Abstract
Background
Type 2 diabetes is a chronic metabolic disease characterized by vascular complications, the prevalence of which varies widely.
Aim
Determine the prevalence of microvascular and macrovascular complications in type-2 diabetes in North India and their correlation with various risk factors.
Design
Prospective observational study
Setting
Tertiary referral centres
Methods
A total of 6400 patients attending diabetes clinic were screened, out of which 6105 patients were enrolled during April 2018 to February 2021. Data were collected using a standardized electronic case record form. Prevalence estimates of microvascular and macrovascular complications were performed, and multivariate regression was applied for the analysis of correlation with known modifiable and non-modifiable risk factors. ROC analysis was done to find the best cut-offs for predictors of diabetic vascular complications.
Results
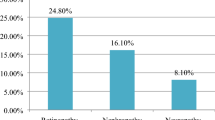
The mean age of the participants was 58.3 ± 9.1 years (57% males). The mean duration of diabetes was 11.3 ± 7 years and HbA1c was 8.4 ± 4%. Prevalent diabetic neuropathy was observed in 30.1%, nephropathy in 18.8% and retinopathy in 13.7%. Coronary artery disease (CAD) was prevalent in 15.7%, cerebrovascular accident (CVA) in 3.6% and foot complications in 2.9%. In the multivariate regression model, all microvascular complications significantly correlated with the longer duration of diabetes but the same was not observed for macrovascular complications. Obesity [BMI cut-off>26.4 kg/m2 (AUC 0.51, p=0.04) and waist circumference>94 cm (male) and >98 cm (female)] significantly predicted prevalent diabetic neuropathy and nephropathy. A BMI of >25.7 kg/m2 had a sensitivity of 55.2% (AUC 0.57), p<0.001 for predicting foot complications.
Conclusion
There is a strong association of obesity and longer diabetes duration with the prevalent microvascular and foot complications irrespective of the glycemic control but not for macrovascular complications.

Similar content being viewed by others
References
International Diabetes Federation.. IDF Diabetes Atlas. 9th ed. Brussels, Belgium: International Diabetes Federation; 2019.
Tandon N, Anjana RM, Mohan V, Kaur T, Afshin A, Ong K, et al. The increasing burden of diabetes and variations among the states of India: the Global Burden of Disease Study 1990–2016. Lancet Glob Health. 2018;6(12):e1352-62.
Bansode B, Jungari DS. Economic burden of diabetic patients in India: a review. Diabetes Metab Syndr. 2019;13(4):2469–72.
Rastogi A, Bhansali A. Diabetic foot infection: an Indian scenario. J Foot Ankle Surg (Asia-Pacific). 2016;3(2):71–9.
Rastogi A, Goyal G, Kesavan R, Bal A, Kumar H, Mangalanadanam, et al. Long term outcomes after incident diabetic foot ulcer: multicenter large cohort prospective study (EDI-FOCUS investigators) epidemiology of diabetic foot complications study epidemiology of diabetic foot complications study. Diabetes Res Clin Pract. 2020;162:108113. https://doi.org/10.1016/j.diabres.2020.108113.
Chaudhary S, Bhansali A, Rastogi A. Mortality in Asian Indians with Charcot’s neuroarthropathy: a nested cohort prospective study. Acta Diabetol. 2019;56:1259–64.
Chawla A, Chawla R, Bhasin GK, Soota K. Profile of adolescent diabetics in North Indian population. J Clin Diabetol. 2014;1:1–3.
UK Prospective Diabetes Study Group. Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837–53.
The DCCT Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86.
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin epidemiologic study of diabetic retinopathy. III. Prevalence and risk of diabetic retinopathy when age at diagnosis is 30 or more years. Arch Ophthalmol. 1984;102(4):527–32.
Levin SR, Coburn JW, Abraira C, Henderson WG, Colwell JA, Emanuele NV, et al. Effect of intensive glycemic control on microalbuminuria in type 2 diabetes. Veterans Affairs Cooperative Study on Glycemic Control and Complications in Type 2 Diabetes Feasibility Trial Investigators. Diabetes Care. 2000;23(10):1478–85.
Rao PV, Makkar BM, Kumar A, et al. RSSDI consensus on self-monitoring of blood glucose in types 1 and 2 diabetes mellitus in India. Int J Diabetes Dev Ctries. 2018;38:260–79.
American Diabetes Association. Standards of medical care in Diabetes—2018. Diabetes Care. 2018;41(Supplement 1):S13-27.
Unnikrishnan R, Anjana RM, Deepa M, Pradeepa R, Joshi SR, Bhansali A, et al. ICMR–INDIAB Collaborative Study Group. Glycemic control among individuals with self-reported diabetes in India–the ICMR-INDIAB Study. Diabetes Technol Ther. 2014;16(9):596–603.
Borgharkar SS, Das SS. Real-world evidence of glycemic control among patients with type 2 diabetes mellitus in India: the TIGHT study. BMJ Open Diab Res Care. 2019;7:e000654.
Mohan V, Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of type 2 diabetes: Indian scenario. Indian J Med Res. 2007;125(3):217–30.
Neel JV. The “Thrifty Genotype” in 19981. Nutr Rev. 2009;57(5):2–9.
Misra A, Khurana L. Obesity-related non-communicable diseases: South Asians vs White Caucasians. Int J Obes. 2011;35(2):167–87.
Rema M, Premkumar S, Anitha B, Deepa R, Pradeepa R, Mohan V. Prevalence of diabetic retinopathy in urban India: The Chennai Urban Rural Epidemiology Study (CURES) eye study I. Invest Ophthalmol Vis Sci. 2005;46:2328–33.
Raman R, Rani PK, ReddiRachepalle S, Gnanamoorthy P, Uthra S, Kumaramanickavel G, et al. Prevalence of diabetic retinopathy in India: Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetics Study report 2. Ophthalmology. 2009;116:311–8.
Raman R, Ganesan S, Pal SS, Kulothungan V, Sharma T. Prevalence and risk factors for diabetic retinopathy in rural India. Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetic Study III (SN-DREAMS III) report no 2. BMJ Open Diabetes Res Care. 2014;2:e000005.
Nirmalan PK, Tielsch JM, Katz J, Thulasiraj RD, Krishnadas R, Ramakrishnan R, et al. Relationship between vision impairment and eye disease to vision-specific quality of life and function in rural India: The Aravind Comprehensive Eye Survey. Invest Ophthalmol Vis Sci. 2005;46:2308–12.
Ramachandran A, Snehalatha C, Satyavani K, Latha E, Sasikala R, Vijay V. Prevalence of vascular complications and their risk factors in type 2 diabetes. J Assoc Physicians India. 1999;47(12):1152–6.
Chawla A, Chawla R, Chawla A. Correlation between retinopathy microalbuminuria and other modifiable risk factors. Presented on American Diabetes Association’s 75th Scientific Session; June 5-9; Boston, Massachusetts; 2015.
Agrawal R, Ola V, Bishnoi P, Gothwal S, Sirohi P, Agrawal R. Prevalence of micro and macrovascular complications and their risk factors in type-2 diabetes mellitus. J Assoc Physicians India. 2014;62:6.
Kosiborod M, Gomes MB, Nicolucci A, Pocock S, Rathmann W, Shestakova M, et al. Vascular complications in patients with type 2 diabetes: prevalence and associated factors in 38 countries (the DISCOVER study program). Cardiovasc Diabetol. 2018;17(1):150.
Shobhana R, Ramarao P, Lavanya A, Vijay VV, Ramchandran A. Cost burden to diabetic patients with foot complications – a study from Southern India. JAPI. 2000;48:1147–50.
Stern MP. Diabetes and cardiovascular disease the “common soil” hypothesis. Diabetes Cardiovasc Dis. 1995;44:6.
Matheus AS, Gomes MB. Early aggressive macrovascular disease and type 1 diabetes mellitus without chronic complications: a case report. BMC Res Notes. 2013;6:22.
Bus SA, van Netten JJ, Lavery LA, Monteiro-Soares M, Rasmussen A, Jubiz Y, Price PE. International Working Group on the Diabetic Foot. IWGDF guidance on the prevention of foot ulcers in at-risk patients with diabetes. Diabetes Metab Res Rev. 2016;32(Suppl 1):16–24. https://doi.org/10.1002/dmrr.2696.
Vibha SP, Kulkarni MM, Kirthinath Ballala AB, Kamath A, Maiya GA. Community based study to assess the prevalence of diabetic foot syndrome and associated risk factors among people with diabetes mellitus. BMC Endocr Disord. 2018;18(1):43. https://doi.org/10.1186/s12902-018-0270-2.
Acknowledgments
We thank Ms Persis and Ms Reshma for data acquisition and entry.
Funding
This study has been funded by ICMR research grant number 5/4/5-7/Diab.16-NCD-II.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
The study was approved by Institute Ethics Committee vide letter No: PGI/IEC/2014/2341 and a written informed consent was obtained from all the participants. The patients were enrolled during their routine physical appointment in the clinic.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Malhotra, B., Hiteshi, P., Rajput, R. et al. Prevalent vascular complications in people with diabetes: a multicentre observational cohort study. Int J Diabetes Dev Ctries 42, 495–504 (2022). https://doi.org/10.1007/s13410-021-01010-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-021-01010-x