Abstract
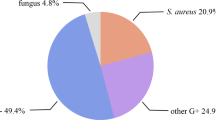
Staphylococcus aureus is one of the most common bacterial pathogens isolated from diabetic foot infections (DFIs). The increasing prevalence of meticillin-resistant S. aureus (MRSA) in patients with diabetes is associated with complications. The aim of this study was to determine the prevalence of S. aureus in DFIs and antibiotic susceptibility patterns of MRSA and non-MRSA isolates. Identification of S. aureus and MRSA was performed by the phenotypic and molecular methods. The Kirby-Bauer and agar dilution methods were performed for determination of antibiotic susceptibility patterns. Thirty-four isolates of S. aureus were isolated from March 2014 to February 2015. The rate of MRSA was 38.23 % according to the disk cefoxitin and oxacillin agar dilution methods, and as by PCR method 12) 35.29 %), isolates were found to have the mecA gene. All MRSA and non-MRSA isolates were susceptible to linezolid and vancomycin. The resistance rate to ceftriaxone was high followed by amoxicillin-clavulanic acid, tetracycline, gentamicin, and erythromycin. The most common bacterial pathogen isolated from DFIs was S. aureus. To ensure effective treatment, accurate detection of MRSA is critical. Our findings showed that MRSA isolates had high-level resistance to antimicrobial agents and that appropriate antibiotic therapy, based on the antibiotic susceptibility pattern, is essential to ensure a good result.

Similar content being viewed by others
References
Ako-Nai A, Ikem I, Akinloye O, Aboderin A, Ikem R, Kassim O. Characterization of bacterial isolates from diabetic foot infections in Ile-Ife, Southwestern Nigeria. Foot. 2006;16(3):158–64.
Roberts AD, Simon GL. Diabetic foot infections: the role of microbiology and antibiotic treatment. Semin Vasc Surg. 2012;25(2):75–81.
Shankar E, Mohan V, Premalatha G, Srinivasan R, Usha A. Bacterial etiology of diabetic foot infections in South India. Eur J Int Med. 2005;16(8):567–70.
Zubair M, Malik A, Ahmad J. Clinico-microbiological study and antimicrobial drug resistance profile of diabetic foot infections in North India. Foot. 2011;21(1):6–14.
Gadepalli R, Dhawan B, Sreenivas V, Kapil A, Ammini A, Chaudhry R. A clinico-microbiological study of diabetic foot ulcers in an Indian tertiary care hospital. Diabetes Care. 2006;29(8):1727–32.
Akhi MT, Ghotaslou R, Asgharzadeh M, Varshochi M, Pirzadeh T, Memar MY, et al. Bacterial etiology and antibiotic susceptibility pattern of diabetic foot infections in Tabriz, Iran. GMS Hyg Infect Control. 2015;10:1–6.
Tentolouris N, Petrikkos G, Vallianou N, Zachos C, Daikos G, Tsapogas P, et al. Prevalence of methicillin-resistant Staphylococcus aureus in infected and uninfected diabetic foot ulcers. Clin Microbiol Infect. 2006;12(2):186–9.
Mohammadi S, Sekawi Z, Monjezi A, Maleki M-H, Soroush S, Sadeghifard N, et al. Emergence of SCCmec type III with variable antimicrobial resistance profiles and spa types among methicillin-resistant Staphylococcus aureus isolated from healthcare- and community-acquired infections in the west of Iran. Int J Infect Dis. 2014;25:152–8.
Sobhy N, Aly F, El Kader OA, Ghazal A, Elbaradei A. Community-acquired methicillin-resistant Staphylococcus aureus from skin and soft tissue infections (in a sample of Egyptian population): analysis of mec gene and staphylococcal cassette chromosome. Braz J Infect Dis. 2012;16(5):426–31.
Hiramatsu K, Cui L, Kuroda M, Ito T. The emergence and evolution of methicillin-resistant Staphylococcus aureus. Trends Microbiol. 2001;9(10):486–93.
Zenelaj B, Bouvet C, Lipsky BA, Uçkay I. Do diabetic foot infections with methicillin-resistant staphylococcus aureus differ from those with other pathogens? Int J Lower Extrem Wounds. 2014;13(4):263–72. doi:10.1177/1534734614550311.
Dang C, Prasad Y, Boulton A, Jude E. Methicillin-resistant Staphylococcus aureus in the diabetic foot clinic: a worsening problem. Diabet Med. 2003;20(2):159–61.
Taha AB. Relationship and susceptibility profile of Staphylococcus aureus infection diabetic foot ulcers with Staphylococcus aureus nasal carriage. Foot. 2013;23(1):11–6.
Araj G, Talhouk R, Simaan C, Maasad M. Discrepancies between mecA PCR and conventional tests used for detection of methicillin resistant Staphylococcus aureus. Int J Antimicrob Agents. 1999;11(1):47–52.
Hasan MR, Brunstein JD, Al-Rawahi G, Tan R, Thomas E, Tilley P. Optimal use of MRSASelect and PCR to maximize sensitivity and specificity of MRSA detection. Curr Microbiol. 2013;66(1):61–3.
Bode LG, van Wunnik P, Vaessen N, Savelkoul PH, Smeets LC. Rapid detection of methicillin-resistant Staphylococcus aureus in screening samples by relative quantification between the mecA gene and the SA442 gene. J Microbiol Methods. 2012;89(2):129–32.
Akhi MT, Ghotaslou R, Beheshtirouy S, Asgharzadeh M, Pirzadeh T, Asghari B, et al. Antibiotic susceptibility pattern of aerobic and anaerobic bacteria isolated from surgical site infection of hospitalized patients. Jundishapur J Microbiol. 2015;8(7):e20309. doi:10.5812/jjm.20309v2.
Mahon CR, Lehman DC. Manuselis Jr G. Elsevier Health Sciences: Textbook of diagnostic microbiology. Philadelphia: Saunders; 2014.
Sadeghi J, Mansouri S. Molecular characterization and antibiotic resistance of clinical isolates of methicillin-resistant Staphylococcus aureus obtained from Southeast of Iran (Kerman). APMIS. 2014;122(5):405–11.
Wayne P. Clinical and Laboratory Standards Institute. Pennsylvania: Clinical and Laboratory Standards Institute Performance Standards for Antimicrobial Susceptibility Testing; 2011. p. 21.
Asgharzadeh M, Kafil HS, Khakpour M. Comparison of mycobacterial interspersed repetitive unit-variable number tandem repeat and IS6110-RFLP methods in identifying epidemiological links in patients with tuberculosis in Northwest of Iran. Ann Microbiol. 2008;58(2):333–9.
Pappu AK, Sinha A, Johnson A. Microbiological profile of diabetic foot ulcer. Calicut Med J. 2011;9(3):e2.
Kandemir Ö, Akbay E, Şahin E, Milcan A, Gen R. Risk factors for infection of the diabetic foot with multi-antibiotic resistant microorganisms. J Infect. 2007;54(5):439–45.
Mendes J, Marques-Costa A, Vilela C, Neves J, Candeias N, Cavaco-Silva P, et al. Clinical and bacteriological survey of diabetic foot infections in Lisbon. Diabet Res Clin Pract. 2012;95(1):153–61.
Benwan KA, Mulla AA, Rotimi VO. A study of the microbiology of diabetic foot infections in a teaching hospital in Kuwait. J Infect Public Health. 2012;5(1):1–8.
Raja NS. Microbiology of diabetic foot infections in a teaching hospital in Malaysia: a retrospective study of 194 cases. J Microbiol Immunol Infect. 2007;40(1):39.
Shanmugam P, Jeya M. The bacteriology of diabetic foot ulcers, with a special reference to multidrug resistant strains. J Clin Diagn Res: JCDR. 2013;7(3):441.
Perez LRR, Dias C, d’Azevedo PA. Agar dilution and agar screen with cefoxitin and oxacillin: what is known and what is unknown in detection of meticillin-resistant Staphylococcus aureus. J Med Microbiol. 2008;57(8):954–6.
Palazzo ICV, Rehder A, Darini ALC. Quantitative disk diffusion as a convenient method for determining minimum inhibitory concentrations of oxacillin for staphylococci strains. J Microbiol Methods. 2007;71(3):186–90.
Hartemann-Heurtier A, Robert J, Jacqueminet S, Ha Van G, Golmard J, Jarlier V, et al. Diabetic foot ulcer and multidrug-resistant organisms: risk factors and impact. Diabetic Med. 2004;21(7):710–5.
Eleftheriadou I, Tentolouris N, Argiana V, Jude E, Boulton AJ. Methicillin-resistant Staphylococcus aureus in diabetic foot infections. Drugs. 2010;70(14):1785–97.
Armstrong DG, Lipsky BA. Diabetic foot infections: stepwise medical and surgical management. Int Wound J. 2004;1(2):123–32.
Tentolouris N, Jude E, Smirnof I, Knowles E, Boulton A. Methicillin-resistant Staphylococcus aureus: an increasing problem in a diabetic foot clinic. Diabetic Med. 1999;16(9):767–71.
Bader MS. Diabetic foot infection. Am Fam Physician. 2008;78(1):71–9.
Cervantes-García E, García-González R, Reséndiz-Albor A, Salazar-Schettino PM. Infections of diabetic foot ulcers with methicillin-resistant Staphylococcus aureus. Int J Lower Extrem Wounds. 2015;14(1):44–9.
Acknowledgments
This research was supported by a grant from Infectious and Tropical Disease Research Center of Tabriz University of Medical Sciences (TUMS), and the manuscript was written based on a dataset of the M.Sc. thesis of Naser Alizadeh registered at Tabriz University of Medical Sciences (Number: 11017-May 2014). The authors would like to thank the staff of Imam Reza and Sina infectious disease wards and microbiology department for their help.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by The Ethic Commission of Tabriz University of Medical Sciences (Number: 5/4/589 -23 Mar. 2014).
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional.
Grant
This research was supported by a grant from Research center of infectious and tropical disease of Tabriz University of Medical sciences.
Rights and permissions
About this article
Cite this article
Akhi, M.T., Ghotaslou, R., Memar, M.Y. et al. Frequency of MRSA in diabetic foot infections. Int J Diabetes Dev Ctries 37, 58–62 (2017). https://doi.org/10.1007/s13410-016-0492-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-016-0492-7