Abstract
Background
There is a huge burden of diabetes-related complications, both microvascular and macrovascular, in India. With the rising prevalence of diabetes mellitus (DM), this translates to an increasing number of people with complications of DM. Diabetic peripheral neuropathy (DPN) is the most common complication among DM patients with a prevalence ranging from 18.8 to 61.9% in India. Early diagnosis of DPN can reduce associated complications. Screening services at the primary healthcare level can aid early diagnosis of complications and improve health outcomes among DM patients. This study aimed to assess the prevalence of DPN and its risk factors among the type 2 DM patients attending a rural health centre.
Methodology
A cross-sectional study was conducted among 390 type 2 DM patients attending the Rural Health and Training Centre of Sri Ramachandra Medical College & Research Institute. Data was collected using a standardized questionnaire followed by general inspection and physical examination of the feet. Blood sample was taken to estimate HbA1c and urine sample was collected to detect presence of albumin.
Results
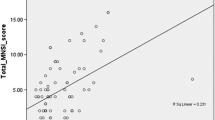
Among the 390 participants, 175 (44.9%) had neuropathy of which 87 (51.5%) were symptomatic. Educational status of primary schooling and less (OR = 3.34; p < 0.001), duration of DM (OR = 1.73; p = 0.038), higher HbA1c levels (OR = 2.87; p = 0.018), presence of urine albumin (OR = 2.57; p = 0.033) and peripheral vascular disease (OR = 2.85; p < 0.001) were predictors for DPN.
Conclusion
The present study shows that the prevalence of peripheral neuropathy is high in rural areas. Regular screening using simple clinical bedside methods and affordable tools can help early identification of DPN and prevent complications like foot ulcer which ultimately leads to amputation.

Similar content being viewed by others
Change history
11 February 2021
A Correction to this paper has been published: https://doi.org/10.1007/s13410-021-00925-9
References
Research E, Atlas I. IDF Diabetes Atlas. Idf.org. 2019 [cited 2019 Aug 8]. Available from: https://www.idf.org/e-library/epidemiology-research/diabetes-atlas/134-idf-diabetes-atlas-8th-edition.html.
Anjana M, Pradeepa R, Guha R, Deepa R, Mohan D, et al. Prevalence of diabetes and pre-diabetes in urban and rural India. Phase 1 results of the Indian Council of Medical Research – India DIABetes (ICMR-INDIAB) study. Diabetologia. 54:3022–7. https://doi.org/10.1007/s00125-011-2291-5.
Shashank RJ. Diabetes care in India. Ann Glob Health. 2015;81(6):830–8.
Pradeepa R, Rema M, Vignesh J, Deepa M, Deepa R, Mohan V. Prevalence and risk factors for diabetic neuropathy in an urban south Indian population: the Chennai Urban Rural Epidemiology Study (CURES-55). Diabet Med. 2008;25:407–12. https://doi.org/10.1111/j.1464-5491.2008.02397.
Mohan V, Deepa R, Shanthirani S, Rema M. Prevalence of microalbuminuria in a selected South Indian population - the Chennai Urban Population Study (CUPS). Diabetes Res Clin Pract. 2000;50:261.
Ramachandran A, Chamukuttan S, Viswanathan V. Burden of type 2 diabetes and its complications-The Indian scenario. Diab Res. 2001;83.
Mohan V, Shah S, Saboo B. Current glycemic status and diabetes related complications among type 2 diabetes patients in India: data from the A1chieve study. J Assoc Physicians India. 2013;61(1 Suppl):12–5.
Tesfaye S, Boulton AJ, Dyck PJ, et al. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments [published correction appears in Diabetes Care. 2010 Dec;33(12):2725]. Diabetes Care. 2010;33(10):2285–93. https://doi.org/10.2337/dc10-1303.
Young MJ, Boulton AJ, MacLeod AF, Williams DR, Sonksen PH. A multicentre study of the prevalence of diabetic peripheral neuropathy in the United Kingdom hospital clinic population. Diabetologia. 1993;36(2):150–4. https://doi.org/10.1007/BF00400697.
Rani P, Raman R, Rachapalli S, Pal S, Kulothungan V, et al. Prevalence and risk factors for severity of diabetic neuropathy in type 2 diabetes mellitus. Indian J Med Sci; Mumbai. 2010;64(2):51–7. https://doi.org/10.4103/0019-5359.94400.
Ashok S, Ramu M, Deepa R, Mohan V. Prevalence of neuropathy in type 2 diabetic patients attending a diabetes centre in South India. J Assoc Physicians India. 2002;50:546–50.
Agrawal RP, Ola V, Bishnoi P, Gothwal S, Sirohi P, Agrawal R. Prevalence of micro and macrovascular complications and their risk factors in type-2 diabetes mellitus. J Assoc Physicians India. 2014;62(6):504–8.
Boulton AJM, Vinik AI, Arezzo JC, Bril V, Feldman EL, Freeman R, et al. Diabetic Neuropathies. Diabetes Care. 2005;28(4):956–62. https://doi.org/10.2337/diacare.28.4.956.
Begum S, Venkatesan M, Ganapathy K. Foot care practices, its barriers and risk for peripheral neuropathy among diabetic patients attending medical college in rural Puducherry. Int J Commun Med Publ Health. [S.l.], 2018;6(1)203–207. ISSN 2394-6040. https://doi.org/10.18203/2394-6040.ijcmph20185243. Available at: https://www.ijcmph.com/index.php/ijcmph/article/view/3747.
World Health Organization. https://www.who.int/dietphysicalactivity/media/en/gsfs_obesity.pdf. Published 2020. Accessed 29 Aug 2020.
WHO Expert Consultation Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163.
WHO technical specifications for automated non-invasive blood pressure measuring devices with cuff. Geneva: World Health Organization; 2020.
de Boer IH, Bangalore S, Benetos A, Davis AM, Michos ED, Muntner P, et al. Diabetes and hypertension: a position statement by the American Diabetes Association. Diab Care. 2017;40(9):1273–84. https://doi.org/10.2337/dci17-0026.
Boyko EJ, Ahroni JH, Cohen V, Nelson KM, Heagerty PJ. Prediction of diabetic foot ulcer occurrence using commonly available clinical information: the Seattle Diabetic Foot Study. Diabetes Care. 2006;29:1202–7.
Mayfield JA, Reiber GE, Sanders LJ, Janisse D, Pogach LM. American Diabetes Association. Preventive foot care in people with diabetes. Diabetes Care. 2003;26(Suppl 1):S78–9. https://doi.org/10.2337/diacare.26.2007.s78.
Mayfield JA, Sugarman JR. The use of the Semmes-Weinstein monofilament and other threshold tests for preventing foot ulceration and amputation in persons with diabetes. J Fam Pract. 2002;49(Suppl. 11):S17–29.
Young MJ, Breddy JL, Veves A, Boulton AJ. The prediction of diabetic neuropathic foot ulceration using vibration perception thresholds: a prospective study. Diabetes Care. 1994;17:557–60.
Boulton AJM, Armstrong DG, Albert SF, Frykberg RG, Hellman R, Kirkman MS, et al. Comprehensive foot examination and risk assessment. Diabetes Care. 2008;31(8):1679–85. https://doi.org/10.2337/dc08-9021.
Armstrong DG, Lavery LA, Vela SA, Quebedeaux TL, Fleischli JG. Choosing a practical screening instrument to identify patients at risk for diabetic foot ulceration. Arch Intern Med. 1998;158:289–92.
Aina blood monitoring system. Analytical performance summary. http://www.janacare.com/assets/pdf/LBL-AINA-13_C.pdf. Accessed 29 Aug 2020
Michigan Diabetes Research & Training Center. Hemoglobin A1c fact sheet. Available from http://diabetesresearch.med.umich.edu/Core_MDRC_Clinical_Hemoglobin.php. Published 2020. Accessed 22 August 2020.
American Diabetes Association. 6. Glycemic Targets: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S66-S76. https://doi.org/10.2337/dc20-S006.
George H, Rakesh P, Krishna M, et al. Foot care knowledge and practices and the prevalence of peripheral neuropathy among people with diabetes attending a secondary care rural hospital in southern India. J Family Med Prim Care. 2013;2(1):27–32. https://doi.org/10.4103/2249-4863.109938.
Surendra D, Khadervali N, Khan PS, Bayapa RN, Sravana DC, Sekhar CC. Prevalence and its associated determinants of diabetic peripheral neuropathy (DPN) in individuals having type-2 diabetes mellitus in Rural South India. Indian J Community Med. 2019;44(2):88–91.
Gill HK, Yadav SB, Ramesh V, Bhatia E. A prospective study of prevalence and association of peripheral neuropathy in Indian patients with newly diagnosed type 2 diabetes mellitus. J Postgrad Med. 2014;60(3):270–5. https://doi.org/10.4103/0022-3859.138750.
Bansal D, Gudala K, Muthyala H, Esam HP, Nayakallu R, Bhansali A. Prevalence and risk factors of development of peripheral diabetic neuropathy in type 2 diabetes mellitus in a tertiary care setting. J Diabetes Investig. 2014;5:714–21.
Cabezas-Cerrato J. The Neuropathy Spanish Study Group of the Spanish Diabetes Society (SDS). Diabetologia. 1998;41:1263. https://doi.org/10.1007/s001250051063.
Javed A, Furqan A, Zaheer M, Kasuri N. Gender based differences in diabetic peripheral neuropathy. Pak J Neurol Sci (PJNS). 2014;9(4):6. Available at: http://ecommons.aku.edu/pjns/vol9/iss4/6.
Gogia S, Rao CR. Prevalence and risk factors for peripheral neuropathy among type 2 diabetes mellitus patients at a tertiary care hospital in coastal Karnataka. Indian J Endocr Metab. 2017;21:665–9.
Al-Maskari F, El-Sadig M. Prevalence of risk factors for diabetic foot complications. BMC Fam Pract. 2007;8:59. https://doi.org/10.1186/1471-2296-8-59.
D'Souza M, Kulkarni V, Bhaskaran U, et al. Diabetic peripheral neuropathy and its determinants among patients attending a tertiary health care centre in Mangalore, India. J Public Health Res. 2015;4(2):450. Published 2015 Jul 30. https://doi.org/10.4081/jphr.2015.450.
Van der Meer JB, Mackenbach JP. The care and course of diabetes: differences according to level of education. Health Policy. 1999;46(2):127–41.
Sharma N, Sharma SK, Maheshwari VD, Sharma KK, Gupta R. Association of low educational status with microvascular complications in type 2 diabetes: Jaipur diabetes registry-1. Indian J Endocrinol Metab. 2015;19(5):667–72. https://doi.org/10.4103/2230-8210.163206.
Health 2020: Education and health through the life. World Health Organization; 2015. https://www.euro.who.int/__data/assets/pdf_file/0007/324619/Health-2020-Education-and-health-through-the-life-course-en.pdf?ua = 1. Accessed Aug 23 2020.
Liu X, Xu Y, An M, Zeng Q. The risk factors for diabetic peripheral neuropathy: a meta-analysis. PLoS One. 2019;14(2):e0212574. https://doi.org/10.1371/journal.pone.0212574.
Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, et al., editors. 16th ed. Vol II. New York: McGraw Hill, Medical Publishing Division; 1998. Harrison’s principles of internal medicine, pp. 2161–63.
Ishibashi F, Taniguchi M, Kosaka A, Uetake H, Tavakoli M. Improvement in neuropathy outcomes with normalizing HbA1c in patients with type 2 diabetes. Diabetes Care. 2018;dc181560; https://doi.org/10.2337/dc18-156
Pfannkuche A, Alhajjar A, Ming A, Walter I, Piehler C, Mertens P. Prevalence and risk factors of diabetic peripheral neuropathy in a diabetics cohort: register initiative “diabetes and nerves”. Endocr Metab Sci. 2020;1(1-2):100053. https://doi.org/10.1016/j.endmts.2020.100053.
Hughes RA. Peripheral neuropathy. BMJ. 2002;324(7335):466–9. https://doi.org/10.1136/bmj.324.7335.466.
Funding
This study was supported by GATE–Young Faculty research grant of Sri Ramachandra Institute of Higher Education and Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethics
This study was performed in line with the principles of the Declaration of Helsinki. The study protocol was approved by Sri Ramachandra Institutional Ethics Committee (Ref: IEC-NI/16/Nov/56/81). Written informed consent was obtained from all study participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The correct order of the Author names is shown in this paper.
Rights and permissions
About this article
Cite this article
Jasmine, A., G.V., A., Durai, V. et al. Prevalence of peripheral neuropathy among type 2 diabetes mellitus patients in a rural health centre in South India. Int J Diabetes Dev Ctries 41, 293–300 (2021). https://doi.org/10.1007/s13410-020-00885-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-020-00885-6