Abstract
Objective
The aim of this study is to explore the correlation between vitamin D and diabetic nephropathy.
Methods
Relevant evidences were searched from PubMed, Embase, Web of Science, Ovid and China Knowledge Resource Integrated (CNKI), Wanfang Data Knowledge Service Platform databases (WANFANG), and VIP dating from inception to December 2019 to obtain the randomized controlled trials (RCTs) of vitamin D in the treatment of diabetic nephropathy. According to inclusion and exclusion criteria, two researchers independently screened the literature, extracted data, and evaluated the quality of included studies. Rev Man 5.3 software was used to conduct statistical analysis.
Results
A total of 10 studies involving 651 patients were identified. These studies were finally included into the meta-analysis. A meta-analysis results showed that vitamin D is the protection factor in diabetic nephropathy, the group treated with vitamin D did better than the traditional drug and the placebo group. After taking vitamin D, the level of vitamin D in the patient’s body increased significantly. Pooled results showed that there was a significant difference for vitamin D (MD = 38.24, 95%CI = 32.69–43.79, p < 0.001.) The patient had a significant decrease in urinary protein; the difference was statistically significant (MD = − 180.92, 95%CI = − 212.67 to − 149.16, p < 0.001). The blood creatinine content decreased obviously (MD = − 17.13, 95%CI = − 27.88 to − 6.37, p < 0.01). However, most of the included studies did not report the quality of life and adverse reactions of patients, making it impossible to analyze these measures.
Conclusion
This study showed that vitamin D played an active role in the treatment of diabetic nephropathy and can be used in future clinical applications. However, there are still some studies of low quality in the included studies, so it is suggested that clinical and scientific researchers carry out more high-quality, large sample, multi-center randomized controlled trials (RCTS) to provide more evidence-based medical evidence for future studies on vitamin D treatment of diabetic nephropathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the World Health Organization (WHO), there are currently at least 415 million people with diabetes and 318 million people with impaired glucose tolerance [1]. Diabetic nephropathy is one of the most concerned chronic microvascular complications in diabetic patients, and is an important cause of death in diabetic patients, as well as the main cause of end-stage nephropathy [2, 3]. Diabetic nephropathy is managed by controlling blood sugar, blood pressure, lipids, urine protein, and improving the way of life to delay the process of end-stage nephropathy [4].
Vitamin D is a steroid hormone which is converted by the liver and kidneys into bioactive 1,25 (OH) 2D3 and acts on the body. Studies showed that vitamin D was associated with pathogenesis of inflammation, immunity, cancer, musculoskeletal system, metabolic disease, cardiovascular system, and psychiatric nervous system, including diabetes and its complications [5]. A growing body of research has linked vitamin D to diabetic kidney disease, but there is no detailed and reliable evidence for evidence-based medicine. Therefore, this paper searched and screened the data of randomized controlled trials of vitamin D and diabetic nephropathy. Meta-analysis was used to study the correlation between vitamin D and diabetic nephropathy, so as to provide guidance for the subsequent clinical prevention and even treatment of diabetic nephropathy.
Materials and methods
Literature retrieval
Two researchers independently searched databases including PubMed, Web of Science, Embase, Ovid databases, China Knowledge Resource Integrated (CNKI), Wanfang Data Knowledge Service Platform databases (WANGFANG), and VIP from inception to December 2019. Using the search terms “Vitamin D,” “25(OH)D,” “diabetic nephropathy,” and “DN.” Publications were limited to the English and Chinese.
Inclusion criteria
Studies were included if they met the following inclusion criteria: (1) The literature type is randomized controlled trials (RCTs). (2) The subjects were diabetic nephropathy patients. (3) The study focused on the relationship between vitamin D and diabetic nephropathy. (4) The research report provided the required data.
Exclusion criteria
Studies were excluded if they met the following inclusion criteria: (1) Unclear statistical methods and data description. (2) Full text unavailable. (3) Repetitive literature. (4) Case reports, literature, and review articles. (5) Experiments on animals.
Study selection and data extraction
Firstly, two researchers independently complete the preliminary screening of the article by reading the title and abstract, and the third researcher makes the decision if there are different opinions. Then, according to the inclusion and exclusion criteria, the two researchers screened the articles by reading the full text, if there were differences between the two researchers, the third researcher would make a judgment. Data were also extracted independently by two investigators to ensure that the precise targeted data were collected. The following data were extracted from each of the included studies: general information of patients, the number of cases and intervention measures in treatment group and control group, effective rate, adverse reaction, and other outcome indicators, author information, year of publication, etc.
Qualitative evaluation
The qualitative evaluation of the studies was based on Cochrane Handbook for Systematic Reviews of Interventions (version 5.0) [6]: The main evaluation content includes the following several aspects: random sequence, allocation concealment, blinding of participants and personal, blinding of outcome assessment, incomplete outcome data, selective reporting, other sources of bias. In all cases, the answer “yes” indicated a low risk of bias, the answer “no” indicated a high risk of bias, and the answer “unclear” indicated an uncertain risk of bias. The quality evaluation shall be conducted independently by two professional researchers and cross-checked. In case of differences, the third party shall make a decision.
Statistical method
The RevMan 5.3 software provided by the Cochrane collaboration was used for meta-analysis of the included RCTs. Combined OR ratio (OR) was used for counting data, and weighted standard deviation (MD) was used for measurement data, with 95% confidence interval (CI) as the effect size for both. The heterogeneity of the included data was analyzed by chi-square test. If I2 ≤ 50%, there was no statistical heterogeneity among the studies, and the fixed effect model was selected for analysis. If I2 > 50%, it indicated statistical heterogeneity between studies. Random effect model was selected for meta-analysis, and the causes of heterogeneity were analyzed.
Results
Literature search results
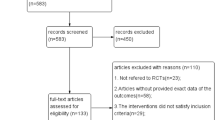
Through NoteExpress document management software combined with manual re-checking, repetitive documents were eliminated, and irrelevant documents were excluded by reading the titles and summaries. Download the full text of relevant literature and to read it carefully before further screening and completing subsequent data extraction. A total of 1273 studies were retrieved through the retrieval strategy, including 299 PubMed, 4 Web of Science, 105 Ovid databases, 0 EmBase, 366 CNKI, 410 Wanfang database, and 89 VIP database. According to the inclusion and exclusion criteria, 269 studies were checked and excluded. Finally, 10 studies were included, with a total of 651 patients. The screening processing is summarized in Fig. 1.
Study characteristics
Ten studies met the inclusion criteria, with a total of 651 patients, including 335 in the treatment group and 316 in the control group, which were involved in both domestic and foreign studies. The study period of 4 studies [9,10,11, 16] was 12 weeks, that of 3 studies [8, 12, 14] was 24 weeks, and 3 studies [7, 13, 15] was 8 weeks. General information of the included studies was shown in Table 1, including the general information of patients, the first author and year of publication, country, the number of cases and intervention measures in treatment group and control group, intervention, the duration of treatment, and outcomes. For more details, see Table 1.
Quality assessment
Risk bias graphs were drawn from 10 included studies. Only 4 [9, 13, 15, 16] referred to specific randomized methods, 3 [13,14,15] to allocation concealment, 4 [13,14,15,16] to double-blind methods, and only 1 to adverse reactions, all referring to changes in patients’ quality of life. The methodological quality evaluation of the included studies was shown in Table 2.
Meta-analysis results
Vitamin D levels
There were 6 studies [7, 8, 13,14,15,16] mentioned vitamin D after the intervention patients before and after the change of the vitamin D levels in the body. There were statistical heterogeneity (p < 0.001,I2 = 95%) between the treatment group and control group. Thus, the random effect model was used for analysis. The pooled results indicated that there was a significant difference in the two groups (MD = 32.87, 95%CI: 20.59 to 45.16, p < 0.001). The detailed results were shown in Fig. 2A below. The studies were transformed into fixed-effect models, and the included studies were statistically analyzed again. Each study was removed one by one, and a new meta-analysis was conducted. Sensitivity analysis showed that there was no statistical heterogeneity (p = 0.18, I2 = 42%) after removing the studies of Esfandiari et al [13], Barzegari et al [15] and Ahmadi et al [16]. The pooled results indicated that there was a significant difference in the two groups (MD = 38.24, 95%CI: 32.69 to 43.79, p < 0.001), suggesting that Esfandiari et al [13], Barzegari et al [15], and Ahmadi et al [16] were the source of heterogeneity. The detailed results are shown in Fig. 2B.
HbA1c
HbA1c reflected a patient’s glycemic control over the past 3 months, so HbA1c provided a patient’s long-term glycemic trend. Three studies [7, 13, 16] mentioned changes in HbA1c before and after intervention, including 83 patients in the treatment group and 78 patients in the control group. There was no statistical heterogeneity (p = 0.88, I2 = 0%) between the treatment group and control group. Thus, the fixed effect model was used for analysis. The pooled results indicated that there was no significant difference in the two groups (MD = 0.02, 95%CI: − 0.37 to 0.41, p = 0.92). The meta-analysis of HbA1c between the treatment group and control group was shown in Fig. 3.
Urine protein analysis
Three of the included studies [7, 10, 11] involved changes in urinary protein. Proteinuria is one of the major markers of renal disease, and accurate measurement of clinically significant proteinuria is important for the diagnosis and management of renal disease [17]. There was statistical heterogeneity between groups in the included studies (p < 0.001, I2 = 93%). The randomized model was used for meta-analysis. The pooled results indicated that there was no significant difference in the two groups (MD = − 564.42, 95%CI: − 1153.85 to 25.02, P = 0.06). The result was shown in Fig. 4A. The studies were transformed into fixed-effect models, and the included studies were statistically analyzed again and a new meta-analysis was conducted. After removing Shi et al [10], the heterogeneity test of the remaining two studies showed no significant statistical heterogeneity (p = 0.21, I2 = 35%), indicating that Shi et al [10] was the source of heterogeneity. The pooled results indicated that there was a significant difference in the two groups (MD = − 180.92, 95%CI: − 212.67 to − 149.16, p < 0.001). Moreover, it can be seen that the treatment group with vitamin D has a statistically significant effect on the reduction of urinary protein, as shown in Fig. 4B.
Creatinine analysis
As can be seen from Fig. 5A, there was statistical heterogeneity between groups (p = 0.02, I2 = 75%), and meta-analysis using a random model showed no statistical significance (MD = − 10.23, 95%CI: − 24.02 to 3.55, p = 0.15). The included studies were transformed into fixed effect models, and the included studies were statistically analyzed again. Each study was removed one by one and a new meta-analysis was conducted. After removing Shi et al [10], there was no statistical heterogeneity between the remaining two groups (p = 0.88, I2 = 0%), which indicated that Shi et al [10] was the source of heterogeneity. After removal, meta-analysis was conducted again, and the results were shown in Fig. 5B. The results were statistically significant (MD = − 17.13, 95%CI: − 27.88 to − 6.37, p = 0.002) indicating that vitamin D was a protective factor for patients with diabetic nephropathy.
Adverse reactions and quality of life
None of the included studies mentioned changes in quality of life, and only Mei et al [12] mentioned adverse reactions, so it cannot be analyzed here.
Discussion
Diabetes is a chronic infectious disease that is currently prevalent. Like other epidemics, it is characterized by the fact that it is difficult to cure within a short period of time, and patients with diabetes often undergo long-term treatment. Diabetic nephropathy (DN) is a serious diabetic microvascular complication that reference for statistic quarter of diabetics are affected and is one of the leading causes of end-stage nephropathy worldwide. Diabetic nephropathy is caused by the changes in the structure of glomerular capillaries and renal tubules as well as the disorder of glucose homeostasis. However, the research on the treatment and prevention of diabetic nephropathy is still an ongoing task.
At present, Mogensen staging is widely used in clinical staging of diabetic nephropathy [18]. Diabetic nephropathy was divided into 5 stages, including acute glomerular hyperfiltration, normal albuminuria, early stage diabetic nephropathy, clinical diabetic nephropathy stage, and renal failure. The treatment of diabetic nephropathy is mainly in the first three stages; at this time, the further deterioration of diabetic nephropathy could be prevented by strict control of blood sugar and good control of blood pressure and lipids, and the application of ACEI or ARB drugs to reduce urinary protein. Once the disease progresses to stage 4 or 5, the use of these drugs can only delay the rate of deterioration of kidney function, which will eventually progress to the stage of uremia. Diaz et al. [19] found that diabetic patients with low vitamin D levels had a higher risk of kidney disease. Tiryaki et al. [20] found that proteinuria was significantly reduced in patients with early diabetic nephropathy treated with vitamin D. Another analysis found that diabetic nephropathy patients with urine protein significantly decreased, and not affected by GFR, blood pressure, and ACEI, after 23 weeks of oral pericalcinol [21]. Therefore, early detection of 25-OH-VD level and timely supplementation of vitamin D in diabetic nephropathy is of great significance to protect the kidney and delay the deterioration of diabetic nephropathy. This is also consistent with the results of this study.
The main mechanism of vitamin D in diabetic nephropathy is reflected in the following aspects. First and foremost, vitamin D had the effect of inhibiting inflammatory factors such as interleukin (IL)-1, IL-6, and tumor factors [22]. Manion et al. [23] believed that patients with vitamin D deficiency had a 23% higher level of IL-6 than those with normal vitamin D. An open, prospective, single-center clinical study showed that oral administration of pericalcitol for 12 weeks significantly reduced serum and peripheral blood monocytes TNF-α and IL-6 levels in patients [24]. Secondly, vitamin D can improve insulin sensitivity and reduce the risk of diabetes. Type 2 diabetes accounts for up to 90% of diabetes patients. The study found that the main pathogenesis of type 2 diabetes mellitus is decreased function and number of pancreatic beta cells and insulin resistance [25]. Wang and Chen [26] found that islet β-cell function was significantly positively correlated with 25 (OH) D level in patients with type 2 diabetes. Several studies showed that taking vitamin D not only increased insulin sensitivity, but also positively regulated insulin signaling pathways [27, 28]. Thirdly, by adjusting the renin-angiotensin system (RAS), to reduce the formation of Angiotensin II, kidney damage caused by high blood sugar has a protective effect [29]. Studies showed that patients with diabetes renal interstitial angiotensin II 1000 times higher than that of healthy people [30]. Compared with RAS inhibitors alone, the combination of RAS inhibitors with VDRA palicalcinol was more effective in reducing proteinuria and renal damage in patients with diabetic nephropathy, a randomized controlled clinical study showed [31]. Therefore, vitamin D and RAS inhibitors have a synergistic effect in the treatment of diabetic nephropathy. Finally, vitamin D reduces podocyte hypertrophy and loss in the kidney, thereby reducing proteinuria and glomerulosclerosis. A number of recent randomized clinical trials have confirmed the antiproteinuric activity of vitamin D analogs in diabetic patients with CKD. Potent antiproteinuric activity of vitamin D has also been demonstrated in a variety of animal models of kidney disease. Treatment with 1,25-dihydroxyvitamin D (1,25(OH)2D3) or activated vitamin D analogs reduced albuminuria and prevented podocyte injury in 5/6 nephrectomized rats [32].
Vitamin D has important biological functions, such as regulating the immune system, affecting insulin secretion, improving insulin resistance, etc. For patients with diabetic nephropathy, vitamin D can well promote the absorption of calcium in glomerular filtrate. Given the prevalence of vitamin D deficiency in many populations and the potential link between vitamin D deficiency and adverse health outcomes, vitamin D deficiency is listed as a major public health problem [33]. Since complications of diabetes are closely related to microvascular disease, we wanted to study the correlation between vitamin D and diabetic nephropathy. However, in view of the small sample size of some included studies, we conducted a systematic review of meta-analysis to provide guidance for the clinical prevention and treatment of diabetic nephropathy in the future.
Our research has several advantages. The methodology was systematic and detailed, since the study’s efficacy was small, which may lead to a greater therapeutic effect than a large study. In addition, we made a meta-analysis of the researchable outcome indicators as much as possible. Although the results were uneven to some extent, we also used the random effects model, which took into account the changes at the research level. Furthermore, most of the RCTS included in this study were multi-center randomized controlled trials, and both Chinese and English studies were involved. The overall quality of the study was relatively high, and the results were of certain reference value. The results of the meta-analysis showed that, from the point of view of HbA1c in patients after taking vitamin D, the significance of taking vitamin D in lowering blood glucose was not obvious in the data obtained from this study. But compared with the control group, in the implementation of the vitamin D after the intervention, the patient’s body vitamin D levels rise obviously, urine protein and creatinine levels significantly lower for the patients with diabetic nephropathy, and renal protection has a positive meaning, thus the clinical treatment of diabetic nephropathy patients with vitamin D is also feasible.
However, this study also has some limitations. First, although randomized controlled trials at home and abroad are included, due to the small sample size and other problems, publication bias also exists to a certain extent. Second, although all of the studies included were randomized controlled trials, the blindness of several of the studies to evaluate the results was not clear, so there could be testing bias or confusion. Moreover, the existence of heterogeneity is inevitable due to the different duration of treatment. Finally, as diabetic nephropathy is a chronic disease, We think the quality of life of patients should be evaluated in the research. There is no research on the quality of life of patients. Therefore, the results should also be drawn with caution.
Conclusion
In conclusion, many patients with diabetic nephropathy are deficient in vitamin D. Vitamin D deficiency may play an important role in the pathogenesis of diabetic nephropathy, and timely supplementation of vitamin D may play an important role in the prevention and treatment of diabetic nephropathy. However, research on vitamin D intervention in diabetic nephropathy is limited, and more clinical trials or further evidence are needed to determine the effectiveness of vitamin D and provide additional evidence to guide vitamin D supplementation depending on the patient’s circumstances.
References
Sak D, Erdenen F, Müderrisoglu C, Altunoglu E, Sozer V, Gungel H, Guler P, Sak T, Uzun H. The relationship between plasma taurine levels and diabetic complications in patients with type 2 diabetes mellitus. Biomolecules. 2019;9(3):96.
Phillips CA, Molitch ME. The relationship between glucose control and the development and progression of diabetic nephropathy. Curr Diab Rep. 2002;2(6):523–9.
Sagoo MK, Gnudi L. Diabetic nephropathy: an overview. Methods Mol Biol. 2020;2067:3–7.
Yu S, Zhou HY, Hu XQ, et al. Progress in drug treatment of diabetic nephropathy. Chin J Integr Tradit West Med. 2019;28(31):3527–31.
Zhou YJ, Wang YY. Effects of vitamin D on diabetic nephropathy and its correlation. World’s latest medical information digest. 2019;19(71):112-113+115.
Frew AJ. 25. Immunotherapy of allergic disease. J Allergy Clin Immunol. 2003;111(2 Suppl):S712–9.
Zhang YH. Effect of vitamin D on proteinuria in patients with type 2 diabetes. Forum on primary medicine. 2017;21(22):2904-2905.
Gong YH, Han Y, Yan YH, et al. Effects of active vitamin D_3 on cardiac function in diabetic nephropathy patients with maintenance hemodialysis. Chin J Gerontol. 2014;34(22):6272–4.
Li YY, Liao YB, Zheng HY, et al. Effect of 1, 25-dihydroxyvitamin D_3 in the treatment of diabetic nephropathy. J Intern Med. 2019;25(01):26–8.
Shi DY, Zheng JC. Clinical study of 1,25 dihydroxyvitamin D3 in the treatment of diabetic nephropathy. J Clin Exp Med. 2016;15(23):2341–4.
Wang J, Chang BC. Clinical observation of 1, 25-dihydroxyvitamin D3 combined with irbesartan in the treatment of diabetic nephropathy. J Urol Int. 2014;34(1):58–60.
Mei RL, Yang YP, Li T. 1, 25 - dihydroxy vitamin D3 joint bering capsule on the clinical effect of the treatment of diabetic nephropathy period. China's health care nutrition (the ten-day), 2013(9).
Esfandiari A, Pourghassem Gargari B, Noshad H, Sarbakhsh P, Mobasseri M, Barzegari M, Arzhang P. The effects of vitamin D3 supplementation on some metabolic and inflammatory markers in diabetic nephropathy patients with marginal status of vitamin D: a randomized double blind placebo controlled clinical trial. Diabetes Metab Syndr. 2019;13(1):278–83.
Liyanage GC, Lekamwasam S, Weerarathna TP, Liyanage CE. Effects of high-dose parenteral vitamin D therapy on lipid profile and blood pressure in patients with diabetic nephropathy: A randomized double-blind clinical trial. Diabetes Metab Syndr. 2017;11(Suppl 2):S767–70.
Barzegari M, Sarbakhsh P, Mobasseri M, Noshad H, Esfandiari A, Khodadadi B, Gargari BP. The effects of vitamin D supplementation on lipid profiles and oxidative indices among diabetic nephropathy patients with marginal vitamin D status. Diabetes Metab Syndr. 2019;13(1):542–7.
Ahmadi N, Mortazavi M, Iraj B, Askari G. Whether vitamin D3 is effective in reducing proteinuria in type 2 diabetic patients? J Res Med Sci. 2013;18(5):374–7.
Liu F, Mao JH. Proteinuria and chronic renal disease. Chin J Pract Pediatr. 2016;31(11):816-820.
Mogensen CE. Microalbuminuria, blood pressure and diabetic renal disease: origin and development of ideas. Diabetologia. 1999;42(3):263–85.
Diaz VA, Mainous AG 3rd, Carek PJ, et al. The association of vitamin D deficiency and insufficiency with diabetic nephropathy: implications for health disparities. J Am Board Fam Med. 2009;22(5):521–7.
Tiryaki Ö, Usalan C, Sayiner ZA. Vitamin D receptor activation with calcitriol for reducing urinary angiotensinogen in patients with type 2 diabetic chronic kidney disease. Ren Fail. 2016;38(2):222–7.
Agarwal R, Acharya M, Tian J, Hippensteel RL, Melnick JZ, Qiu P, Williams L, Batlle D. Antiproteinuric effect of oral paricalcitol in chronic kidney disease. Kidney Int. 2005;68(6):2823–8.
Kassi E, Adamopoulos C, Basdra EK, Papavassiliou AG. Role of vitamin D in atherosclerosis. Circulation. 2013;128(23):2517–31.
Manion M, Hullsiek KH, Wilson EMP, Rhame F, Kojic E, Gibson D, Hammer J, Patel P, Brooks JT, Baker JV, Sereti I, for the Study to Understand the Natural History of HIV/AIDS in the Era of Effective Antiretroviral Therapy (the ‘SUN Study’) Investigators. Vitamin D deficiency is associated with IL-6 levels and monocyte activation in HIV-infected persons. PLoS ONE. 2017;12(5):e0175517.
Navarro-González JF, Donate-Correa J, Méndez ML, de Fuentes MM, García-Pérez J, Mora-Fernández C. Anti-inflammatory profile of paricalcitol in hemodialysis patients: a prospective, open-label, pilot study. J Clin Pharmacol. 2013;53(4):421–6.
Niroomand M, Fotouhi A, Irannejad N, Hosseinpanah F. Does high-dose vitamin D supplementation impact insulin resistance and risk of development of diabetes in patients with pre-diabetes? A double-blind randomized clinical trial. Diabetes Res Clin Pract. 2019;148:1–9.
Wang K, Chen N. The relationship between 25(OH)D and pancreatic beta cell function in type 2 diabetes mellitus. Shenzhen J Integr Tradit Chin West Med. 2020;30(20):26–8.
Liang F, Kume S, Koya D. SIRT1 and insulin resistance. Nat Rev Endocrinol. 2009;5(7):367–73.
Szymczak-Pajor I, Śliwińska A. Analysis of association between vitamin D deficiency and insulin resistance. Nutrients. 2019;11(4):794.
Hu X, Liu W, Yan Y, Liu H, Huang Q, Xiao Y, Gong Z, du J. Vitamin D protects against diabetic nephropathy: Evidence-based effectiveness and mechanism. Eur J Pharmacol. 2019;845:91–8.
Carey RM, Siragy HM. The intrarenal renin-angiotensin system and diabetic nephropathy. Trends Endocrinol Metab. 2003;14(6):274–81.
de Zeeuw D, Agarwal R, Amdahl M, Audhya P, Coyne D, Garimella T, Parving HH, Pritchett Y, Remuzzi G, Ritz E, Andress D. Selective vitamin D receptor activation with paricalcitol for reduction of albuminuria in patients with type 2 diabetes (VITAL study): a randomised controlled trial. Lancet. 2010;376(9752):1543–51.
Wang Y, Deb DK, Zhang Z, Sun T, Liu W, Yoon D, Kong J, Chen Y, Chang A, Li YC. Vitamin D receptor signaling in podocytes protects against diabetic nephropathy. J Am Soc Nephrol. 2012;23(12):1977–86.
Lerchbaum E, Trummer C, Theiler-Schwetz V, Kollmann M, Wölfler M, Heijboer AC, Pilz S, Obermayer-Pietsch B. Effects of vitamin D supplementation on androgens in men with low testosterone levels: a randomized controlled trial. Eur J Nutr. 2019;58(8):3135–46.
Acknowledgments
The authors would like to thank all those who contributed to this research.
Funding
National Basic Research Program of China: Study on identification of vital energy and spirit in TCM health status (number:2011CB505406).
Author information
Authors and Affiliations
Contributions
Xuan Sun and Hong-wu Wang participated in the conception and design of this article. Xuan Sun and Zhe Wang completed the data retrieval. Xuan Sun and Chun-ying Tian completed the preliminary article screening according to the title and abstract. If they have different opinions, Yuan-yuan Guan makes the decision. Then Xuan Sun and Dong-jun Wang completed the article screening according to the existing standards, if there were differences between the two researches, Huai-en Bu would make a judgment. Xuan Sun, Zhe Wang, and Hong-wu Wang completed the data extraction. Xuan Sun and Huai-en Bu completed the data evaluation. Xuan Sun completed the statistical analysis.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xuan, S., Jin, Z., Zhe, W. et al. A systematic review and meta-analysis of randomized control trials of vitamin D supplementation in diabetic nephropathy. Int J Diabetes Dev Ctries 43, 4–11 (2023). https://doi.org/10.1007/s13410-022-01108-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-022-01108-w