan. Adults with self-reported healthcare practitioner (HCP)-diagnosed PsO and/or PsA and dermatologists who spent > 50% of time treating patients and treated ≥ 20 patients with PsO, including plaque PsO, per month were included. Patient participants were recruited at random from online panels; dermatologists were recruited randomly from representative physician panels.
Results
Of 264,054 patient responses, 3806 who self-reported an HCP diagnosis of PsO and/or PsA were included in the final sample; 67% had PsO alone, 28% had PsO and PsA, and 5% had PsA alone. The estimated population prevalence of psoriatic disease was 7% (PsO only: 4%; PsO and PsA: 2%; PsA only: 1%). Most patients (78%) reported PsO-involved body surface area (BSA) ≤ 3 palms, and ~ 90% or more reported itching, redness, flaking, and scales. Many PsO patients without diagnosed PsA reported musculoskeletal symptoms suggestive of PsA (63%). Across BSA categories, approximately one in four patients was not currently receiving treatment and > 50% had Dermatology Life Quality Index score > 5. Patients and dermatologists had different perceptions of PsO severity, office visit discussions, treatment goals, and treatment satisfaction. The survey was conducted during the coronavirus disease 2019 (COVID-19) pandemic, which could have affected assessments of patient-reported outcomes and ability to have in-person HCP visits.
Conclusions
Patients with PsO and PsA in UPLIFT reported high disease burden, including patients with limited skin involvement. An opportunity exists to align patient and dermatologist perceptions to optimize management of PsO and PsA.
Infographic

Digital feature
This article is published with digital features, including an infographic, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.17104586.
Plain Language Summary
In recent years, several new treatments for psoriasis and psoriatic arthritis have become available. The UPLIFT survey was conducted to understand how viewpoints on psoriatic disease outcomes have changed, especially for patients whose disease is mild or moderate. UPLIFT was a large, online, population-based survey conducted in North America, Europe, and Japan. Adults with psoriasis and/or psoriatic arthritis and dermatologists who treated at least 20 patients with psoriasis per month were included. There were 3806 patients who participated; of these, most had psoriasis and few had psoriatic arthritis. Most patients (78%) with mild to moderate psoriasis had a limited area of skin affected by psoriasis. Psoriasis symptoms were common and included itching, redness, flaking, and scales. Many patients without a diagnosis of psoriatic arthritis reported symptoms that could be related to this disease (such as joint discomfort). Although many patients had psoriasis symptoms, approximately one in four was not currently receiving treatment and more than half reported psoriasis impacted their quality of life. Patients and dermatologists had different perceptions of psoriasis severity, office visit discussions, treatment goals, and treatment satisfaction. There is an opportunity to improve treatment of psoriasis and psoriatic arthritis and to better align patient and physician perceptions of psoriasis. This survey was conducted during the COVID-19 pandemic, which could have partially affected some assessments and the ability to have in-person doctor visits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The impact of new systemic treatments for psoriasis and psoriatic arthritis on perceptions of psoriasis and its treatment is not fully understood. |
The Understanding Psoriatic Disease Leveraging Insights for Treatment (UPLIFT) survey aimed to understand how patient perceptions of treatment-related outcomes have evolved since the 2012 Multinational Assessment of Psoriasis and Psoriatic Arthritis (MAPP) survey, particularly for patients with mild to moderate psoriasis and/or psoriatic arthritis. |
The UPLIFT survey found persistent unmet needs and differences in perceptions of disease severity and treatment satisfaction between patients and physicians. |
There are opportunities to include special area involvement in assessments of disease severity, to enhance relationships between patients and dermatologists, and to improve outcomes in patients with psoriasis across the disease severity continuum. |
Introduction
In 2012, the Multinational Assessment of Psoriasis and Psoriatic Arthritis (MAPP) survey was conducted to characterize the burden of psoriasis (PsO) and psoriatic arthritis (PsA), as well as patient and physician perceptions, and to identify unmet treatment needs [1, 2]. The MAPP survey provided valuable patient-reported findings demonstrating a profound impact of psoriatic disease on quality of life (QOL), high symptom burden, and undertreatment in patients with PsO and/or PsA [1, 2]. Since the MAPP survey was conducted [1], new systemic treatments have been approved with an efficacy permitting clear skin and nearly clear skin in the majority of patients [3,4,5,6], and patient perceptions of treatment-related outcomes may have changed [7, 8]. These treatments represent different mechanisms of action and provide physicians and patients with options to effectively manage psoriatic disease to the extent that treatment targets in guidelines have been upgraded to clear and nearly clear skin [7,8,9,10]. Furthermore, the perception that PsO should be regarded as a systemic disease has expanded under dermatologists [11]. To better understand how patient perceptions of treatment-related outcomes have evolved since the 2012 MAPP survey, particularly for patients with mild to moderate PsO and/or PsA, the Understanding Psoriatic Disease Leveraging Insights for Treatment (UPLIFT) survey was designed based on insights from MAPP and administered to patients and physicians.
Despite the efficacy of available treatments, research suggests that a high burden of disease persists, particularly among patients with bothersome PsO symptoms such as itch, involvement in special areas, or musculoskeletal symptoms [1, 2, 12]. These disease manifestations can result in substantial QOL impairment even in patients who have limited skin involvement [1, 12]. The MAPP survey also highlighted the disconnect between patient and dermatologist perceptions of psoriatic disease severity, indicating that traditional measures of disease severity used by physicians do not fully capture the impact of PsO on patients’ lives and mental health [1, 2, 13, 14]. These different perceptions may explain why some patients with PsO who may benefit from systemic treatment remain on topical therapies [1]. However, topical therapies can be ineffective, inconvenient, or difficult to apply, particularly for patients with PsO in special areas, and do not address the systemic nature of the disease in many patients [15]. Also, joint involvement is often unrecognized in patients with PsO, and patients with mild to moderate PsA may require systemic treatment [1, 16].
When defining disease severity and selecting treatment, current guidelines and international expert consensus recommend considering symptoms and involvement of areas associated with high disease burden, response to topical treatment, and impact of psoriatic disease on QOL in addition to objective measures of disease severity [7, 9, 17, 18]. Because current treatment goals may be more ambitious than they were when MAPP was conducted, it is important to evaluate how the treatment landscape has changed for patients with psoriatic disease.
Data from UPLIFT provide an updated account of the status of the psoriasis field for patients and dermatologists. We present key patient-reported data from UPLIFT, with particular focus on PsO disease burden and current treatments. We also describe patient and dermatologist perceptions of factors contributing to disease severity and treatment expectations.
Methods
Survey Design
The methodology and design of the UPLIFT survey were developed with input from a steering committee consisting of international experts in dermatology and rheumatology. The survey was conducted by AplusA Bell Falla between 2 March 2020 and 3 June 2020. AplusA is a member of major national professional organizations (notably Intellus, ESOMAR, and EphMRA) and adheres to the international code of marketing and social research practice. The protocol was submitted for approval to a central institutional review board (Advarra) in the USA to comply with human subject research requirements. The central institutional review board approval included oversight of all survey activities, as well as the conduct of the survey within Canada, France, Germany, Italy, Japan, Spain, the UK, and the USA. The survey was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki. Survey conduct was consistent with good clinical practices and applicable laws and regulations. Informed consent was obtained prior to survey procedures.
UPLIFT was a cross-sectional, quantitative web-based survey conducted in Canada, France, Germany, Italy, Japan, Spain, the UK, and the USA and administered in the respective local language(s). Completing the survey required ~ 25 min for the patient survey and ~ 30 min for the physician survey. Pretests were conducted before the survey to assess the clarity, understanding, and interpretation of questions and to determine the ease of use and participant experience, including interview length.
Patients were recruited at random from the general population of an online panel of adults, and the sample was balanced for representative populations by region. Panel sources included loyalty panels (e.g., travel, entertainment, media, and retail recruitment programs); organic, open enrollment, and partnership recruitment (including websites, social media influencers, and mobile apps); and affiliate network recruitment (including school and community websites). Patient recruitment was stratified to general population demographics based on sex, age, and region for the respective countries. In the USA, participants who were panelists in the National Psoriasis Foundation were not randomly selected and were excluded from analyses of the prevalence of PsO and PsA diagnoses. For the physician survey, dermatologists were recruited using random selection methods in all countries and sourced from representative panels of physicians. Dermatologists were qualified based on a screening questionnaire. The target sample was 3800 patients and 450 dermatologists, with individual quotas for each country. The number of survey participants was selected as a convenience sample based on participant accessibility by the patient and healthcare provider (HCP) panels. No particular variable was considered to be the most important for the descriptive summary in the primary objective. Subsequently, the anticipated enrollment rate was a factor in determining the final sample size.
Eligibility Criteria
Adults (age ≥ 18 years) with a self-reported HCP diagnosis of PsO and/or PsA were eligible to participate in the patient survey. The physician survey included dermatologists who reported they spend ≥ 50% of their professional time directly treating patients and ≥ 50% of office visits specifically on medical dermatology, and who see ≥ 20 patients with PsO in a typical month, including adults with plaque PsO.
Assessments
Custom and validated patient assessments were conducted, including respondent demographics and clinical characteristics, presence of PsO in all areas and in areas of high disease burden (i.e., genital, nail, scalp, palms, and soles), musculoskeletal/PsA symptoms, Psoriasis Epidemiology Screening Tool (PEST) scores, self-reported skin involvement by PsO-involved BSA (assessed by number of palms based on the palm of the hand including fingers), self-rated current disease severity [1–3 (mild), 4–6 (moderate), 7–10 (severe)], Health Assessment Questionnaire-Disability Index (HAQ-DI) item 8 (HAQ-8), Dermatology Life Quality Index (DLQI), Patient Health Questionnaire-2 (PHQ-2), patient satisfaction with PsO treatment options, and current treatment. Physician responses included dermatologists’ satisfaction with PsO treatment options and their perceptions of patient satisfaction with PsO treatment options. Patient and dermatologist alignment on determinants of disease severity, treatment priorities, and treatment goals was assessed; respondents were asked to rank their top three contributing factors for each metric.
Analyses
Survey results for the patient and dermatologist survey responses were summarized descriptively. Data for patient-rated current disease severity, current treatment, and DLQI were analyzed by level of BSA skin involvement (≤ 3 palms, 4–10 palms, or > 10 palms). An analysis of patients with limited skin involvement (BSA ≤ 3 palms) and PsO in at least one special area (i.e., scalp, nails, palms and/or soles, face, and genitals) evaluated patient-rated current disease severity, current treatment, and DLQI score. Data were summarized using descriptive statistics without data imputation using SAS Enterprise Guide 7.15 HF9 software (SAS, Cary, NC).
Results
Prevalence of PsO and PsA
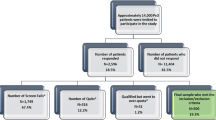
Of 264,054 responses (i.e., participants who clicked on the survey link), 227,637 answered the diagnostic screening question (i.e., “Have you ever been diagnosed by a doctor, or other healthcare practitioner, to have any of these conditions?”) for PsO and PsA; 3806 patient respondents who self-reported an HCP diagnosis of PsO and/or PsA and met inclusion criteria were included in the final sample. Reasons for exclusion included incomplete screening questionnaire, not meeting the survey criteria, incomplete interview response, and responses received after the survey was closed. The number of patients who completed the survey in each country is provided in Table 1.
Most patients responding to the survey had PsO without PsA (67%), 28% had PsO and PsA, and 5% had PsA without PsO. Overall, the population prevalence of psoriatic disease was estimated to be 7%, including 4% of patients with PsO only, 2% with PsO and PsA, and 1% with PsA only (Table 1). The estimated population prevalence of PsO and/or PsA was highest in Italy (11%) and lowest in Japan (2%) (Table 1).
Patient Demographics and Dermatologist Practice Characteristics
Mean patient age was 45.1 years, and approximately half of patients were men (Table 2). The most reported comorbidities were hypertension, depression, and arthritis (patient-reported, HCP-diagnosed osteoarthritis or rheumatoid arthritis; Table 2).
Among the 473 dermatologists who completed the survey, 51% practiced in a hospital-based setting and 49% practiced in a community- or office-based setting. Dermatologists reported that they spent most of their time (91%) treating patients. They treated an average of 501 patients per month in their practices (mean with PsO: n = 71; mean with PsO and PsA: n = 31), and 78% of their patients with PsO had plaque PsO.
Patient-Rated Disease Characteristics
The majority of patients with PsO and/or PsA currently experiencing PsO symptoms reported BSA ≤ 3 palms (78%, n = 3200; Fig. 1). Among patients with BSA ≤ 3 palms, 58% rated their current PsO symptoms as moderate or severe (Fig. 1). Patients commonly reported PsO involvement in special areas, and more than half of patients had scalp involvement (Table 2). Most patients reported PsO symptoms; itching, redness, flaking, and scales occurred in ~ 90% of patients or more (Table 2).
Severity of current PsO symptoms by self-reported BSA category (assessed by number of palms)a. aIn response to the question: On a scale of 1–10, where “1” is “very mild” and “10” is “very severe,” please tell us… a. How severe is your psoriasis currently? bIn response to the question: Based on the amount of psoriasis that could be covered by the palm of your hand (including fingers), how many palms of psoriasis would you say you currently have? BSA psoriasis-involved body surface area, PsA psoriatic arthritis, PsO psoriasis
Among patients with PsO alone (n = 2550), 58% reported experiencing joint discomfort; of these (n = 1485), 63% had ≤ 4 involved joints (consistent with oligoarthritis). When asked if they have experienced PsA symptoms, many patients with PsO alone reported morning stiffness of the joints (44%), nail involvement (32%), pain and/or swelling of the feet (24%), or “sausage” digits (18%); 33% responded none of the above, and 4% responded not sure. Overall, 42% of patients with PsO alone who had joint discomfort had PEST score ≥ 3, suggesting that referral to a rheumatologist should be considered [19]. Among patients with PsO who experienced joint discomfort (overall: n = 1485; ≤ 4 joints: n = 942; > 4 joints: n = 543), 33% of patients with ≤ 4 affected joints and 57% of patients with > 4 affected joints had PEST score ≥ 3. Patients with PsA and/or PsO (n = 1256) had a mean HAQ-8 score of 0.8.
Patient-Reported Current Treatment
Among patients with PsO or PsO and PsA currently experiencing PsO symptoms (n = 3200), ≥ 50% of patients with BSA > 3 palms were receiving systemic therapy (i.e., oral and/or biologic therapy) compared with 35% of those with ≤ 3 palms; however, substantial proportions of patients were not receiving any treatment or only topical therapy. Across BSA categories, 12% (> 10 palms) to 29% (≤ 3 palms) of patients reported they were not currently receiving any treatment for their PsO (Fig. 2). Across BSA categories, approximately 29% of patients reported using topical prescription therapy only, approximately 20% oral therapy (oral prescription only or oral prescription + topical prescription therapy), 10% biologic therapy (biologic only or biologic + topical prescription therapy), and 11% both oral and biologic therapy (oral prescription + biologic, or topical prescription + oral prescription + biologic) (Fig. 2).
Current PsO treatment by level of BSA involvement (assessed by number of palms) in patients with PsO (alone or with PsA) currently experiencing PsO symptoms. BSA psoriasis-involved body surface area, OTC over the counter, PsA psoriatic arthritis, PsO psoriasis, Rx prescription, Oral + biologic oral Rx + biologic, topical Rx + oral Rx + biologic, biologic biologic only, biologic + topical Rx, oral oral Rx only, oral Rx + topical Rx, topical only topical Rx only, other other only, phototherapy only, phototherapy + other (i.e., anything other than prescription oral/biologic/topical therapy or phototherapy), no Rx treatment no treatment other than oral OTC or topical OTC
Patient-Reported Quality of Life
Overall, in patients with PsO and/or PsA (n = 3614), mean DLQI score was 9.3, and 56% of patients experienced at least a moderate impact on QOL (DLQI score > 5). In patients with PsO involvement in at least one special area (n = 2776), the mean (SD) DLQI total score was 9.9 (8.5) and 57.9% reported DLQI total score > 5. The proportion of patients with at least a moderate effect of PsO on QOL was greater among patients with involvement in at least one special area versus no special area involvement; the proportion of patients with DLQI total score > 5 was highest for patients with face involvement and lowest for patients with scalp involvement (Fig. 3). For each item in the DLQI questionnaire, mean DLQI scores were higher for patients with PsO involvement in at least one special area compared with patients with no special area involvement (Fig. 4). Also, mean DLQI scores for individual questions were generally lowest in patients with scalp PsO and higher for patients with involvement in other special areas, such as the face (Supplementary Fig. 1). Among patients with PsO and/or PsA with limited BSA (≤ 3 palms; n = 2497), 56% had DLQI score > 5; 80% of patients with moderate BSA (4–10 palms) and 88% of patients with large BSA (> 10 palms) had DLQI total score > 5.
Approximately half of patients (52%) with PsO and/or PsA (n = 3806) screened positive for potential major depressive disorder, according to PHQ-2 guidelines (i.e., PHQ-2 score ≥ 3). Patients with DLQI total score > 5 and PsO in at least one special area who also had PHQ-2 score ≥ 3 had higher mean (SD) DLQI total scores [16.8 (6.7); n = 1203] compared with all patients with DLQI total score > 5 and PsO in at least one special area [15.5 (6.85); n = 1607, without positive depression screen].
Analysis of Patients with Limited BSA (BSA ≤ 3 Palms) and Involvement of at Least One Special Area
In UPLIFT, 60% of PsO patients with limited BSA and involvement (BSA ≤ 3 palms) in at least one special area (n = 1927) reported their current disease as moderate or severe. Of these, 51% were receiving topical treatment or no treatment. In this group of patients, mean DLQI score was 9.4, and more than half of patients (56.4%) had a DLQI score > 5.
Patient and Dermatologist Perceptions of Disease Burden and Office Visits
Patients ranked the types of symptoms, duration of PsO, and location of skin lesions as the most important factors defining disease severity (Supplementary Fig. 2). By contrast, dermatologists ranked impact on overall QOL, amount of BSA involvement, and type of symptoms as the top three factors contributing to disease severity (Supplementary Fig. 2); disease duration was ranked tenth, and location of lesions was ranked fourth, for dermatologists. When recalling office visits, considerably more patients than dermatologists reported never discussing joint pain, related conditions, and the impact of PsO on emotional well-being (Supplementary Fig. 3).
Patient and Dermatologist Perceptions of Disease Burden and Treatment Goals and Attributes
For patients, itch reduction was the most important treatment goal, followed by symptom control and skin clearance (Supplementary Fig. 2), whereas dermatologists rated itch reduction as a less important treatment goal and ranked improving QOL as the most important goal (Supplementary Fig. 2). Despite these differences, most patients and dermatologists (> 80%) believed their treatment goals were very closely or somewhat closely aligned. When looking at practice characteristics (e.g., work setting, number of patients per month, percentage of patients with PsO, and disease severity of PsO patients) of dermatologists ranking similar drivers of severity and treatment goals as patients, little difference was observed compared with those dermatologists not ranking factors prioritized by patients.
Patients and dermatologists both considered skin clearance and long-term efficacy to be the most important attributes of an ideal PsO therapy (Supplementary Fig. 2). In addition, dermatologists considered long-term safety to be a top attribute (Supplementary Fig. 2).
Patient and Dermatologist Perceptions of Treatment Satisfaction
Approximately 70% of patients with PsO and/or PsA who had current or prior topical treatment (n = 3129) reported being satisfied with the effectiveness (67%), convenience (71%), and safety (73%) of prescription topical medications for PsO; however, the majority considered topical medications to be burdensome (75%). The most common reasons for the perceived burden of topical treatments included mess (54%), frequency (38%), and duration of application (32%) (Supplementary Fig. 4).
Many patients with PsO and/or PsA who had current or prior oral treatment (n = 2111) reported being satisfied with the effectiveness (66%), convenience (71%), and safety (61%) of prescription oral medications; however, many (66%) considered oral treatments to be burdensome. Top reasons why patients considered oral treatments to be burdensome included side effects (33%), frequency of dosing (32%), and required monitoring of blood levels (29%) (Supplementary Fig. 4). More than half of patients (57%) (n = 1208) had discontinued oral treatment. The most common reasons for discontinuing oral treatments included lack of effectiveness (28%), loss of treatment effectiveness over time (22%), adverse effects on other organs (19%), and lack of tolerability (18%) (Supplementary Fig. 5).
In patients with PsO and/or PsA and current or prior injectable or intravenous treatment (n = 1426), 65% were satisfied with their effectiveness, 60% were satisfied with their convenience, and 58% were satisfied with their safety; however, most patients (84%) reported that these treatments were burdensome. The most common reasons for the perceived burden of injectable or intravenous treatments included fear of adverse events (24%), mental anxiety about preparing for self-injection (24%), and fear of developing immunity or resistance (23%) (Supplementary Fig. 4). A total of 57% of patients (n = 817) had discontinued treatment with an injectable or intravenous medication. The most common reasons for discontinuing injectable or intravenous medications included symptom improvement (19%), concerns regarding long-term safety issues (18%), and needle fatigue (18%) (Supplementary Fig. 5).
The majority of dermatologists (n = 473) reported being somewhat or very satisfied with the short-term (≥ 88%) and long-term effectiveness (≥ 74%), convenience (≥ 79%), tolerability (≥ 88%), and long-term safety (≥ 79%) of current treatment options for PsO. Furthermore, dermatologists (n = 473) perceived that more than half of patients with mild (62%), moderate (59%), and severe (57%) PsO were satisfied with current treatment options.
Overall, 84% of patients (n = 3614) and ≥ 73% of dermatologists (n = 473) reported they believe there is a moderate or strong need for better therapies for PsO, particularly for patients with moderate PsO.
Among patients who reported that topical therapies were “moderately” or “very” burdensome, there was an increased prevalence of PsO involvement in at least one special area, particularly scalp and face involvement, compared with those who reported that topical therapies were “not at all” or “only a little” burdensome (Fig. 5). Greater proportions of patients reporting at least a moderate burden with topical therapies versus lower burden had a positive depression screen [PHQ-2 ≥ 3: 69.3% (786/1134) versus 41.4% (826/1995)], reported polyarthritis [> 4 joints involved: 41.1% (466/1134) versus 29.0% (579/1195)], and had at least a moderate effect of PsO on QOL [DLQI > 5: 76.8% (871/1134) versus 44.8% (893/1995)]. Mean (SD) DLQI total score was higher for patients reporting at least a moderate burden with topical therapies compared with patients reporting lower burden with topical therapies [13.7 (8.8) versus 7.1 (7.2)].
Discussion
The large, multinational UPLIFT survey provided important insights into patient and physician perceptions regarding disease burden and treatment of psoriatic disease. Although new treatments have changed the treatment landscape for PsO and/or PsA since the MAPP survey was conducted in 2012, UPLIFT identified a persistent unmet need for better management of psoriatic disease and several areas in which patient and dermatologist perceptions are not aligned.
Similar to the MAPP survey, two-thirds of patients in UPLIFT had PsO without PsA [1]. However, the estimated population prevalence of PsO and/or PsA in UPLIFT (7%) was higher than that reported in the 2012 MAPP survey (1.9%) [1] and in a recent global metaanalysis (1.1%) [20]. Also, many comorbidities were more prevalent among patients in UPLIFT compared with MAPP, despite patients being younger on average in the UPLIFT versus the MAPP survey [1]. The reasons for these differences in comorbidities are not fully understood but may reflect regional variations or differences in survey methodology. For example, patients recruited for online surveys may be generally younger, more educated, and more likely to have private health insurance than patients recruited for phone surveys such as MAPP [21]; therefore, the UPLIFT population may have been more aware of health conditions and may have been more likely to respond in the affirmative to screening questions for other health conditions. It is also possible that patient awareness of comorbidities and health literacy have increased in the years since the MAPP study was conducted and contributed to differences in comorbidity rates between MAPP and UPLIFT. Despite these differences, common comorbidities in UPLIFT, such as cardiovascular diseases and depression, were similar to comorbidities commonly reported in the Global Burden of Disease Study, a large multinational study that analyzed PsO trends from 1990 to 2017 [22].
Patients in the UPLIFT survey reported relatively high disease burden and unmet need, particularly for a population in which more than three-quarters had limited skin involvement (≤ 3 palms). For example, many patients had PsO involvement in special areas, reported bothersome symptoms such as itching and pain, and perceived their current PsO symptoms as moderate or severe. Moreover, many PsO patients without a PsA diagnosis were exhibiting joint symptoms or had PEST scores warranting referral to a rheumatologist, yet few patients were treated with systemic therapy. Patients in UPLIFT also had mean DLQI scores that indicated at least moderate impairment in QOL, including patients with limited skin involvement. The impact of PsO on QOL was greater among patients with involvement in at least one special area versus those without special area involvement and in patients with a positive depression screen. Considering that greater PsO severity has been associated with increased risk of anxiety or depression, screening for depression using validated assessments may be warranted in patients who demonstrate a high impact of PsO on their QOL [14] with subsequent referral to a mental health professional. In UPLIFT, patients with PsO involvement in any special area had increased QOL burden, which is consistent with prior research showing a relationship between PsO in visible and sensitive special areas and QOL impairment [23]. These findings further support recommendations from current treatment guidelines, which acknowledge the importance of PsO location and QOL when evaluating disease severity in patients with limited skin involvement [7, 9, 24].
Despite the high disease burden and increased number of available treatments, substantial proportions of patients in UPLIFT reported they were not receiving any treatment for their PsO and/or PsA. Although the proportion of patients with PsO in special areas was numerically higher in UPLIFT versus MAPP, the proportion of these patients who were currently receiving treatment was similar in UPLIFT compared with MAPP and compared with the National Psoriasis Foundation Surveys conducted in the USA using data from 2003 to 2011 [25]. Furthermore, in patients who had limited skin involvement and PsO in at least one special area in UPLIFT, more than half rated their disease as moderate or severe and were receiving only topical treatment or no treatment. Findings from UPLIFT highlight an opportunity to initiate systemic treatment earlier in patients who perceive their current disease as moderate or severe regardless of the level of skin involvement, particularly patients with PsO in special areas.
The UPLIFT survey revealed differences between patient and dermatologist perceptions about psoriatic disease burden and treatment options. While patient responses emphasized the impact of specific symptoms of PsO, dermatologists placed greater importance on overall QOL when evaluating disease severity. Furthermore, recall of past office visit discussions differed between patients and dermatologists, highlighting an opportunity to better align patient and physician perceptions of PsO treatment and goals of therapy. These findings are in line with results from the global Harris poll, a web-based survey of patients with PsA, which found that most patients wished for increased communication with their physicians about their disease and treatment goals [26]. Considering that National Psoriasis Foundation (NPF)–American Academy of Dermatology (AAD) guidelines emphasize the importance of the patient–provider relationship in the care of patients with psoriasis [7], results from UPLIFT suggest there is an opportunity to improve communication and patient care.
Many patients also reported a high burden associated with PsO treatments, including lack or loss of effectiveness, tolerability issues, and route-of-administration concerns. Furthermore, some patients had discontinued oral or injectable/intravenous treatments because of lack of access or insurance issues. Reasons for discontinuing PsO medications among patients in UPLIFT were consistent with those reported in the Harris poll among patients with PsA [26]. Also, more than 80% of patients with PsO in UPLIFT believed there was a need for better therapies, which was generally consistent with findings from the Harris poll [26]. Taken together, findings from UPLIFT suggest there is an opportunity to further optimize treatment for many patients with PsO.
For patients reporting that topical therapies were “moderate” or “very” burdensome, results from UPLIFT demonstrated an increased prevalence of special area manifestations, particularly for scalp and face involvement, compared with patients who reported that topical therapies were “not at all” or “only a little” burdensome. This finding suggests there are limitations associated with topical therapies for the treatment of PsO involvement in special areas. In addition, a greater proportion of patients reporting at least a moderate burden with topical therapies displayed symptoms of depression, had polyarthritis, and reported at least a moderate effect of PsO on their QOL compared with patients whose burden associated with topical treatments was lower. Thus, the perceived burden of topical therapies reflects a broader disease burden and highlights the importance of optimizing treatment for patients with PsO. For better access to care for these patients, it is important to recategorize disease severity assessment, including special area involvement.
This survey study had some limitations inherent to survey studies, such as recall bias. Participants were selected from an online panel of adults that may not be fully representative of the general population. The survey did not include nurse practitioners or physician assistants, who often provide care to patients with psoriasis in clinical practice. Also, part of this survey was conducted during the COVID-19 pandemic. The emotional burden associated with COVID-19 may have had an impact on psychological and physiological aspects of living with psoriatic disease and could have affected assessments of patient-reported outcomes. Pandemic restrictions may have limited in-office visits and necessitated reliance on virtual visits, which could have affected patient and physician responses.
Conclusions
The 2020 UPLIFT survey revealed substantial patient burden, treatment dissatisfaction, and potential undertreatment with systemic therapy in PsO, including for patients with limited skin involvement, involvement in special areas, or bothersome symptoms such as itching and pain. Many patients with PsO but without a PsA diagnosis experienced musculoskeletal symptoms and may be candidates for referral to a rheumatologist. Also, QOL impairment was higher in patients with a positive depression screen, suggesting a need for further mental health evaluation. Overall, these findings underscore an opportunity for enhanced patient–dermatologist relationships to improve outcomes and address persistent unmet needs of patients with PsO across the disease severity continuum. Potential topics for future analysis include further exploration of the disconnect between patient and physician perceptions to optimize management of PsO and PsA.
Change history
26 December 2021
A peer-reviewed infographic was retrospectively added to this publication.
06 January 2022
A Correction to this paper has been published: https://doi.org/10.1007/s13555-021-00656-z
References
Lebwohl MG, Bachelez H, Barker J, Girolomoni G, Kavanaugh A, Langley RG, et al. Patient perspectives in the management of psoriasis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis Survey. J Am Acad Dermatol. 2014;70(5):871–81.
van de Kerkhof PCM, Reich K, Kavanaugh A, Bachelez H, Barker J, Girolomoni G, et al. Physician perspectives in the management of psoriasis and psoriatic arthritis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis survey. J Eur Acad Dermatol Venereol. 2015;29(10):2002–10.
Reich K, Armstrong AW, Foley P, Song M, Wasfi Y, Randazzo B, et al. Efficacy and safety of guselkumab, an anti-interleukin-23 monoclonal antibody, compared with adalimumab for the treatment of patients with moderate to severe psoriasis with randomized withdrawal and retreatment: results from the phase III, double-blind, placebo- and active comparator-controlled VOYAGE 2 trial. J Am Acad Dermatol. 2017;76(3):418–31.
Reich K, Pinter A, Lacour JP, Ferrandiz C, Micali G, French LE, et al. Comparison of ixekizumab with ustekinumab in moderate-to-severe psoriasis: 24-week results from IXORA-S, a phase III study. Br J Dermatol. 2017;177(4):1014–23.
Langley RG, Elewski BE, Lebwohl M, Reich K, Griffiths CE, Papp K, et al. Secukinumab in plaque psoriasis - results of two phase 3 trials. N Engl J Med. 2014;371(4):326–38.
Thaci D, Blauvelt A, Reich K, Tsai TF, Vanaclocha F, Kingo K, et al. Secukinumab is superior to ustekinumab in clearing skin of subjects with moderate to severe plaque psoriasis: CLEAR, a randomized controlled trial. J Am Acad Dermatol. 2015;73(3):400–9.
Menter A, Strober BE, Kaplan DH, Kivelevitch D, Prater EF, Stoff B, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics. J Am Acad Dermatol. 2019;80(4):1029–72.
Nast A, Spuls PI, van der Kraaij G, Gisondi P, Paul C, Ormerod AD, et al. European S3-Guideline on the systemic treatment of psoriasis vulgaris—update apremilast and secukinumab—EDF in cooperation with EADV and IPC. J Eur Acad Dermatol Venereol. 2017;31(12):1951–63.
Armstrong AW, Siegel MP, Bagel J, Boh EE, Buell M, Cooper KD, et al. From the Medical Board of the National Psoriasis Foundation: treatment targets for plaque psoriasis. J Am Acad Dermatol. 2017;76(2):290–8.
Puig L, Carrascosa JM, Carretero G, de la Cueva P, Lafuente-Urrez RF, Belinchón I, et al. Spanish evidence-based guidelines on the treatment of psoriasis with biologic agents, 2013. Part 1: on efficacy and choice of treatment. Spanish Psoriasis Group of the Spanish Academy of Dermatology and Venereology. Actas Dermosifiliogr. 2013;104(8):694–709.
Korman NJ. Management of psoriasis as a systemic disease: what is the evidence? Br J Dermatol. 2020;182(4):840–8.
Edson-Heredia E, Zhu B, Guo J, Maeda-Chubachi T, Lebwohl M. Disease burden and quality of life in psoriasis patients with and without comorbid psoriatic arthritis: results from National Psoriasis Foundation panel surveys. Cutis. 2015;95(3):173–8.
Merola JF, Qureshi A, Husni ME. Underdiagnosed and undertreated psoriasis: nuances of treating psoriasis affecting the scalp, face, intertriginous areas, genitals, hands, feet, and nails. Dermatol Ther. 2018;31(3):e12589.
Lamb RC, Matcham F, Turner MA, Rayner L, Simpson A, Hotopf M, et al. Screening for anxiety and depression in people with psoriasis: a cross-sectional study in a tertiary referral setting. Br J Dermatol. 2017;176(4):1028–34.
Blakely K, Gooderham M. Management of scalp psoriasis: current perspectives. Psoriasis (Auckland, NZ). 2016;6:33–40.
Singh JA, Guyatt G, Ogdie A, Gladman DD, Deal C, Deodhar A, et al. 2018 American College of Rheumatology/National Psoriasis Foundation guideline for the treatment of psoriatic arthritis. Arthritis Rheumatol. 2019;71(1):5–32.
Strober B, Ryan C, van de Kerkhof P, van der Walt J, Kimball AB, Barker J, et al. Recategorization of psoriasis severity: Delphi consensus from the International Psoriasis Council. J Am Acad Dermatol. 2020;82(1):117–22.
Amatore F, Villani AP, Tauber M, Viguier M, Guillot B. French guidelines on the use of systemic treatments for moderate-to-severe psoriasis in adults. J Eur Acad Dermatol Venereol. 2019;33(3):464–83.
Ibrahim GH, Buch MH, Lawson C, Waxman R, Helliwell PS. Evaluation of an existing screening tool for psoriatic arthritis in people with psoriasis and the development of a new instrument: the Psoriasis Epidemiology Screening Tool (PEST) questionnaire. Clin Exp Rheumatol. 2009;27(3):469–74.
Parisi R, Iskandar IYK, Kontopantelis E, Augustin M, Griffiths CEM, Ashcroft DM. National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study. BMJ. 2020;369:m1590.
Alcaraz KI, Vereen RN, Burnham D. Use of telephone and digital channels to engage socioeconomically disadvantaged adults in health disparities research within a social service setting: cross-sectional study. J Med Internet Res. 2020;22(4):e16680.
Mehrmal S, Uppal P, Nedley N, Giesey RL, Delost GR. The global, regional, and national burden of psoriasis in 195 countries and territories, 1990 to 2017: a systematic analysis from the Global Burden of Disease Study 2017. J Am Acad Dermatol. 2021;84:46–52.
Augustin M, Sommer R, Kirsten N, Danckworth A, Radtke MA, Reich K, et al. Topology of psoriasis in routine care: results from a high-resolution analysis in 2009 patients. Br J Dermatol. 2019;181(2):358–65.
Elmets CA, Leonardi CL, Davis DMR, Gelfand JM, Lichten J, Mehta NN, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities. J Am Acad Dermatol. 2019;80(4):1073–113.
Armstrong AW, Robertson AD, Wu J, Schupp C, Lebwohl MG. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation surveys, 2003–2011. JAMA Dermatol. 2013;149(10):1180–5.
Lim I, Richette P, Queiro-Silva R, Moser J, Cappelleri JC, Ng HY, et al. Patient perceptions of psoriatic arthritis management and communication with physicians in Australia: results from a patient survey. Rheumatol Ther. 2021;8:761–74.
Acknowledgements
We thank the patients and physicians who participated in the survey.
Funding
This survey and the journal’s Rapid Service Fees were funded by Amgen Inc.
Medical Writing and/or Editorial Assistance
Writing support was funded by Amgen Inc. and provided by Kristin Carlin, BSPharm, MBA, of Peloton Advantage, LLC, an OPEN Health company, and Cathryn M. Carter, MS, employee of and stockholder in Amgen Inc.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Mark Lebwohl, Richard G. Langley, Carle Paul, Lluis Puíg, Kristian Reich, Peter van de Kerkhof, and Paolo Gisondi contributed to the survey conception and design. Material preparation, data collection, and/or analysis were performed by Mark Lebwohl, Richard G. Langley, Carle Paul, Lluis Puíg, Kristian Reich, Peter van de Kerkhof, Hsiuan-Lin Wu, Sven Richter, Shauna Jardon, and Paolo Gisondi. All authors contributed to drafting of the manuscript and approved the final manuscript.
Prior Presentation
Lebwohl M, Langley RG, Paul C, Puíg L, Reich K, van de Kerkhof P, Tang L, Richter S, Guerette B, Gisondi P. Evolution of patient perceptions of psoriatic disease: results from the Understanding Psoriatic Disease Leveraging Insights for Treatment (UPLIFT) survey. Poster presented at: the 2021 Winter Clinical Dermatology Conference-Hawaii® [virtual]; January 16–24, 2021.
Disclosures
Mount Sinai (which receives research funds from AbbVie, Amgen Inc., Arcutis, Avotres, Boehringer Ingelheim, Dermavant Sciences, Eli Lilly, Incyte, Janssen Research & Development, LLC, Ortho Dermatologics, Regeneron, and UCB) – employment; Aditum Bio, Almirall, AltruBio Inc., AnaptysBio, Arcutis, Inc., Arena Pharmaceuticals, Aristea Therapeutics, Arrive Technologies, Avotres Therapeutics, BiomX, Boehringer Ingelheim, Brickell Biotech, Bristol Myers Squibb, Cara Therapeutics, Castle Biosciences, CorEvitas, Dermavant Sciences, Dr. Reddy’s Laboratories, Evelo Biosciences, Evommune, Inc., Facilitation of International Dermatologic Education, Forte Biosciences, Foundation for Research and Education in Dermatology, Helsinn Therapeutics, Hexima Ltd., LEO Pharma, Meiji Seika Pharma, Mindera, Pfizer, Seanergy, and Verrica – consultant. Richard G. Langley: AbbVie, Amgen Inc., Boehringer Ingelheim, Janssen, LEO Pharma, Lilly, Novartis, Pfizer, and UCB—principal investigator, scientific advisory board, or speaker. Carle Paul: AbbVie, Boehringer Ingelheim, Janssen, Lilly, Pfizer, Pierre Fabre, Sanofi, and UCB—research support; AbbVie, Almirall, Amgen, Boehringer Ingelheim, Celgene, Janssen, LEO Pharma, Lilly, Merck, Pierre Fabre, Pfizer, Regeneron, Sanofi, and UCB honoraria/consultant. Lluis Puíg: AbbVie, Amgen Inc., Boehringer Ingelheim, Janssen, LEO Pharma, Lilly, Novartis, Pfizer, Regeneron, Roche, Sanofi, and UCB—fees; AbbVie, Almirall, Amgen Inc., Baxalta, Biogen, Boehringer Ingelheim, Celgene, Gebro, Janssen, LEO Pharma, Lilly, Merck-Serono, MSD, Mylan, Novartis, Pfizer, Regeneron, Roche, Sandoz, Sanofi, and UCB—honoraria and consultant fees; Celgene, Janssen, Lilly, MSD, Novartis, and Pfizer—company-sponsored speakers bureaus. Kristian Reich: AbbVie, Affibody, Almirall, Amgen Inc., Avillion, Biogen, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Centocor, Covagen, Dermira, Forward Pharma, Fresenius Medical Care, Galapagos, GlaxoSmithKline, Janssen-Cilag, Kyowa Kirin, LEO Pharma, Lilly, Medac, Merck Sharp & Dohme, Novartis, Miltenyi Biotec, Ocean Pharma, Pfizer, Regeneron, Samsung Bioepis, Sanofi, Sun Pharma, Takeda, UCB, Valeant, and XenoPort—paid speaker and/or participated in clinical trials. Peter van de Kerkhof: AbbVie, Almirall, Bristol Myers Squibb, Celgene, Dermavant, Eli Lilly, Janssen, LEO Pharma, and Novartis—consultant and/or lecturer. Hsiuan-Lin Wu, Sven Richter, and Shauna Jardon: Amgen Inc.—employment. Paolo Gisondi: AbbVie, Amgen Inc., Janssen, LEO Pharma, Lilly, Novartis, Pfizer, Sanofi, and UCB—consultant and grant/research support.
Compliance with Ethics Guidelines
The protocol was submitted for approval to a central institutional review board (Advarra) in the United States to comply with human subject research requirements. The central institutional review board approval included oversight of all survey activities, as well as the conduct of the survey within Canada, France, Germany, Italy, Japan, Spain, the United Kingdom, and the United States. The survey was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki. Survey conduct was consistent with good clinical practices and applicable laws and regulations. Informed consent was obtained prior to survey procedures.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original online version of this article was revised: Revised version of Supplementary material updated.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lebwohl, M., Langley, R.G., Paul, C. et al. Evolution of Patient Perceptions of Psoriatic Disease: Results from the Understanding Psoriatic Disease Leveraging Insights for Treatment (UPLIFT) Survey. Dermatol Ther (Heidelb) 12, 61–78 (2022). https://doi.org/10.1007/s13555-021-00635-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-021-00635-4