Abstract
Introduction
Type 2 diabetes mellitus (T2DM) is associated with long-term complications in different organs, and this is attributable to macrovascular and microvascular changes as reported by Fowler. Pulmonary complications, however, have been poorly characterised.
Materials and methods
The present study was a case–control study done at SRN Hospital, Prayagraj to correlate the pulmonary functions with glycemic status and insulin resistance in 100 patients with diabetes (cases) and compare these parameters in patients without diabetes (controls). Baseline values of fasting plasma glucose (FPG), prandial plasma glucose (PPG) and glycated hemoglobin (A1C) were significantly increased in cases as compared with controls.
Results
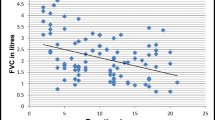
Forced expiratory volume (FEV1) (78.71% compared with 88.15%) and forced vital capacity (FVC) (67.48% compared with 96.58%) were both decreased in cases compared with controls but as decline in FVC was more compared with FEV1; their ratio, FEV1/FVC (121.70 as compared to 90.19), was increased in cases. FVC decreased with increase in A1C values (96.2%, 84.2%, 71.2% for A1C values 5.7%, 5.7–6.4% and > 6.4% respectively). FVC was also decreased for greater values of Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) (98.2% for HOMA-IR < 2.5 and 74.6% for HOMA-IR > 2.5). The ratio of FEV1/FVC was more with higher values of A1C (103.3 for A1C > 2.5 and 91.1 for A1C < 2.5). FVC also decreased with increasing values of FPG (97.4%, 91.1% and 71.2% for FPG values of < 100 mg%, 100–125 mg% and ≥ 126 mg%).
Conclusion
A total of 65% of patients had abnormal pulmonary function tests with predominance of restrictive pattern. This restrictive decline is significantly associated with increasing dysglycemia and insulin resistance. However, it is unrelated to levels of low-density lipoprotein (LDL) and duration of T2DM.



Similar content being viewed by others
References
Fowler MJ. Microvascular and macrovascular complications of diabetes. Clinical Diabetes. 2008;26(2):77–82.
Yadav A, Saxena AK, Gaur K, Punjabi P, Meena G. Study of pulmonary function test in type 2 diabetes mellitus. IOSR-JDMS.2013;10(2) :74–7.
Irfan M, Jabbar A, Haque AS, Awan S, Hussain SF. Pulmonary functions in patients with diabetes mellitus. Lung India. 2011;28(2):89–92.
Agarwal AS, Fuladi AB, Mishra G, Tayade BO. Spirometry and diffusion studies in patients with type 2 diabetes mellitus and their association with microvascular complications. Indian J Chest Dis Allied Sci. 2010;52:213–6.
Meo A, et al. Effect of duration of disease on ventilator function in an ethnic Saudi group of diabetic patients. J Diabetes Sci Technol. 2007 Sep;1(5):711–7.
Davis, W., Knuiman, M., Kendall, P.,Grange, V., & Davis, T. (2004). Glycemic exposure is associated with reduced pulmonary function in type 2 diabetes: the Fremantle Diabetes Study. Diabetes care.2004; 27(3): 752-7.
Shah S, Sonawane P, Nahar P, Vaidya S et al. PFTs in type 2 diabetes mellitus and their association with glycemic control and duration of the disease. Lung India2013;30(2):108–112.
Lee et al. Association between HOMA-IR and lung function in Korean young adults based on the Korea National Health and Nutrition Examination Survey. Sci Rep.2017;7:117–26.
Lawlor DA, Ebrahim S, Smith GD. Associations of measures of lung function with insulin resistance and type 2 diabetes : findings from the British Women's Heart and Health Study. Diabetologia 2004;(47):195–203.
Lazarus R, Sparrow D, Weiss ST. Impaired ventilator function and elevated insulin levels in non diabetic males: the normative ageing study. Eur Respir J. 1998;12:635–40.
Timothy ME, Knuimann M, Kendall P. Reduced pulmonary function and its association in type 2 diabetes. Diabetes Res Clin Pract. 2000;50:152–9.
Kanyakumari DH, Nataraj SM, Devaraj HS. Correlation of duration of diabetes and pulmonary function tests in type 2 diabetes mellitus patients. Int J Biol Med Res. 2011;2(4):1168–70.
Acknowledgments
The authors convey their gratitude to Research Society for Studies of Diabetes in India (RSSDI) for funding the project and to the technical staff of hospital laboratory.
Funding
The study was funded by Research Society for Studies of Diabetes in India (RSSDI).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
An informed consent was obtained from all included subjects after explaining them the nature and purpose of the study. All procedures performed in the study were in accordance with the ethical committee of the institution, and a prior consent for the same was obtained.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bajaj, S., Anil, S. & Prajapati, R. Pulmonary function tests in type 2 diabetes mellitus and their association with glycemic status and insulin resistance. Int J Diabetes Dev Ctries 40, 406–409 (2020). https://doi.org/10.1007/s13410-020-00795-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-020-00795-7