Abstract
Background
Patients with type 2 diabetes mellitus (T2DM) have risk of cardiovascular complications if blood glucose, blood lipids, and blood pressure (BP) are not optimally controlled. National Metabolic Management Center (MMC) has established a new management model to improve metabolic control.
Purpose
This study aimed to assess the level of metabolic control in T2DM patients under MMC and explore the relationship between clinical follow-up frequency and target-reaching rate of HbA1c, LDL-C, and BP.
Method
This was a retrospective study. Baseline measurements and follow-up data were collected from September 2017 to November 2019. The subjects were grouped according to the follow-up frequency as <4 times/year, =4 times/year, and >4 times/year.
Results
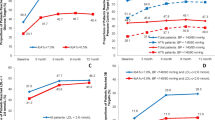
The positive changes in HbA1c and LDL-C were associated with follow-up frequency. After adjusting for confounders, the target-reaching rate of HbA1c for patients with follow-up ≥4 times/year was higher than those with <4 times/year, with odds ratios of 1.518 (=4 times/year) and 1.508 (>4 times/year). Compared to patients with follow-up <4 times/year, the target-reaching rate of LDL-C for patients with follow-up ≥4 times/year was higher, with odds ratios of 1.998 (=4 times/year) and 2.517 (>4 times/year). After 1 year of management, 48.91%, 47.43%, and 56.72% of patients achieved the target goals, respectively. 12.88% patients met all three targets.
Conclusion
MMC improves the target-reaching rate of HbA1c, BP, and LDL-C for T2DM patients in China. Compared with follow-up <4 times/year, follow-up 4 times/year has the maximum benefit of metabolic control in patients while >4 times/year was found no additional benefits than 4 times/year.
Similar content being viewed by others
References
Ebrahimi H, Emamian MH, Khosravi A, Hashemi H, Fotouhi A. Comparison of the accuracy of three diagnostic criteria and estimating the prevalence of metabolic syndrome: a latent class analysis. J Res Med Sci Off J Isfahan Univ Med Sci. 2019;24:108. https://doi.org/10.4103/jrms.JRMS_858_18.
Nuti L, Turkcan A, Lawley MA, Zhang L, Sands L, McComb S. The impact of interventions on appointment and clinical outcomes for individuals with diabetes: a systematic review. BMC Health Serv Res. 2015;15:355. https://doi.org/10.1186/s12913-015-0938-5.
Turkcan A, Nuti L, Delaurentis PC, Tian Z, Sands L. No-show modeling for adult ambulatory clinics. Springer New York. 2013. https://doi.org/10.1007/978-1-4614-5885-2_10.
McMahon GT, Fonda SJ, Gomes HE, Alexis G, Conlin PR. A randomized comparison of online- and telephone-based care management with internet training alone in adult patients with poorly controlled type 2 diabetes. Diabetes Technol Ther. 2012;14(11):1060–7. https://doi.org/10.1089/dia.2012.0137.
American Diabetes Association. Glycemic targets: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S66–76. https://doi.org/10.2337/dc20-S006.
Liu L, Lou Q, Guo X, Yuan L, Shen L, Sun Z, Zhao F, Dai X, Huang J, Yang H, Mordes JP, Chinese Diabetes Education Status Survey Study Group. Management status and its predictive factors in patients with type 2 diabetes in China: a nationwide multicenter study: a nationwide multicenter study. Diabetes/Metab Res Rev. 2015;31(8):811–6. https://doi.org/10.1002/dmrr.2757.
Zhang Y, Wang W, Ning G. Metabolic management center: an innovation project for the management of metabolic diseases and complications in China. J Diabetes. 2019;11(1):11–3. https://doi.org/10.1111/1753-0407.12847.
Gary TL, Batts-Turner M, Yeh HC, Hill-Briggs F, Bone LR, Wang NY, Levine DM, Powe NR, Saudek CD, Hill MN, McGuire M, Brancati FL. The effects of a nurse case manager and a community health worker team on diabetic control, emergency department visits, and hospitalizations among urban African Americans with type 2 diabetes mellitus: a randomized controlled trial. Arch Int Med. 2009;169(19):1788–94. https://doi.org/10.1001/archinternmed.2009.338.
Kaur R, Kajal KS, Kaur A, Singh P. Telephonic consultation and follow-up in diabetics: impact on metabolic profile, quality of life, and patient compliance. N Am J Med Sci. 2015;7(5):199–207. https://doi.org/10.4103/1947-2714.157483.
Pulgarón ER, Hernandez J, Dehaan H, Patiño-Fernandez AM, Carrillo A, Sanchez J, Delamater AM. Clinic attendance and health outcomes of youth with type 2 diabetes mellitus. Int J Adolesc Med Health. 2015;27(3):271–4. https://doi.org/10.1515/ijamh-2014-0021.
Pinhas-Hamiel O, Zeitler P. Barriers to the treatment of adolescent type 2 diabetes—a survey of provider perceptions. Pediatr Diabetes. 2003;4(1):24–8. https://doi.org/10.1034/j.1399-5448.2003.00027.x.
Rana JS, Liu JY, Moffet HH, Sanchez RJ, Khan I, Karter AJ. Risk of cardiovascular events in patients with type 2 diabetes and metabolic dyslipidemia without prevalent atherosclerotic cardiovascular disease. Am J Med. 2020;133(2):200–6. https://doi.org/10.1016/j.amjmed.2019.07.003.
Zhu J, Gao R, Zhao S, Lu G, Zhao D, Li J. Chinese guidelines for the prevention and treatment of blood lipids in adults. Chin Circ J. 2016;31(10):937–53.
Zuo HJ, Ma JX, Wang JW, Chen XR, Hou L. The impact of routine follow-up with health care teams on blood pressure control among patients with hypertension. J Hum Hypertens. 2019;33(6):466–74. https://doi.org/10.1038/s41371-018-0158-7.
Ji L, Hu D, Pan C, Weng J, Huo Y, Ma C, M, Y, Hao C, Ji Q, Ra, X, Su B, Zhuo H, Fox KA, Weber M, Zhang D. CCMR Advisory Board, & CCMR-3B STUDY Investigators. 2013: Primacy of the 3B approach to control risk factors for cardiovascular disease in type 2 diabetes patients. Am J Med. 2013;126(10), 925.e11–925.e9.25E22. https://doi.org/10.1016/j.amjmed.2013.02.035
Du Y, Heidemann C, Schaffrath Rosario A, Buttery A, Paprott R, Neuhauser H, Riedel T, Icks A, Scheidt-Nave C. Changes in diabetes care indicators: findings from German National Health Interview and Examination Surveys 1997-1999 and 2008-2011. BMJ Open Diabetes Res Care. 2015;3(1):e000135. https://doi.org/10.1136/bmjdrc-2015-000135.
Acknowledgments
The authors appreciate all the investigators and their staff for participation in this study.
Author information
Authors and Affiliations
Contributions
Study conception and design: QDZ and CYX
Data collection: QDZ, JHL, and XQL
Data analysis and interpretation: YW and ML
Drafting of the article: JHL and XQL
Critical revision of the article: CYX and QDZ
All of the authors approved the final version and agreed to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
It was approved by the Ethical Committee of Health Community Group of Yuhuan Second People’s Hospital. Participants provided written informed consent before enrollment.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jiaohong Luo, Chenyun Xu, Ying Wang, and Min Li hold author country’s registered Nurse license (RN).
Highlight
(1) MMC care improves the target-reaching rate of metabolic control for patients with type 2 diabetes
(2) Compared with <4 times/year follow-up frequency, 4 times/year follow-up has the maximum benefit of metabolic control in diabetic patients, while >4 times/year had no additional benefits
Rights and permissions
About this article
Cite this article
Luo, J., Long, X., Wang, Y. et al. Follow-up frequency impacts metabolic control in diabetes patients under MMC framework—a retrospective study. Int J Diabetes Dev Ctries 43, 398–404 (2023). https://doi.org/10.1007/s13410-022-01084-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-022-01084-1