Abstract
Introduction
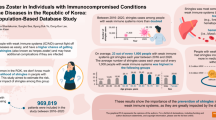
The aim of this study is to describe the disease burden and costs of herpes zoster (HZ) in the general adult Japanese population or patients with immunocompromised (IC) conditions or chronic disorders.
Methods
A retrospective cohort study of individuals aged 18–74 years was conducted using January 2005 to December 2014 records from the Japan Medical Data Center claims database. Twenty-eight IC conditions and chronic disorders were defined by diagnosis codes and/or procedures/treatments. HZ and its related complications were identified. Incidence rates (IR), frequency of HZ-related complications, healthcare resource utilization (HRU), and direct medical costs were estimated. HRU and costs were estimated on a subcohort of HZ cases occurring April 2012–January 2014.
Results
The overall IR of HZ in the total cohort of 2,778,476 adults was 4.92/1000 person-years (PY) [95% confidence interval (CI): 4.86–4.98] and increased with age. The IR in the IC cohort (51,818 subjects) was 8.87/1000 PY (95% CI: 8.29–9.48), ranging from 5.55/1000 PY (95% CI: 4.26–7.09) in psoriasis to 151.68/1000 PY (95% CI: 111.45–201.71) in hematopoietic stem cell transplant recipients; most IRs were in the range 6–10/1000 PY. The IRs in individuals with chronic disorders were also relatively high, in the range 5.40–12.90/1000 PY. The frequency of postherpetic neuralgia was 4.01% (95% CI: 3.72–4.33) in the total cohort and 11.73% (95% CI: 9.01–14.93) in the IC cohort. The mean [standard deviation (SD)] number of outpatient visits was 3.4 (4.9) and 5.0 (5.7), respectively, and the proportion of HZ patients hospitalized was 2.20% and 6.70%, respectively. The mean (SD) direct medical cost per HZ episode was ¥34,664 (¥54,433) and ¥55,201 (¥92,642) in the total and IC cohort, respectively.
Conclusions
The elevated burden of HZ in Japanese individuals harboring IC conditions and chronic disorders documented in our study underlines the need for prevention of HZ in people with these conditions.
Funding
GlaxoSmithKline Biologicals SA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Herpes zoster (HZ) is a viral disease caused by reactivation of varicella-zoster virus (VZV) that remains latent in cranial-nerve or dorsal-root ganglia after previous varicella infection. HZ is characterized by a painful, dermatomal, vesicular rash that in most cases resolves without sequelae within about 1 month [1, 2]. Importantly, approximately 25% of all patients experience HZ-associated complications, the most common of which is postherpetic neuralgia (PHN), persistent pain in the affected area that may last for months or years and severely reduce the patient’s quality of life and ability to perform their usual activities of daily living [3, 4]. Other common HZ complications are ocular, neurological (other than PHN), and disseminated HZ [5, 6].
The cause of reactivation of VZV has not been clearly elucidated, but it is known that effective VZV-specific cell-mediated immunity is necessary to keep VZV in a dormant state [5]. Reactivation may occur at any age, but increasing age is the most important risk factor for HZ, as a result of natural immunosenescence that advances markedly from the age of about 50 years. The proportion of HZ patients developing PHN and other complications also increases with age [5, 7]. Other immunocompromising (IC) conditions, such as malignancies and immunosuppressive medical treatments or interventions often used to treat autoimmune diseases and in organ transplant recipients, may also lead to increased risk of HZ [8,9,10,11,12].
The epidemiology of HZ and its complications is relatively similar around the world (although estimates of the frequency of PHN vary widely due to varying definitions [13]), but the economic burden of the disease varies considerably between countries, depending on factors such as the level of socioeconomic development and types of healthcare available [14].
In Japan, studies have shown an incidence of HZ in the general population aged ≥ 50 [15] or ≥ 60 years [16] of approximately 10 per 1000 person-years (PY), increasing to more than 12/1000 PY in people aged ≥ 80 years. The overall proportion of HZ patients developing PHN was found to be 19.7% in one study, increasing to 32.9% in individuals aged ≥ 80 years [15]. Sato and colleagues found that the odds ratio of PHN development in people on current immunosuppressive treatment compared with no such treatment was 6.44 (p = 0.03) [16].
Similar to health economic studies performed in many other countries (e.g., [17,18,19,20]), the first study of the economic burden of HZ and PHN in Japan found that the associated direct medical costs of these conditions were considerable and mainly caused by multiple outpatient visits and high prescription medication costs [21].
The objective of the present study is to estimate the incidence of HZ and its complications in Japanese adults with a wide range of IC conditions and several chronic disease conditions considered as risk factors for HZ. There is evidence that HZ patients with IC conditions have more frequent HZ-related complications and generate direct medical costs severalfold higher than immunocompetent individuals [22]. To investigate this issue, we also assessed the utilization of healthcare resources and the associated direct medical costs for HZ patients with IC conditions and for the general adult population.
Methods
Study Design and Data Source
This study (GSK study identifier: 204513) was a retrospective, observational cohort study using records from the Japan Medical Data Center claims database (JMDC–CDB). This is a nationwide electronic database of completely anonymized individual records from contracted health insurance associations (payers). Almost 30 million of the Japanese population belong to this type of health insurance association. The registered population includes employees of medium- to large-scale companies aged 74 years or under and their family members. The JMDC-CDB covers approximately 4 million registered individuals (about 3% of the total Japanese population < 75 years of age in 2011).
The medical claims data of JMDC-CDB include patient demographics, diagnosis codes, prescriptions, medical procedures, laboratory tests, and other medical services. Diagnosis codes are recorded as the standardized local codes of diseases defined by the Medical Information System Development Center and the International Classification of Diseases-10 (ICD-10) codes. Prescription medications are recorded by the codes of the standard Anatomic Therapeutic Chemical Classification System (ATC codes).
Study Cohorts
The total cohort consisted of individuals registered in the JMDC-CDB, aged ≥ 18 years at any time between 1 January 2005 and 31 December 2014, with data available for at least 1 year (Fig. 1).
Disposition of participants for the epidemiology or cost analyses. CHC chronic hepatitis, cirrhosis, COPD chronic obstructive pulmonary disease, IHD ischemic heart disease, DM2 type 2 diabetes mellitus, HRU healthcare resource utilization, IC immunocompromised, N number of individuals in the cohort, n number of individuals with specific condition
The study evaluated 16 IC conditions and 12 chronic disease conditions, with the conditions identified by means of ICD-10 codes, procedure codes, and/or ATC codes. The precise definitions of IC conditions and chronic disorders used are summarized with code details and descriptions in the Supplementary Material available online (Tables S1 and S2).
The IC conditions comprised autoimmune thyroiditis (AT), chronic kidney disease accompanied with dialysis or renal transplant as end-stage renal disease (ESRD), congenital immune deficiency (CID), hematological malignancies (HM), hematopoietic stem cell transplant (HSCT), inflammatory bowel disease (IBD), multiple sclerosis (MS), polymyalgia rheumatica (PR), psoriasis (PSOR), rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), solid organ malignancies (SOM), solid organ transplantation (SOT), type 1 diabetes mellitus (DM1), vasculitis (autoimmune) (VAS), and other autoimmune/collagen-connective tissue disease (OAI). Individuals with these conditions comprise the IC cohort. Human immunodeficiency virus or acquired immune deficiency syndrome were not included due to patient privacy concerns.
The chronic disorders comprised asthma (AST), chronic hepatitis, cirrhosis (CHC), chronic obstructive pulmonary disease (COPD), depression (DEP), heart failure (HF), ischemic heart disease (coronary artery disease including angina, cardiac infarction) (IHD), osteoarthritis (OA), osteoporosis (OST_PO), renal failure (RF), stroke (ST), type 2 diabetes mellitus (DM2), and viral hepatitis (VH).
To ensure that follow-up was started at the actual time of diagnosis of an IC or chronic disorder, individuals were only included in an IC or chronic disorder cohort if the date of the first claim related to this IC or chronic disorder occurred at least 12 months (365 days) after the individual’s entry into the JMDC-CDB. Individuals included in one of these cohorts were thus considered as free of that IC or chronic disorder for at least 12 months, and their index date was set to the first date of a claim related to that IC condition or chronic disorder. For individuals with multiple IC/chronic conditions, index date in the total cohort was set to the earliest of index dates. For individuals who were younger than 18 years of age at the date of the first such claim, the index date was set to January 1 of the year they turned 19. Individuals could be included in more than one category of IC condition or chronic disorder.
For all other individuals in the total cohort, the index date was set to 12 months after their date of entry into the database. For individuals younger than 18 years at their date of entry into the database, the index date was set to January 1 of the year they turned 19.
Case Definitions of HZ, PHN, and Other HZ-Related Complications
An HZ episode was defined as individuals reporting at least one medical claim related to HZ (ICD-10 codes B02, B02.0, B02.1, B02.2, B02.3, B02.7, B02.8, and B02.9) associated with a prescription claim for an antiviral drug (such as famciclovir, valaciclovir, aciclovir, or vidarabine) within 1 month of the date of the HZ diagnosis. To exclude patients with herpes simplex, we selected and analyzed only individuals who were prescribed antiviral drugs at the appropriate dosages for HZ according to the Japanese medical package inserts. Table S3 provides details on the definition of HZ events and the appropriate HZ-associated antivirals. The incident HZ was defined as the first recorded HZ episode occurring after index date in the total cohort. HZ episodes prior to index date were not considered. Any HZ episode as defined above occurring more than 2 months after the onset of the first recorded HZ was considered as recurrent HZ and recorded as a separate event.
A case of PHN was identified when an incident HZ case reported at least one medical claim related to HZ (ICD-10 codes as above) between 91 and 365 days after the date of incident HZ and at least one prescription claim for a pain analgesic (including nonsteroidal antiinflammatory drugs, anticonvulsants, tricyclic antidepressants, topical agents, and opioid analgesics) within 1 month of the medical claim. Table S4 presents details on the definition of PHN. As pain analgesics can be prescribed to treat concomitant diseases other than PHN, drug claims for which the same treatment had already been prescribed to the patient during the 6 months preceding the first recorded HZ episode were excluded.
Other HZ-related complications including neurological (other than PHN), ocular, disseminated HZ, and “other” were identified based on standard disease codes and considered as HZ-related complications if they were coded with HZ diagnosis codes (ICD-10 codes as above).
HZ-related complications were assessed up to 12 months after the incident HZ and are reported only for incident HZ cases with at least 12 months of follow-up after HZ onset.
Healthcare Resource Utilization and Cost
The assessment of healthcare resource utilization (HRU) and the calculation of the direct medical costs associated with HZ were limited to HZ episodes occurring between 1 April 2012 and 31 January 2014 with available follow-up in the database for 6 months before and 12 months after the episode (Fig. 1). Each HZ episode was observed up to 12 months after onset or until occurrence of recurrent HZ. The cohorts included in this assessment are referred to as the HRU total cohort and the HRU IC cohort.
The HRU considered included outpatient visits, hospital admissions, laboratory tests, oral prescription medications, injections, topical treatments, and other HZ-related treatments. The duration of HZ-related hospitalizations was determined as follows: (1) hospitalizations with HZ as the causative disease: the entire inpatient period; (2) hospitalizations with a concomitant medical claim with an HZ diagnosis code (ICD-10 codes as above) and antiviral injections or treatment for neurological complications, nerve block, topical treatment, orthopedic treatment, or rehabilitation except for condition (1): hospitalizations under this condition were determined to end the last day any of those treatments was administered; (3) hospitalizations with concomitant medical claims with an HZ diagnosis code (ICD-10 codes as above) but without claims for any of the treatments mentioned under condition (2): not counted as HZ related, and only the HRU related to laboratory tests and pharmacotherapy was included.
The direct medical costs (reported in Japanese Yen, ¥) were calculated based on medical fee points for each procedure, diet, and accommodation fees during hospitalization, and the cost of medications using official drug prices. The medical fee points and drug prices current at the time of HRU were applied. HRU and direct medical cost were calculated for the HRU total cohort and the HRU IC cohort separately. Costs were also calculated according to age group and the type of HZ: uncomplicated HZ, HZ with PHN, HZ with complications other than PHN, and all HZ combined. Cases with both PHN and one or more other complication(s) were classified as HZ with PHN.
A comorbidity score was assessed over the 6 months prior to the HZ episode using the modified Charlson Comorbidity Index based on the algorithm presented by Quan [23, 24].
Statistical Analyses
The incidence rates (IRs) of HZ per 1000 PY with exact 95% confidence interval (CI) were calculated for the total cohort, for the IC cohort overall, and separately for each type of IC condition or chronic disorder. In the total cohort and in the IC cohort, the IR was also calculated stratified by age and gender. For each of these cohorts, the IR was calculated as the total number of incident HZ cases in the cohort divided by the sum of the number of PYs at risk in the cohort. IR and associated CIs are not reported for groups counting fewer than 100 individuals or fewer than 10 incident HZ episodes.
For each individual in an IC or chronic disorder cohort, the period at risk (number of PYs contributed) was defined as lasting from the index date of the IC condition or chronic disorder until the earliest of the following events: first recorded HZ episode, end of follow-up, or study end (31 December 2014). The period at risk in the IC cohort overall was calculated as lasting from the earliest of IC index dates.
For each individual in the total cohort, the period at risk (number of PYs contributed) was calculated as lasting from the index date until the earliest of the following events: first recorded HZ episode, end of follow-up, or study end.
The proportions of HZ cases developing PHN or HZ complications other than PHN were calculated as the percentage of HZ cases that developed PHN or at least one other HZ-related complication, respectively. These proportions were estimated in the total cohort and in the IC cohort.
The frequency of recurrence was calculated as the proportion of HZ cases with at least one recurrent HZ event during the study period.
All statistical analyses were performed using the Statistical Analysis System (SAS 9.2) Drug and Development (SDD) web portal, and Microsoft Excel version 2007 or later.
Compliance with Ethics Guidelines
The study was conducted in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects from The Ministry of Education, Culture, Sports, Science and Technology and the Ministry of Health Labour and Welfare [25], privacy requirements, and the guiding principles of the Declaration of Helsinki. It was approved by the ethics committee of external healthcare providers (the Kitamachi clinic ethics committee, Tokyo).
Results
Study Participants
After eliminating individuals who never reached 18 years of age during the study period, a total of 2,778,476 individuals among the 4,561,815 registered in the JMDC-CDB between 1 January 2005 and 31 December 2014 were enrolled in the study (Fig. 1). Among these, 51,818 (1.86%) individuals entered the IC cohort. The numbers of individuals included in each of the separate IC and chronic disorder cohorts are listed in Table 1.
The mean age (standard deviation, SD) of the total cohort was 37.78 (13.40) years, 45.24% were female, and the mean (SD) follow-up time was 3.20 (2.16) years. The mean (SD) age of the individuals in the total IC cohort was 44.15 (12.64) years, 53.06% were female, and the mean (SD) follow-up period was 4.85 (2.61) years (Table 1). In the last month of the study (Decembeearliest of the followingr 2014), the proportion of subjects from the total cohort included in the total IC cohort was 1.97% (Table S5).
Incidence of HZ
The overall IR of HZ in the total cohort was 4.92/1000 PY (95% CI: 4.86–4.98). A sharp increase in the IR from age 50 years and a steady increase with age in over 50-year-olds was observed for both men and women. Between ages 50 and 65 years, the IR for women was approximately 2 percentage points higher than for men (Table 2). The overall IR for the IC cohort was 8.87/1000 PY (95% CI: 8.29–9.48) (Table 2). IRs in the IC cohort increased from 4.36/1000 PY (95% CI: 3.02–6.10) for the age group 18–29 years to 16.94 (95% CI: 13.57–20.90) for those aged ≥ 65 years. The overall IR for women in the IC cohort was 9.83/1000 PY (95% CI: 8.99–10.71) and for men 7.80/1000 PY (95% CI: 7.02–8.65).
The IRs for the individual IC conditions ranged from 5.55/1000 PY (95% CI: 4.26–7.09) in PSOR to 151.68/1000 PY (95% CI: 111.45–201.71) in HSCT (Table 3). Among the autoimmune diseases, the highest IR was found for SLE, 15.91/1000 PY (95% CI: 8.91–26.25). Among the individuals with chronic disorders, the IRs ranged from 5.40/1000 PY (95% CI: 4.57–6.34) for AST to 12.90/1000 PY (95% CI: 10.83–15.26) for osteoporosis (OST_PO) (Table 3).
Proportion of HZ Patients with PHN and Other Complications
Among the 16,045 HZ cases in the total cohort with at least 12 months of follow-up after HZ onset, 4.01% (95% CI: 3.72–4.33) developed PHN. The proportions with HZ-related complications other than PHN were: neurological, 12.36% (95% CI: 11.85–12.88); ocular, 0.97% (95% CI: 0.82–1.13); disseminated HZ, 0.24% (95% CI: 0.17–0.32); other complications, 17.85% (95% CI: 17.26–18.45). Among the 486 HZ cases in the IC cohort with at least 12 months of follow-up after HZ onset, 11.73% (95% CI: 9.01–14.93) developed PHN. The proportions in this cohort with complications other than PHN were: neurological, 15.84% (95% CI: 12.71–19.40); ocular, 1.03% (95% CI: 0.33–2.38); disseminated 1.03% (95% CI: 0.33–2.38); and other complications, 18.72% (95% CI: 15.35–22.48) (Table S6). There was no association between increasing age and the proportion with PHN, neither in the IC cohort nor in the total cohort (data not shown).
Details on the proportion of HZ patients with at least one episode of recurrent HZ are reported in the Supplementary Materials.
Healthcare Resource Utilization and Cost
The total HRU cohort for the cost analysis included 7111 HZ patients, 224 (3.15 %) of whom had at least one IC condition (Table 4).
Comparing the HRU IC cohort with the HRU total cohort, the main differences in resource utilization were in the mean number of outpatient visits, which was 1.5 times higher for the IC cohort than for the total cohort, and the proportion of patients admitted to hospital, 6.7 % in the IC cohort and 2.3 % in the total cohort. The mean number of in-hospital days was similar across the two cohorts (Table 4). The proportions of patients receiving HZ-related oral prescription medications and topical treatments were approximately the same, whereas the proportion receiving injected drugs, antivirals, neurotropin, vitamins, etc., was about 50 % higher in the HRU IC cohort than in the HRU total cohort. Frequently used medications were antivirals, analgesics, and dermatological topicals.
In both cohorts, the mean number of outpatient visits doubled for patients aged ≥60 years compared with those in the age group 18–49 years, just as the frequency of hospitalizations and the length of hospital stays also increased with age (Table S7). Table 5 describes in detail the mean direct medical cost per resource item according to the patients’ IC status and age group (≤ 49, 50–59, and ≥ 60 years). The overall mean cost per HZ episode in the HRU total cohort was ¥34,664, increasing steadily with age by about 20% from one age group to the next. For the HRU IC cohort, the mean cost was ¥55,201, ranging from ¥45,465 in the age group 50–59 years to ¥81,207 in the age group ≥ 60 years. The relatively high rate of hospitalization for the age group 18–49 years in the HRU IC cohort explains this deviation from the general pattern of costs increasing monotonically with age.
Table 5 also presents the distribution of the cost items according to the type of HZ event and the patients’ IC status. Overall, the mean costs of uncomplicated HZ, HZ with PHN, and HZ with complications other than PHN were ¥26,078, ¥119,330, and ¥60,869, respectively. The relative costs according to HZ category (with or without complications) were similar in the two cohorts, with the costs of HZ with PHN about 4.5 times higher and the costs of HZ with complications other than PHN about two times higher than the costs of uncomplicated HZ.
To summarize the cost analysis, HZ patients with IC conditions contributed 3.2% of all the HZ cases and accounted for 5.0% of the total costs attributable to HZ and related complications.
Discussion
This study showed that the overall incidence of HZ among individuals with the selected IC conditions was almost twice as high as the incidence in the total cohort, with considerable variation among the individual IC conditions. The proportion of HZ patients with PHN was about three times as high in the IC cohort as in the total cohort, whereas other HZ-related complications were equally frequent in the two cohorts. The mean direct medical costs per HZ episode were about 60% higher for HZ patients with IC conditions than for the total cohort. The costs per episode increased with age and were much higher for patients with PHN or other HZ-related complications than for those with uncomplicated HZ.
The IRs estimated in the present study in the total cohort for the age groups ≥ 50 years (Table 2) are in line with the incidence rates of approximately 10 per 1000 PY reported in previous studies of the general Japanese population of older adults [15, 16].
Previous studies of the incidence of HZ in individuals with a wider range of IC conditions include those of Chen et al. [8], Forbes et al. [9], Schroder et al. [11], and Yanni et al. [12]. Across these studies and ours, some consistent patterns emerge, for example that the IR is always highest for individuals with HSCT and that the autoimmune disease with highest risk of HZ is SLE. However, the absolute IRs for each IC condition vary considerably between the studies; for instance, the IR we found for HSCT is almost four times higher than that found in another study [8]. These differences in the estimated IRs for the individual IC conditions may be due to varying case definitions, study designs, and population distributions.
A possible reason why SLE consistently showed higher IRs than other autoimmune diseases in many studies is that SLE-specific autoimmune B cell abnormalities or auto-antibody production may be involved in reactivation of VZV and stimulation of nerve cells, although the mechanism is not fully elucidated. The differences in pathophysiology between SLE and other autoimmune diseases are crucial for understanding the VZV reactivation mechanism [26, 27].
The incidence of HZ in IC conditions or chronic disorders may be impacted by use of immunosuppressive agents. Future examinations of several biologicals used in autoimmune disease therapies may help to understand the biological mechanisms responsible for differences between individuals in the timing and severity of VZV reactivation.
Defining PHN as pain (in the rash area) persisting 3 months after HZ onset without any indication of the pain severity, Takao et al. [15] reported a PHN proportion of 19.7% among Japanese HZ patients aged ≥ 50 years. Another prospective study reported that 12.4% of HZ patients treated with famciclovir sustained zoster-associated pain for 90 days [7]. Here, we defined PHN as HZ diagnosis with prescription of analgesics between 3 months and a year after HZ onset, suggesting persistent pain. This definition partly follows the PHN recognition algorithm developed by Klompas et al. [28], but our more limited version has not been validated and likely missed some cases. Hence, the observed PHN proportions of 4.01% (95% CI: 3.72–4.33) in the total cohort and 11.73% (95% CI: 9.01–14.93) in the IC cohort are probably underestimates.
A recent prospective study estimated the direct medical costs of Japanese HZ patients aged ≥ 60 years [21]. Their findings with regard to the mean number of outpatient visits, proportion of patients hospitalized, duration of hospital stays, and proportion receiving prescriptions for oral medications are very similar to ours. They reported mean costs of ¥35,751, ¥95,836, and ¥67,643 for uncomplicated HZ, HZ with PHN, and HZ with complications other than PHN, respectively. The costs per HZ episode were rather similar to our estimates, and the relative costs according to HZ category were also the same as we observed. The Nakamura study only presented economic evidence for HZ episodes in the general Japanese population, and as far as we know, our study is the first to present results for the selected IC populations.
One strength of the present study is the large sample size, both in the part estimating HZ incidence and in the cost analysis cohort, which allowed us to obtain very precise estimates for most of the studied IC/chronic conditions.
The study has several limitations. First, the clinical conditions defined were not validated clinically or by other means. A second limitation is the obvious underestimation of the total burden of HZ in Japan due to the upper age limit of 74 years. With the well-known age-related increase in HZ incidence and frequency of related complications, which in most studies continue undiminished in individuals aged ≥ 75 years [5, 13], our results clearly document only a part of the burden of HZ in Japan. The incidence rates were estimated based on HZ episodes occurring after the index date, so some of these cases may actually have been HZ recurrences. Another limitation is that there was no comparison group of individuals with no IC condition and no chronic disorder.
A further potential limitation is that the socioeconomic status of individuals covered by these employment-associated health insurance plans may not be representative of the general Japanese population in this age group. However, as far as we are aware, no study to date has documented any socioeconomic gradient in the incidence and severity of HZ. Another aspect related to the criteria for being covered by the health insurance plans is that individuals remaining in employment at advanced age are most likely to be healthier and perhaps at lower risk of developing IC conditions or chronic disorders.
Lastly, the definition of an HZ case required prescription of an antiviral in addition to the ICD code, which means that HZ cases for which no antiviral medication was prescribed were not counted. This could probably lead to an underestimation of the overall HZ incidence and make the study results less representative of HZ cases considered of lower severity at presentation.
Conclusions
This study documented that adult Japanese individuals with selected IC conditions or chronic disorders have higher incidence of HZ and develop PHN more often than the total cohort, whereas other HZ-related complications occurred equally often in the two cohorts. The direct medical costs were also higher for HZ cases in the IC cohort than in the total cohort.
Regardless of the still incomplete understanding of the signaling mechanisms involved between particular IC conditions and VZV-specific cell-mediated immunity, it is very informative for clinicians and healthcare payers to realize that individuals with IC conditions or chronic disorders are at higher risk for HZ and therefore may require special attention for its prevention and care.
References
Cohen JI. Herpes zoster. N Engl J Med. 2013;369:1766–7.
Gershon AA, Gershon MD. Pathogenesis and current approaches to control of varicella-zoster virus infections. Clin Microbiol Rev. 2013;26:728–43.
Drolet M, Brisson M, Schmader KE, et al. The impact of herpes zoster and postherpetic neuralgia on health-related quality of life: a prospective study. CMAJ. 2010;182:1731–6.
Johnson RW, Bouhassira D, Kassianos G, Leplege A, Schmader KE, Weinke T. The impact of herpes zoster and post-herpetic neuralgia on quality-of-life. BMC Med. 2010;8:37.
Gershon AA, Gershon MD, Breuer J, Levin MJ, Oaklander AL, Griffiths PD. Advances in the understanding of the pathogenesis and epidemiology of herpes zoster. J Clin Virol. 2010;48(Suppl 1):S2–7.
Johnson RW. Herpes zoster and postherpetic neuralgia. Expert Rev Vaccines. 2010;9:21–6.
Imafuku S, Nakayama J, Higa K, et al. One-year follow-up of zoster-associated pain in 764 immunocompetent patients with acute herpes zoster treated with famciclovir (FAMILIAR study). J Eur Acad Dermatol Venereol. 2014;28:1716–22.
Chen SY, Suaya JA, Li Q, et al. Incidence of herpes zoster in patients with altered immune function. Infection. 2014;42:325–34.
Forbes HJ, Bhaskaran K, Thomas SL, Smeeth L, Clayton T, Langan SM. Quantification of risk factors for herpes zoster: population based case-control study. BMJ. 2014;348:g2911.
Hata A, Kuniyoshi M, Ohkusa Y. Risk of Herpes zoster in patients with underlying diseases: a retrospective hospital-based cohort study. Infection. 2011;39:537–44.
Schroder C, Enders D, Schink T, Riedel O. Incidence of herpes zoster amongst adults varies by severity of immunosuppression. J Infect. 2017;75:207–15.
Yanni EA, Ferreira G, Guennec M, et al. Burden of herpes zoster in 16 selected immunocompromised populations in England: a cohort study in the Clinical Practice Research Datalink 2000-2012. BMJ Open. 2018;8:e020528.
Kawai K, Gebremeskel BG, Acosta CJ. Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open. 2014;4:e004833.
Panatto D, Bragazzi NL, Rizzitelli E, et al. Evaluation of the economic burden of Herpes Zoster (HZ) infection. Hum Vaccine Immunother. 2015;11:245–62.
Takao Y, Miyazaki Y, Okeda M, et al. Incidences of herpes zoster and postherpetic neuralgia in Japanese adults aged 50 years and older from a community-based prospective cohort study: the SHEZ study. J Epidemiol. 2015;25:617–25.
Sato K, Adachi K, Nakamura H, et al. Burden of herpes zoster and postherpetic neuralgia in Japanese adults 60 years of age or older: results from an observational, prospective, physician practice-based cohort study. J Dermatol. 2017;44:414–22.
Gialloreti LE, Merito M, Pezzotti P, et al. Epidemiology and economic burden of herpes zoster and post-herpetic neuralgia in Italy: a retrospective, population-based study. BMC Infect Dis. 2010;10:230.
Johnson BH, Palmer L, Gatwood J, Lenhart G, Kawai K, Acosta CJ. Healthcare resource utilization and costs associated with herpes zoster in the US. J Med Econ. 2016;19:928–35.
Song H, Lee J, Lee M, et al. Burden of illness, quality of life, and healthcare utilization among patients with herpes zoster in South Korea: a prospective clinical-epidemiological study. Int J Infect Dis. 2014;20:23–30.
Ultsch B, Koster I, Reinhold T, et al. Epidemiology and cost of herpes zoster and postherpetic neuralgia in Germany. Eur J Health Econ. 2013;14:1015–26.
Nakamura H, Mizukami A, Adachi K, et al. Economic burden of herpes zoster and post-herpetic neuralgia in adults 60 years of age or older: results from a prospective, physician practice-based cohort study in Kushiro, Japan. Drugs Real World Outcomes. 2017;4:187–98.
Yawn BP, Itzler RF, Wollan PC, Pellissier JM, Sy LS, Saddier P. Health care utilization and cost burden of herpes zoster in a community population. Mayo Clin Proc. 2009;84:787–94.
Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173:676–82.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
The Ministry of Education, Culture, Sports, Science and Technology and the Ministry of Health Labour and Welfare. “Ethical Guidelines for Medical and Health Research Involving Human Subjects” (Provisional Translation as of March 2015). https://www.mhlw.go.jp/file/06-Seisakujouhou-10600000-Daijinkanboukouseikagakuka/0000080278.pdf. Accessed March 2017.
Chen D, Li H, Xie J, Zhan Z, Liang L, Yang X. Herpes zoster in patients with systemic lupus erythematosus: clinical features, complications and risk factors. Exp Ther Med. 2017;14:6222–8.
White DW, Suzanne Beard R, Barton ES. Immune modulation during latent herpesvirus infection. Immunol Rev. 2012;245:189–208.
Klompas M, Kulldorff M, Vilk Y, Bialek SR, Harpaz R. Herpes zoster and postherpetic neuralgia surveillance using structured electronic data. Mayo Clin Proc. 2011;86:1146–53.
Acknowledgements
The authors thank Mr. Gen Terashima, Ms. Miho Fukuhara, and Mr. Yoshihisa Isobe (JMDC Co. Ltd.) for the data collection and analysis of cost part. The authors acknowledge Ms. Soumeya Pierret and Ms. Sophie Caterina for data management and statistical analysis, both for GSK. Morgane Guennec (Keyrus Biopharma at the time) was involved as study biostatistician until October 2016. We also acknowledge Dr. Emmanuelle Espié (GSK) for critical input during the development of the statistical analysis plan. Josephine Ocran-Appiah (GSK Epidemiologist Global Zoster Project) critically reviewed the manuscript draft. The authors thank Giulia Dormal (GSK Stats team) for reviewing the manuscript and providing part of the results.
Funding
GlaxoSmithKline Biologicals SA was the funding source and was involved in all study activities and overall data management (collection, analysis, and interpretation) of this study (GSK identifier 204513). GlaxoSmithKline Biologicals SA also funded all costs associated with the development and publishing of the present manuscript. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Medical Writing and Editorial Assistance
Niels Neymark of Neymark Scientific Writing SCS provided writing assistance on behalf of GSK. Authors would like to thank Business & Decision Life Sciences platform for editorial assistance and publications coordination, on behalf of GSK; Matthieu Depuydt coordinated publication development and provided editorial support.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Prior Presentation
The data of this manuscript have been presented at the Japan Society for Clinical Immunology (JSCI)—45th Annual Meeting 2017 for the epidemiology endpoints and at the ISPOR-AP (2018) International Society for Pharmacoeconomics and Outcomes Research—8th Asia-Pacific Conference 2018 (ISPOR-AP 2018) for the health economics endpoints.
Disclosures
Shinichi Imafuku has received consulting fees and honoraria from the GSK group of companies. Taizo Matsuki is an employee of the GSK group of companies. Akiko Mizukami is an employee of the GSK group of companies. Yasushi Goto has received consulting fees from GSK group of companies. Sabrina de Souza reports consulting fees to her institution Keyrus Biopharma, from GSK group of companies as a part of her function of Consultant (Biostatistician in Epidemiology) until February 2018. Céline Jégou reports consulting fees to her institution Business & Decision Life Sciences, from GSK group of companies as a part of her function of Statistical Programmer. Véronique Bianco is an employee of the GSK group of companies and holds shares in the GSK group of companies. Dominique Rosillon is an employee of the GSK group of companies and holds shares in the GSK group of companies. Chie Ito is an employee of the Japan Medical Data Center and reports having received study fees from the GSK group of companies for the data collection and their analysis. Desmond Curran is an employee of the GSK group of companies and holds shares in the GSK group of companies. Katsiaryna Holl was an employee of the GSK group of companies until mid-August 2018 and holds shares in the GSK group of companies.
Compliance with Ethics Guidelines
The study was conducted in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects from The Ministry of Education, Culture, Sports, Science and Technology and the Ministry of Health Labour and Welfare [25], privacy requirements, and the guiding principles of the Declaration of Helsinki. It was approved by the ethics committee of external healthcare providers (the Kitamachi clinic ethics committee, Tokyo).
Data Availability
Anonymized individual participant data and study documents can be requested for further research from http://www.clinicalstudydatarequest.com.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced digital features
To view enhanced digital features go to: https://doi.org/10.6084/m9.figshare.7251932.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Imafuku, S., Matsuki, T., Mizukami, A. et al. Burden of Herpes Zoster in the Japanese Population with Immunocompromised/Chronic Disease Conditions: Results from a Cohort Study Claims Database from 2005–2014. Dermatol Ther (Heidelb) 9, 117–133 (2019). https://doi.org/10.1007/s13555-018-0268-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-018-0268-8