Abstract
Objective
This retrospective longitudinal study analyzed the demographic profile, insulin usage pattern, and outcomes of insulin-naive adults with type 2 diabetes mellitus (T2DM) who initiated insulin glargine.
Methods
The study included 1006 insulin naive T2DM individuals aged ≥ 18 years, treated with any insulin type between January 2016 and December 2018, using electronic medical records.
Results
Majority of participants were men (55.8%) with a mean age of 59.8 ± 11.9 years and average T2DM duration of 12.0 ± 6.6 years. Insulin glargine was the most commonly used insulin (66.9%), followed by insulin aspart (16.4%), insulin degludec (15.1%), human insulin (11.1%), and insulin isophane (9.2%). At baseline, the mean glycated hemoglobin (HbA1c) was 8.9 ± 1.9%, mean fasting plasma glucose (FPG) was 190 ± 59 mg/dL, and mean post-prandial plasma glucose (PPG) was 264 ± 78 mg/dL. In the insulin glargine group, baseline HbA1c was 9.0 ± 1.7%, FPG was 196 ± 62 mg/dL, and PPG was 283 ± 81 mg/dL. Throughout the study, there was an improvement in HbA1c, FPG, and PPG levels in the insulin glargine group. Body weight remained relatively stable, and the number of hypoglycemic events was minimal and non-life-threatening.
Conclusion
The REALITY study in India demonstrated that initiating basal insulin treatment in insulin-naive individuals with T2DM led to improved glycemic parameters over a 12-month period.
Similar content being viewed by others
Introduction
The global burden of diabetes is steadily increasing, owing primarily to increased sedentary behavior, an overweight/obese population, and unhealthy lifestyles. Diabetes is rapidly increasing in low- and middle-income countries [1]. According to International Diabetes Federation (IDF) 2022, 8.3% of Indian population is estimated to have diabetes [2].
Type 2 diabetes (T2DM) is characterized by worsening hyperglycemia due to a progressive decline in pancreatic β-cells function and a deficit of β-cell mass. Uncontrolled diabetes is associated with the risk of vascular diseases, and long term macrovascular and microvascular complications [3]. Because of the progressive nature, a timely treatment strategy is, therefore, necessary to achieve and maintain optimal glycemic control early in the course of disease. Oral antidiabetic drugs (OADs) are the mainstay of therapy though limited in their ability to maintain glycemic control in long-term use [4]. Initiation of insulin therapy is required when lifestyle modifications combined with OADs fail to achieve metabolic control [5]. There is increasing support for the early initiation of insulin in people with T2DM to ensure target glycemic control and avoid microvascular and macrovascular complications [3]. Basal insulin secretion is essential for maintaining fasting plasma glucose (FPG) levels, primarily by inhibiting excessive glucose output from the liver [4]. Insulin glargine is the first long-acting insulin analogue that provides a more convenient replacement of physiological basal insulin compared to older long-acting insulin formulations [6]. Insulin glargine is thought to provide a more even distribution of insulin throughout the day, help achieve target glycemic control with once daily injection, and reduce the risk of hypoglycemia [7].
There is limited information available on the clinical management of people with T2DM in India, who were started on insulin glargine after failure of OADs. Therefore, the REALITY study was planned to explore the demographic profile, insulin usage patterns and outcomes in insulin-naïve participants with T2DM.
Materials and methods
This multicentric, non-interventional, retrospective, electronic medical record (EMR)-based study was conducted to explore the real-world insulin usage patterns and their longitudinal outcomes in insulin-naïve participants with T2DM. In the study, a total of 1006 insulin naive T2DM participants of ≥ 18 years age, who were initiated on insulin during the index period of January 01, 2016, to December 31, 2018, were enrolled. People with T1DM, T2DM of < 5 years duration, gestational diabetes, secondary diabetes (e.g., fibro calculus pancreatic diabetes), cancer, end-stage liver disease, end-stage renal failure, treatment with short-term insulin therapy (< 1 month) and those using other investigational drugs concurrently, were excluded from the study.
Analyses were performed using version 9.4 of SAS statistical software (SAS Institute Inc., Cary, NC, USA). Descriptive analyses were reported as mean, standard deviation (SD), minimum (min), maximum (max), median, interquartile range (IQR), percentages, and frequency count (n) for each evaluable parameter. The categorical variables were summarized using the frequency count (n) and percentage (%) for each possible value. The level of significance for statistical tests was 0.05 two-sided. p-values for statistical tests were provided with 4 decimals, or as < 0.0001.
Insulin outcome evaluation
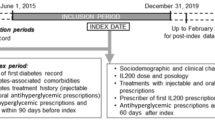
At baseline, demographic, anthropometric and clinical characteristics including glycated hemoglobin (HbA1c), FPG, postprandial plasma glucose (PPG), anti-diabetic medications, co-morbidities prior to insulin initiation were abstracted from participants’ medical records. Data on the insulin usage pattern (dose and type of insulin, frequency of administration), mean / median changes in insulin dose and outcome parameters for HbA1c, FPG, PPG, body weight and the incidence of hypoglycemia were collected from EMRs at 3, 6, and 12 months after initiation of insulin therapy. The mean / median change in the HbA1c levels was reported at 6 months and 12 months post-initiation of insulin glargine. The prescription patterns of OADs post initiation of insulin were also assessed at 3, 6 and 12 months. Details on study schedule are provided in Fig. 1.
Results
The study included 1006 participants with T2DM (55.8% [n = 561] men) having a mean age of 59.8 ± 11.8 years and an average T2DM duration of 12.0 ± 6.6 years. The mean height of the participants was 162.4 ± 98.8 cm, weight was 70.8 ± 12.8 kg, and BMI was 26.9 ± 4.7 kg/cm2. The baseline systolic blood pressure was 128 ± 15 mmHg and diastolic blood pressure was 78 ± 9 mmHg. The most noted comorbidities were hypertension in 50.9% (n = 512), dyslipidemia in 28.8% (n = 290), hypothyroidism in 9.6% (n = 97), and coronary artery disease in 4.1% (n = 41) participants. Additional baseline characteristics of insulin-naïve participants with T2DM are presented in Table 1.
Glycemic parameters at baseline
Overall, the HbA1c value was recorded for 76.1% (n = 766) participants with a mean of 8.9 ± 1.9%. The FPG of > 130 mg/dL was reported for 55.6% (n = 559) participants with a mean of 201 ± 54 mg/dL. While 5.5% (n = 55) participants reported > 180 mg/dL PPG with a mean of 276 ± 72 mg/dL.
In the insulin glargine group (U100 and U300; n = 673), the mean HbA1c was 9.0 ± 1.7%; of these 63.7% (n = 429) participants had HbA1c ≥ 7%. The FPG of ≥ 130 mg/dL was reported for 44.5% (n = 300) participants with a mean of 209 ± 55 mg/dL. While PPG of ≥ 180 mg/dL was reported for 42.5% (n = 286) participants with a mean of 298 ± 71 mg/dL.
Glycemic parameters of the overall population and the insulin glargine group at various study intervals are presented in Table 2.
Insulin usage pattern at baseline
At the onset (baseline), 66.9% (n = 673) participants were on insulin glargine; 34.1% (n = 343) on U100 (insulin glargine 100 IU per mL [Gla-100]) and 24.8% (n = 249) on U300 (insulin glargine 300 IU per mL [Gla-300]). Information on the type of insulin glargine was unavailable for 8.1% (n = 81) participants.
Other major types of insulin noted were insulin degludec in 15.1% (n = 152), human insulin in 11.1% (n = 112), and insulin isophane in 9.2% (n = 93) participants. Among other categories of insulin (ultra-short/fast-acting), insulin lispro was noted in 4.1% (n = 41) and insulin glulisine in 0.6% (n = 6) participants. Short-acting, insulin aspart was noted in 16.4% (n = 165), regular insulin in 7.4% (n = 74), and intermediate-acting insulin isophane in 9.2% (n = 93) participants. A combination of fast and intermediate-acting, insulin aspart protamine and insulin lispro protamine was noted in 1.8% (n = 18) and 1.7% (n = 17) participants, respectively.
The median (IQR) dose of insulin glargine (Gla-100, n = 343; Gla-300, n = 249; Gla-unclassified, n = 81) was 14.0 (10, 20) IU; and it was most frequently administered at bedtime (58.2%; n = 392) and once daily (39.2%; n = 26). The median dose of insulin aspart, insulin degludec and human insulin was 16.0 IU, 15.0 IU, and 20.0 IU, respectively. Insulin aspart and insulin degludec were taken once daily by most participants and human insulin was taken twice daily.
Information on insulin usage pattern (including dose and frequency) at baseline is provided in Table 3.
Insulin glargine group assessment at 3, 6 and 12 months
Based on the records/data available, the use and change in dose of insulin glargine was noted for 24.7% (n = 166), 32.4% (n = 218) and 21.8% (n = 147) participants at 3, 6 and 12 months, respectively. The median (IQR) change in dose of insulin glargine from baseline to 3, 6 and 12 months was 4.0 IU (2, 6), 4.0 IU (1, 6), and 8.0 IU (4, 12), respectively (Table 4). For the insulin glargine group, an improvement in HbA1c, FPG, and PPG levels was indicated during the study. The change in body weight was minimal throughout the study (Table 5).
Hypoglycemic events in the insulin glargine subset
At 3 months, a total of 43 hypoglycemic events (38 mild, 4 moderate, and 1 severe) were noted in 39 participants of insulin glargine subset (N = 673). None of events were life-threatening or required hospitalization. The severe hypoglycemic event was serious in nature reported with antidiabetic medications: metformin, glimepiride, vildagliptin, canagliflozin and insulin glargine U100. Hypoglycemia was possibly related to antidiabetic therapy in 36 events and not related in 7 events. Forty hypoglycemic events were resolved, 1 recovered with sequelae and status of 2 events was unknown.
At 6 months, 58 hypoglycemic events (47 mild, and 11 moderate) were noted in 45 participants of insulin glargine subset (N = 673). Thirty-seven events were possibly related to antidiabetic medication, 1 unlikely and 20 were not related. Fifty-six events were resolved, and the status of the 2 events was unknown.
At 12 months, a total of 36 hypoglycemic events (32 mild, and 4 moderate) were reported in 26 participants of insulin glargine subset (N = 673). Twenty-seven events were possibly related to antidiabetic medication, 1 unlikely and 8 were not related. Thirty-two events were resolved, and the status of 4 events was unknown.
Oral antidiabetic drugs usage throughout the study
Prior to insulin initiation, 63.4% (n = 638), 45.8% (n = 461) and 35.7% (n = 359) participants were taking at least one, two, or three OADs, respectively. The most noted OADs were biguanides (60.5%; n = 609), sulfonylureas (41.1%; n = 413), and dipeptidyl peptidase-4 inhibitors (36.1%; n = 363). As per the records, the usage patterns remained almost same across different time points with biguanides, sulfonylureas, and dipeptidyl peptidase-4 inhibitors as the most common OADs.
Missing values
Since it was a retrospective EMR-based study, all the required information was not available in the medical records, and no imputations were made for missing values.
Discussion
This multicentric retrospective study evaluated the demographic profile of insulin-naïve T2DM Indian participants initiated on insulin in a larger cohort. In addition, the study assessed the insulin usage pattern, the glycemic parameters, and incidences of hypoglycemia. Most participants were initiated with insulin glargine and improvement in glycemic parameters was indicated over 12 months.
In our study, the mean age of T2DM participants was comparable with other Asian population-based real-world studies [8]. We noted that, 66% individuals of the total enrolled population were obese (BMI ≥ 25 kg/m2). A cross-sectional registry-based retrospective study in India noted that 46.4% of the participants were obese and were younger (54.6 ± 11.0 years) compared to our study population [9].
In our study, most insulin-naïve participants had at least one comorbid condition, commonly hypertension (50.9%) and/or dyslipidemia (28.8%). Other studies in India also show a higher prevalence of vascular and lipid metabolic disorders in people with diabetes [10,11,12]. As per American Diabetes Association (ADA), hypertension and dyslipidemia are among the top 15 comorbid conditions commonly observed in people with T2DM [13].
The Indian Council of Medical Research (ICMR) and Research Society for the Study of Diabetes in India (RSSDI) guidelines recommend the use of insulin in people with T2DM having HbA1c > 9% [14]. In this study HbA1c at baseline was 8.9 ± 1.9% which is high and, about 67% of participants at baseline were taking insulin glargine, which is considered safer in terms of reducing the risk of hypoglycemia, compared to short-acting insulin. Basal insulin was chosen in accordance with available literature and RSSDI recommendations [15].
The mean FPG noted at baseline in our study is similar to that reported in an Asian population-based study [10]. While PPG noted in our study was higher and HbA1c levels were on the lower side compared to another Indian population-based study [16]. Among all the components present in an individual's diet, carbohydrates exert the most significant impact on blood glucose levels. The quantity and type of carbohydrates consumed are pivotal factors influencing postprandial glucose levels. The prevalence of high carbohydrate intake within the population may be a contributing factor to elevated postprandial glucose levels [17].
In the insulin glargine group of our study, there was an improvement in the HbA1c, FPG and PPG levels throughout the study duration. ATOS, a multi-country, real-world study assessed the effectiveness and safety of insulin glargine 300 U/mL in insulin-naïve people with T2DM. The ATOS study reports a reduction in HbA1c by − 1.5% and − 1.9%, at 6 and 12 months, respectively [10]. FPG was also reduced by − 3.4 mmol/L and − 3.9 mmol/L at 6 and 12 months, respectively. Higher levels of HbA1c and FPG reduction seen in the ATOS study may be associated with higher baseline values of HbA1c and FPG compared to our study [10].
The weight change was minimal throughout our study (3, 6 and 12 months), which is supported by another real-world study conducted in wider geographic regions (Asia, the Middle East, North Africa, Latin America, and Eastern Europe) [10]. However, a study based on post-hoc analysis of 16 clinical trials where insulin therapy was initiated with the OADs, reported a substantial increase in body weight in Asian compared to non-Asian subjects [18].
In our study, a total of 43 hypoglycemic events were reported at 3 months, 58 events reported at 6 months, and 36 events reported at 12 months. The hypoglycemic events reported in our study are comparable to the real-world ATOS study [10].
We note that biguanides (60.5%), sulfonylureas (40.1%), and dipeptidyl peptidase-4 (DPP-4) inhibitors (36.1%) were the most used OADs. Similarly in ATOS, biguanides were the most used OAD at baseline (88.9%), followed by sulfonylureas (73.0%) and DPP-4 inhibitors (43.5%). Our findings are consistent with the pattern of treatment followed in India.
This study provides real-world data on the insulin usage patterns and the outcomes in Indian people with T2DM. A major limitation of the study was its retrospective nature and the dependency on secondary data source through EMRs. Therefore, there were challenges of computing missing data, including loss to follow-up at various stages of the study. Additionally, because of the EMR-based study design, the incidences of hypoglycemia may have been under-reported. There could also be a potential center selection bias. Another challenge was missing data on insulin education of patients, their compliance, storage, site, technique of administration and information on dietary survey. The scope and nature of the present research did not focus on the biochemical parameters and its significance in capturing the outcomes of insulin usage. Hence, further, large, and complete dataset studies would be required to validate our study findings.
Conclusion
In this EMR-based REALITY study, focusing on insulin-naïve participants with T2DM in India, most individuals were initially prescribed insulin glargine. The results highlighted a noteworthy improvement in glycemic parameters over a 12-month period. The study identified hypertension and dyslipidemia as the most prevalent comorbid conditions, while biguanide and sulfonylurea emerged as the most preferred concomitant antidiabetic medications. Furthermore, the changes in body weight and the occurrence of hypoglycemic events were found to be comparable to similar real-world studies.
Data Availability
Qualified researchers may request access to patient-level data and related documents [including, e.g., the clinical study report, study protocol with any amendments, blank case report form, statistical analysis plan, and dataset specifications]. Patient-level data will be anonymized, and study documents will be redacted to protect the privacy of trial participants. Further details on Sanofi’s data sharing criteria, eligible studies, and process for requesting access can be found at https://vivli.org/.
References
World Health Organization. Diabetes. [Last accessed on 04 Jun 2021]. Available from: https://www.who.int/health-topics/diabetes.
International Diabetes Federation. [Last accessed on 07 Apr 2023 ]. https://idf.org/our-network/regions-members/south-east-asia/members/94-india.html.
Pradeepa R, Mohan V. Prevalence of type 2 diabetes and its complications in India and economic costs to the nation. Eur J Clin Nutr. 2017;71:816–24.
Hilgenfeld R, Seipke G, Berchtold H, Owens DR. The evolution of Insulin Glargine and its continuing contribution to diabetes care. Drugs. 2014;74(8):911–27.
Bretzel RG, Eckhard M, Landgraf W, Owens DR, Linn T. Initiating insulin therapy in type 2 diabetic patients failing on oral hypoglycemic agents: basal or prandial insulin? The APOLLO trial and beyond. Diabetes Care. 2009;32(Suppl 2):S260-5.
Singhai A, Banzal S, Joseph D, Jha RK. Comparison of Insulin Glargine with human premix insulin in patients with type 2 diabetes inadequately controlled on oral hypoglycemic drugs in a 24 week randomized study among central Indian population. Indian J Clin Pract. 2013;2(2):619–23.
Pearson SM, Trujillo JM. Conversion from insulin glargine U-100 to insulin glargine U-300 or insulin degludec and the impact on dosage requirements. Ther Adv Endocrinol Metab. 2018;9(4):113–21.
Kong APS, Lew T, Lau ESH, et al. Real-world data reveal unmet clinical needs in insulin treatment in Asian people with type 2 diabetes: the Joint Asia Diabetes Evaluation (JADE) Register. Diabetes Obes Metab. 2020;22(4):669–79.
Baruah MP, Kalra S, Bose S, Deka J. An Audit of Insulin Usage and Insulin Injection Practices in a Large Indian Cohort. Indian J Endocrinol Metab. 2017;21(3):443–52.
Galstyan GR, Tirosh A, Vargas-Uricoechea H, et al. Real-World Effectiveness and Safety of Insulin Glargine 300 U/mL in Insulin-Naïve People with Type 2 Diabetes: the ATOS Study. Diabetes Ther. 2022;13:1187–202.
Rathi A, Bansal R, Saha K. Presence of Co-Morbidities in Patients Suffering from Diabetes Mellitus Type-2 Attending Two Clinics in Delhi. MOJ Immunol. 2017;5(3):00160.
Podder V, Srivastava V, Kumar S, et al. Prevalence and Awareness of Stroke and Other Comorbidities Associated with Diabetes in Northwest India. J Neurosci Rural Pract. 2020;11(3):467–73.
American Diabetes Association [Last accessed on 2023 Apr 07]. https://professional.diabetes.org/abstract/recent-top-15-comorbid-conditions-among-patients-type-2-diabetes-mellitusmdasha-large, Accessed on 30 Sep 2022.
Chawla R, Madhu SV, Makkar BM, Ghosh S, Saboo B, Kalra S, RSSDI-ESI Consensus Group. RSSDI-ESI Clinical Practice Recommendations for the Management of Type 2 Diabetes Mellitus 2020. Indian J Endocrinol Metab. 2020;24(1):1–122.
ICMR Guidelines for Management of Type 2 Diabetes 2018. [Last accessed on 2023 Apr 07]. https://main.icmr.nic.in/sites/default/files/guidelines/ICMR_GuidelinesType2diabetes2018_0.pdf.
Borgharkar SS, Das SS. Real-world evidence of glycemic control among patients with type 2 diabetes mellitus in India: the TIGHT study. BMJ Open Diabetes Res Care. 2019;7(1): e000654.
Chawla R, Mukherjee JJ, Chawla M, Kanungo A, Shunmugavelu MS, Das AK. Expert Group Recommendations on the Effective Use of Bolus Insulin in the Management of Type 2 Diabetes Mellitus. Med Sci (Basel). 2021;9(2):38.
Chan JCN, Bunnag P, Chan SP, et al. Glycaemic responses in Asian and non-Asian people with type 2 diabetes initiating insulin glargine 100 units/mL: A patient-level pooled analysis of 16 randomised controlled trials. Diabetes Res Clin Pract. 2018;135:199–205.
Acknowledgment
The authors would like to thank Dr. Ravi Kant (Project management), Mohd. Rashid Khan (statistical data analysis) and Dr. Shweta Varshney (manuscript writing/review and submission) from IQVIA Consulting and Information Services India Private Limited. Editorial support was also provided by Kedar Gandhi, Vaibhav Revandkar, and Anahita Gouri of Sanofi, India.
Funding
This study was funded by Sanofi Mumbai, India.
Author information
Authors and Affiliations
Contributions
All authors adhered to the ICMJE authorship criteria.
Conceptualization- M Chawla, B Makkar, K Modi, S Phatak, S Waghdhare, A Satpathy, A Gadekar, D Chodankar, C Trivedi, K P Kumar and V Mohan;
Data curation- A Gadekar, D Chodankar and C Trivedi;
Funding acquisition- A Gadekar, A Chodankar and C Trivedi;
Investigation- M Chawla, B Makkar, K Modi, S Phatak, S Waghdhare, K P Kumar and V Mohan;
Methodology- B Makkar, S Phatak, S Waghdhare, A Satpathy, A Gadekar, D Chodankar, C Trivedi, K P Kumar and V Mohan;
Project administration- A Gadekar, D Chodankar and C Trivedi;
Resources- M Chawla, K Modi, S Phatak, D Chodankar and C Trivedi;
Supervision- M Chawla, B Makkar, K Modi and A Satpathy;
Validation- M Chawla, B Makkar, K Modi, S Phatak, S Waghdhare, A Satpathy, A Gadekar, D Chodankar and C Trivedi;
Visualization- M Chawla, D Chodankar and K P Kumar;
Writing (review & editing)- A Gadekar.
Corresponding author
Ethics declarations
Ethics statement
Ethical approval for the study was obtained from the local ethics committee.
CTRI number
CTRI/2021/03/031796.
Conflicts of interest
Authors declare no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A. Satpathy is an Ex-employee of Sanofi.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chawla, M., Makkar, B.M., Modi, K.D. et al. A retrospective electronic medical record-based study of insulin usage and outcomes in insulin-naive Indian adults with T2DM: The REALITY study. Int J Diabetes Dev Ctries (2023). https://doi.org/10.1007/s13410-023-01294-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13410-023-01294-1