Abstract
Thyroid cancer is the most common cancer (90%) of the endocrine system and is responsible for 0.5% of all cancer deaths. The incidence of thyroid cancer is thought to be rapidly and steadily increasing in recent decades. Recent studies have described thyroid cancer as the 4th most common cancer today, up from 14th in the early 1990s. This increase is mainly due to various environmental factors including: radiation, smoking, obesity, pollutants such as pesticides, phthalates, polychlorinated biphenyls, perfluorinated compounds, bromine flame retardants, perchlorates, nitrates and various elements such as metals, non-metals and metalloids. In particular, some metals such as iron, copper, cadmium, lead, vanadium, chromium, manganese and nickel have a positive effect, while others such as zinc and magnesium have a negative correlation with thyroid cancer. Other metals such as molybdenum, tin and cobalt appear to increase the incidence of thyroid cancer in combination, while sodium, mercury, aluminum and silver have no evidence of thyroid carcinogenicity. Of the non-metals, iodine and selenium deficiency are associated with carcinogenic effects on the thyroid, while there is no information on any phosphorus-relative activity. Boron belonging to the metalloids is considered a goitrogenic element and probably increases the incidence of thyroid cancer when it acts in combination with cadmium, molybdenum, taken in small non-toxic doses, for a long time. Finally, air pollution has been studied. It has been found that originating from gaseous waste is associated with an increased incidence of cancer in various anatomical areas, including the thyroid.
Similar content being viewed by others
References
Fiore M, Conti GO, Caltabiano R et al (2019) Role of environmental emerging risk factors in thyroid cancer : a brief review. Int J Environ Res Public Health 16:1183–1192
Dalles K, Kostoglou-Athanasiou I (2007) Thyroid cancer. Archives of Hellenic Medicine 24:250–264
Haugen BR, Alexander EK, Bible KC et al (2016) American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26:1–133
Araque KA, Gubbi S, Klubo-Gwiezdzinska J (2020) Updates on the Management of Thyroid Cancer. Horm Metab Res 52:562–577
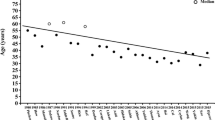
Lim H, Devesa SS, Sosa JA et al (2017) Trends in thyroid cancer incidence and mortality in the United States 1974–2013. JAMA 317:1338–1348
Nickel B, Tan T, Cvejic E, Baade P, McLeod DSA, Pandeya N, Youl P, McCaffery K, Jordan S (2019) Health-Related Quality of Life After Diagnosis and Treatment of Differentiated Thyroid Cancer and Association With Type of Surgical Treatment. JAMA Otolaryngol Head Neck Surg 145:231–238
Pellegriti G, Frasca F, Regalbuto C et al (2013) Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J Cancer Epidemiol 2013:965212
Howlader N, Noone A, Krapcho M et al (2013) SEER Cancer Statistics Review 1975–2010. Bethesda MD: National Cancer Institute. http://seer.cancer.gov/csr/1975_2010
Ferlay J, Colombet M, Soerjomataram I et al (2019) Estimating the global cancer incidence and mortality in 2018: Globocan sources and methods. Int J Cancer 144:1941–1953
Colonna M, Uhry Z, Guizard AV et al (2015) Recent trends in incidence, geographical distribution, and survival of papillary thyroid cancer in France. Cancer Epidemiol 39:511–518
McLeod DSA, Zhang L, Durante C, Cooper DS (2019) Contemporary Debates in Adult Papillary Thyroid Cancer Management. Endocr Rev 40:1481–1499
Aschebrook-Kilfoy B, Dellavalle CT, Purdue M et al (2015) Polybrominated diphenyl ethers and thyroid cancer and risk in the prostate, colorectal, lung, and ovarian cancer screening trial cohort. Am J Epidemiol 181:883–888
Luca E, Fici L, Ronchi A et al (2017) Intake of boron, cadmium, and molybdenum enhances rat thyroid cell transformation. J Exper Clin Cancer Res 36:1–9
Pasha Q, Malik SA, Shah MH (2008) Statistical analysis of trace metals in the plasma of cancer patients versus controls. J Hazard Matr 153:1215–1221
Saenko V, Ivanov V, Tsyb A et al (2011) The Chernobyl accident and its consequences. Clin Oncol (R Coll Radiol) 23:234–243
American Cancer Society. Thyroid cancer detailed guide (2016)- Scharpf J, Tuttle M, Wong R, Ridge D, Smith R, Hartl D, Levine R, Randolph G (2016) Comprehensive management of recurrent thyroid cancer: an American Head and Neck Society consensus statement: AHNS consensus statement. Head Neck 38:1862–1869
Stojsavljevic A, Rovcanin B, Krstic D et al (2019) Evaluation of trace metals in thyroid tissues: comparative analysis with benign and malignant thyroid diseases. Ecotoxicol Environ Saf 183:109479
Furukawa K, Preston D, Funamoto S et al (2013) Long-term trend of thyroid cancer risk among Japanese atomic-bomb survivors: 60 Years after exposure. Int J Cancer 132:1222–1226
UNSCEAR (United Nations, Committee on the Effects of Atomic Radiation) (2000) Sources and effects of ionizing radiation. Report to the General Assembly, with Scientific Annexes. New York, United Nations
Stefan A-I, Piciu A, Mesler A et al (2020) Pediatric thyroid cancer in Europe: an overdiagnosed condition ? A literature review. Diagnostics (Basel) 10:112
Bridget-Sinnott Β, Elaine-Ron Ε, Schneider ΑΒ (2010) Exposing the thyroid to radiation: a review of its current extent, risks, and implications. Endocrinol Rev 31:756–773
Schwertheim S, Theurer S, Jastrow H et al (2019) New insights into intranuclear inclusions in thyroid carcinoma: association with autophagy and with BRAFV600E mutation. PLoS ONE 14:e0226199
Goyal N, Camacho F, Mangano J, Goldenberg D (2015) Evaluating for a geospatial relationship between radon levels and thyroid cancer in Pennsylvania. Laryngoscope 125:E45–E49
Oakland C, Meliker JR (2018) County -level radon and incidence of female thyroid cancer in Iowa, New Jersey, and Wisconsin, USA. Toxics 6:17
CDC (2010) Smoking and tobacco Smoke. Atlanta: CDC http://www.cdc.gov/tobacco/data_statistics/sgr/2010/consumer_booklet/chemicals_smoke/.
Mack WJ, Preston-Martin S, Maso LD et al (2003) A pooled analysis of case-control studies of thyroid cancer: cigarette smoking and consumption of alcohol, coffee, and tea. Cancer Causes Control 14:773–785
Kitahara CM, Platz EA, Beane-Freeman LE et al (2012) Physical activity, diabetes. Cancer Causes Control 23:463–471
Marcello MA, Malandrino P, Almeida JFM et al (2014) The influence of the environment on the development of thyroid tumors: a new appraisal. Endocr Relat Cancer 21:T235–T254
Ericsson UB, Lindgärde F (1991) Effects of cigarette smoking on thyroid function and the prevalence of goitre, thyrotoxicosis and autoimmune thyroiditis. J Inter Med 229:67–71
Franceschi S, Preston-Martin S, Dal Maso L et al (1999) A pooled analysis of case-control studies of thyroid cancer. IV. Benign thyroid diseases. Cancer Causes Control 10:583–595
Aydin LY, Aydin Y, Besir FH et al (2011) Effect of smoking intensity on thyroid volume, thyroid nodularity and thyroid function: The Melen study. Minerva Endocrinol 36:273–280
Malandrino P, Russo M, Ronchi A et al (2016) Increased thyroid cancer incidence in a basaltic volcanic area is associated with non-anthropogenic pollution and biocontamination. Endocrine 53:471–479
Scmidt D, Ricci C, Behrens G, Leitzmann MF (2015) Adiposity and risk of thyroid cancer: a systematic review and meta-analysis. Obes Rev 16:1042–1054
Choi JS, Kim EK, Moon HJ et al (2015) Higher body mass index may be a predictor of extrathyroidal extension in patients with papillary thyroid microcarcinoma. Endocrine 48:264–271
Han MA, Kim JH, Song HS (2019) Persistent organic pollutants, pesticides, and the risk of thyroid cancer: systematic review and meta-analysis. Eur J Cancer Prev 28:344–349
Colao A, Muscogiuri G, Piscitelli P (2016) Environment and health: not only cancer. Int J Environ Res Public Health 13:724
Boas M, Feldt-Rasmussen U, Main KM (2012) Thyroid effects of endocrine disrupting chemicals. Mol Cell Endocrinol 355:240–248
Marotta V, Maladrino P, Russo M et al (2020) Fathoming the link between antropogenic chemical contamination and thyroid cancer. Crit Rev Oncol Hematol 150:102950
Ferrari S-M, Fallahi P, Antonelli A, Benvenvenga S (2017) Environmental issues in thyroid diseases. Front Endocrinol (Lausanne) 8:50
Valizadeh S, Lee SS, Baek K et al (2021) Bioremediation strategies with biochar for polychlorinated biphenyls (PCBs)-contaminated soils: a review. Environ Res 200:111757
Lero CC, Jones RR, Lang H et al (2018) A nested case-control study of polychlorinated biphenyls, organochlorine pesticides, and thyroid cancer in the Janus serum bank cohort. Environ Res 165:125–132
Melzer D, Rice N, Depledge MH, Henley WE, Galloway TS (2010) Association between serum perfluorooctanoic acid (PFOA) and thyroid disease in the U.S. National Health and Nutrition Examination Survey. Environ Health Perspect 118:686–692
Lope V, Perez-Gomez B, Aragones N et al (2009) (2009) Occupational exposure to chemicals and risk of thyroid cancer in Sweden. Int Arch Occup Environ Health 82:267–274
Huang H, Sjodin A, Chen Y et al (2020) Polybrominated diphenyl ethers, polybrominated biphenyls, and risk of papillary thyroid cancer: a nested case-control study. Am J Epidemiol 189:120–132
Nettore IC, Colao A, Macchia PE (2018) Nutritional and environmental factors in thyroid carcinogenesis. Int J Environ Res Public Health 15:1735
NHANES 2001–2002 U.S. Department of Agriculture, Agricultural Research Service (2005) What We Eat In America: usual nutrient intakes from food compared to dietary reference intakes. http://www.ars.usda.gov/ba/bhnrc/fsrg
Yilmaz B, Terekeci H, Sandal S, Kelestimur F (2020) Endocrine disrupting chemicals: exposure, effects on human health, mechanism of action, models for testing and strategies for prevention. Rev Endocr Metab Disord 21:127–147
Ward MH, Jones RR, Brender JD et al (2018) Drinking water nitrate and human health: an updated review. Int J Environ Res Public Health 15:1557
Sebranck JG, Bacus JN (2007) Cured meat products without direct addition of nitrate or nitrite: what are the issues ? Meat Sci 77:136–147
Atakisi E and Merhan O (2017) Nitric Oxide Synthase and Nitric Oxide Involvement in Different Toxicities. Chapter from the book Nitric oxide synthase -Simple enzyme complex roles. http://www.intenchopen.com/books/ Nitric oxide synthase -Simple enzyme complex roles
WHO (2011) Guidelines for drinking water quality, 4th edn. WHO Publications, Geneva
Drozd VM, Branovan I, Shiglik N et al (2018) Thyroid cancer induction: nitrates as independent risk factors or risk modulators after radiation exposure, with a focus on the Chernobyl accident. Eur Thyroid J 7:67–74
Kilfoy BA, Zhang Y, Park Y et al (2011) Dietary nitrate and nitrite and the risk of thyroid cancer in the NIH-AARP diet and health study. Int J Cancer 129:160–172
Sadik NAH, EL-Maraghy, Ismail MF, (2008) Diethylnitrosamine-induced hepatocarcinogenesis in rats: possible chemoprevention by blueberries. Afr J Biochem Res 2:81–87
Merhan O, Ozcan A, Atakisi E et al (2016) The Effect of β-carotene on acute phase response in diethylnitrosamine given rabbits. Kafkas Üniversitesi Veteriner Fakültesi Dergisi 22:533–537
Markaki I, Linos D, Linos A (2003) The influence of dietary patterns on the development of thyroid cancer. Eur J Cancer 39:1912–1919
Liang J, Zhao N, Zhu C et al (2020) Dietary patterns and thyroid cancer risk: a population -based case -control study. Am J Transl Res 12:180–190
Zhang C, Wu H-B, Cheng M-X et al (2019) Association of exposure to multiple metals with papillary thyroid cancer risk in china. Environ Sci Pollut Res Inst 26:20560–20572
Bibi K, Shah MH (2021) Study of essential and toxic metal imbalances in the scalp hair of thyroid cancer patients in comparison with healthy donors. Biol Trace Elem Res 199:500–512
Buha A, Matovic V, Antonijevic B et al (2018) Overview of cadmium thyroid disrupting effects and mechanisms. Int J Mol Sci 19:1501
Zhang Q, Jiang C, Li H et al (2020) Effect of the interaction between cadmium exposure and CLOCK gene polymorphisms on thyroid cancer: a case-control study in China. Biol Trace Elem Res 196:86–95
Chung HK, Nam JS, Ahn CW, Lee YS, Kim KR (2016) Some elements in thyroid tissue are associated with more advanced stage of thyroid cancer in Korean women. Biol Trace Elem Res 171:54–62
Rezaei M, Javadmoosavi S-Y, Mansouri B et al (2019) Thyroid dysfunction: how concentration of toxic and essential elements contribute to risk of hypothyroidism, hyperthyroidism, and thyroid cancer. Environ Sci Pollut Res Int 26:35787–35796
Olmedo P, Pla A, Hernandez AF et al (2013) Determination of toxic elements (mercury, cadmium, lead, tin, and arsenic) in fish and shellfish samples. Risk assessment for the consumers. Environ Int 59:63–72
Leux C, Truong T, Petit C et al (2012) Family history of malignant and benign thyroid diseases and risk of thyroid cancer: a population-based case-control study in New Caledonia. Cancer causes Control 23:745–755
Burger J, Diaz-Bariga F, Marafante E et al (2003) Methodologies to examine the importance of host factors in bioavailability of metals. Ecotoxicol Environ Saf 56:20–31
Badmaev V, Prakash S, Majeed M (1999) Vanadium: a review of its potential role in the fight against diabetes. J Altern Complement Med 5:273–291
Barceloux DG (1999) Vanadium. J Toxicol Clin Toxicol 37:265–278
Mukherjee B, Patra B, Mahapatra S et al (2004) Vanadium—an element of atypical biological significance. Toxicol Lett 150:135–145
Malandrino P, Russo M, Ronchi A et al (2020) Increased thyroid cancer incidence in volcanic areas: a role of increased heavy metals in the environment? Int J Mol Sci 21:3425
Fallahi P, Foddis R, Elia G et al (2018) Vanadium pentoxide induces the secretion of CXCL9 and CX.CL10 chemokines in thyroid cells. Oncol Rep 39:2422–2462
Deng Y, Wang M, Tian T et al (2019) The effect of hexavalent chromium on the incidence and mortality of human cancers: a meta-analysis based on published epidemiological cohort studies. Front Oncol 9:24
Burns CJ, McIntosh LJ, Mink PJ, Jurek AM, Li AA (2013) Pesticide exposure and neurodevelopmental outcomes: review of the epidemiologic and animal studies. J Toxicol Environ Health B Crit Rev 16:127–283
Takir M, Turkoglu O, Turkoglu Z (2017) Thyroid hormone and ultrasonographical analyses in patients with nickel Allergy. EJMO 1:145–148
Mamyrbayev A, Djarkenow T, Dosbayev A et al (2016) The incidence of malignant tumors in environmentally disadvantaged regions of Kazakhstan. Asian Pac J Cancer Prev 17:5203–5209
Baltaci A-K, Dundar T-K, Aksoy F et al (2017) Changes in the serum levels of trace elements before and after the operation in thyroid cancer patients. Biol Trace Elem Res 175:57–64
Qu X, Yang H, Zhifeng Yu et al (2020) Serum zink levels and multiple health outcomes: implications for zink-based biomaterials. Bioact Mater 5:410–422
Saris NEL, Mervaala E, Karppanen H et al (2000) Magnesium: an update on physiological, clinical and analytical aspects. Clin Chim Acta 294:1–26
Anastassopoulou J, Theophanides T (2002) Magnesium-DNA interactions and the possible relation of magnesium to carcinogenesis. Irradiation and free radicals. Crit Rev Oncol Hematol 42:79–91
Castiglioni S, Maier JAM (2011) Magnesium and cancer: a dangerous liaison. Magnes Res 24:S92–S100
Blaszczyk U, Duda-Chodak A (2013) Magnesium: its role in nutrition and carcinogenesis. Rocz Panstw Zakl Hig 64:165–171
Shen F, Cai WS, Li JL, Feng Z, Cao J, Xu B (2015) The Association between serum levels of selenium, copper, and magnesium with thyroid cancer: a meta-analysis. Biol Trace Elem Res 167:225–235
Blunden S, Wallace T (2003) Tin in canned food: a review and understanding of occurrence and effect. Food Chem Toxicol 41:1651–1652
Mol S (2011) Levels of heavy metals in canned bonito, sardines, and mackerel produced in Turkey. Biol Trace Elem 143:974–982
Carcasso I, Benejam I, Benito J et al (2011) Methylmercury levels and bioaccumulation in the aquatic web of a highly mercury-contaminated reservoir. Environ Int 37:1213–1218
IARC monographs on the evaluation of carcinogenic risks to human of beryllium, cadmium, mercury, and exposure in the glass manufacturing industry.58 IARC Lyon, France. http://monographs.iarc.fr/ENG/monographs/58/
Kinjo Y, Akiba S, Yamaguchi N et al (1996) Cancer mortality in Minamata disease patients exposed to methylmercury through fish diet. J Epidemiol 6:134–138
Zidane M, Ren Y, Xhaard C et al (2019) Non-essential trace elements dietary exposure in French Polynesia: intake assessment, nail bio monitoring and thyroid cancer risk. Asian Pac J Cancer Prev 20:355–367
Orihuela D (2011) Aluminum effects on thyroid gland function: iodide uptake, hormone biosynthesis and secretion. J Inorg Biochem 105:1464–1468
Wang W, Liu J, Feng W et al (2019) Targeting mitochondria with Au-Ag. Polydopamine nanoparticles for papillary thyroid cancer therapy. Biomater Sci 7:1052–1063
Ye ZV, Tsyb AF, Vtyurin BM (1995) Trace elements and thyroid cancer. Analyst 120:817–821
Knobel M, Medeiros-Neto G (2007) Relevance of iodine intake as a reputed predisposing factor for thyroid cancer. Arq Bras Endocrinol Metabol 51:701–712
Liu Y, Su L, Xiao H (2017) Review of factors related to the Thyroid Cancer Epidemic. Int J Endocrinol 2017:5308635
Williams ED, Doniach I, Bjarnason O, Michie W (1977) Thyroid cancer in an iodide rich area: a histopathological study. Cancer 39:215–222
Feldt-Rasmussen U (2001) Iodine and cancer. Thyroid 11:483–486
Fuziwara CS, Kimura ET (2014) High iodine blocks a Notch/miR-19 loop activated by the BRAF (V600E) oncoprotein and restores the response to TGFβ in thyroid follicular cells. Thyroid 24:453–462
Kohrle J (2015) Selenium and the thyroid. Curr Opin Endocrinol Diabetes Obes 22:392–401
Filippini T, Michalke B, Wise LA et al (2018) Diet composition and serum levels of selenium species: a cross-sectional study. Food Chem Toxicol 115:482–490
Popova EV, Tinkov AA, Ajsuvakova OP, Skalnaya MG, Skalny AV (2017) Boron—a potential goiterogen? Med Hypotheses 104:63–67
Turner MC, Krewski D, Diver WR et al (2017) Ambient air pollution and cancer mortality in the cancer prevention study II. Environ Health Perspect 125:087013
Cong X (2018) Air pollution from industrial waste gas emission sis associated with cancer incidences in Shanghai, China. Environ Sci Pollut Res 25:13067–13078
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
I. Legakis, A. Barbouni and G. Chrousos declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Legakis, I., Barbouni, A. & Chrousos, G. The importance of toxic environmental substances in the development of thyroid cancer. Toxicol. Environ. Health Sci. 14, 101–109 (2022). https://doi.org/10.1007/s13530-022-00127-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13530-022-00127-8