Abstract
Purpose
Loss of a cytostatic response to TGF-β has been implicated in multiple hyper-proliferative disorders, including cancer. Although several key genes involved in the cytostatic activity of TGF-β have in the past been identified, its exact mode of action is yet to be elucidated. A comprehensive understanding of the mechanisms underlying the cytostatic activity of TGF-β may open up new avenues for the development of therapeutic strategies.
Methods
Quantitative real-time RT-PCR was used to assess osteopontin (OPN) gene expression in human hepatoma-derived Huh-7 and lung adenocarcinoma-derived A549 cells. Reporter assays using an OPN promoter-luciferase construct and its mutated counterparts were performed to assess its transcriptional activity. Binding of Smad4 to the OPN gene promoter was investigated using chromatin immunoprecipitation (CHIP). The putative role of Smad4 in OPN gene expression down-regulation was also assessed using a shRNA-mediated knockdown strategy. The anti-proliferative effect of TGF-β on different cancer-derived cell lines was determined using the cell proliferation reagent WST-1.
Results
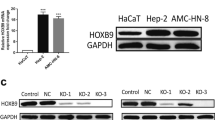
We found that the OPN expression levels dose-dependently decreased in TGF-β-treated Huh-7 and A549 cells. Our reporter assays indicated that this TGF-β-induced repression occurred at the transcriptional level, and could largely be abrogated by disruption of an element (TIE2) similar to the TGF-β inhibitory element found in other TGF-β-repressed genes. Our CHIP assay revealed that the Smad protein complex specifically binds to the OPN gene promoter, and that the TGF-β-mediated inhibition of OPN was lost upon shRNA-mediated knockdown of Smad4. Moreover, we found that the deregulation of OPN gene expression by TGF-β occurred concomitantly with loss of the TGF-β anti-proliferative response, whereas a neutralizing anti-OPN antibody partially restored this response.
Conclusions
Our results indicate that the OPN gene is a direct target of Smad-mediated TGF-β signaling, implying that OPN expression inhibition serves as a novel mechanism underlying the cytostatic activity of TGF-β.




Similar content being viewed by others
References
F. Lebrin, M. Deckers, P. Bertolino, P. ten Dijke, TGF-β receptor function in the endothelium. Cardiovasc. Res. 65, 599–608 (2004)
C.-H. Heldin, M. Landström, A. Moustakas, Mechanism of TGF-β signaling to growth arrest, apoptosis, and epithelial-mesenchymal transition. Curr. Opin. Cell Biol. 21, 166–176 (2009)
E. Meulmeester, P. Ten Dijke, The dynamic roles of TGF-beta in cancer. J. Pathol. 223, 205–218 (2011)
A Maier, A.L. Peille, V. Vuaroqueaux, M. Lahn, Anti-tumor activity of the TGF-β receptor kinase inhibitor galunisertib (LY2157299 monohydrate) in patient-derived tumor xenografts. Cell. Oncol. 38, 131–144 (2015)
S. Ross, C.S. Hill, How the smads regulate transcription. Int. J. Biochem. Cell Biol. 40, 383–408 (2008)
A Moustakas, C.H. Heldin, The regulation of TGFβ signal transduction. Development 136, 3699–3714 (2009)
P.M. Siegel, J. Massagué, Cytostatic and apoptotic actions of TGF-β in homeostasis and cancer. Nat. Rev. Cancer 3, 807–821 (2003)
J. Massagué, TGFβ in cancer. Cell 134, 215–230 (2008)
J. Xu, S. Lamouille, R. Derynck, TGF-β-induced epithelial to mesenchymal transition. Cell Res. 19, 156–172 (2009)
G.J. Hannon, D. Beach, p15INK4B is a potential effector of TGFbeta-induced cell cycle arrest. Nature 371, 257–261 (1994)
M.B. Datto, Y. Li, J.F. Panus, D.J. Howe, Y. Xiong, X.F. Wang, Transforming growth factor beta induces the cyclin-dependent kinase inhibitor p21 throughp53-independent mechanism. Proc. Natl. Acad. Sci. U. S. A. 92, 5545–5549 (1995)
J.M. Scandura, P. Boccuni, J. Massague, S.D. Nimer, Transforming growth factor beta-induced cell cycle arrest of human hematopoietic cells requires p57KIP2 upregulation. Proc. Natl. Acad. Sci. U. S. A. 101, 15231–15236 (2004)
J. Massagué, S.W. Blain, R.S. Lo, TGFβ signaling in growth control, cancer, and heritable disorders. Cell 103, 295–309 (2000)
R. Derynck, R.J. Akhurst, A. Balmain, TGF-β signaling in tumor suppression and cancer progression. Nat. Genet. 29, 117–129 (2001)
L.M. Wakefield, A.B. Roberts, TGF-β signaling: positive and negative effects on tumorigenesis. Curr. Opin. Genet. Dev. 12, 22–29 (2002)
B. Kleuser, D. Malek, R. Gust, H.H. Pertz, H. Potteck, 17-beta-estradiol inhibits transforming growth factor-beta signaling and function in breast cancer cells via activation of extracellular signal-regulated kinase through the G protein-coupled receptor 30. Mol. Pharmacol. 74, 1533–1543 (2008)
S. Gizzo, C. Saccardi, T.S. Patrelli, R. Berretta, G. Capobianco, S. Di Gangi, A. Vacilotto, A. Bertocco, M. Noventa, E. Ancona, D. D’Antona, G.B. Nardelli, Update on raloxifene: mechanism of action, clinical efficacy, adverse effects, and contraindications. Obstet. Gynecol. Surv. 68, 467–481 (2013)
S. Gizzo, M. Noventa, C. Saccardi, P. Litta, D. D’Antona, G.B. Nardelli, Proposal on raloxifene use after prophylactic salpingo-oophorectomy in BRCA1-2: hypothesis and rationale. Eur. J. Cancer Prev. 23, 514–515 (2014)
S. Gizzo, M. Noventa, S. Di Gangi, P. Litta, C. Saccardi, D. D’Antona, G.B. Nardelli, Could in-vitro studies on Ishikawa cell lines explain the endometrial safety of raloxifene? Systematic literature review and starting points for future oncological research. Eur. J. Cancer Prev 24, 497–507 (2015)
L. Levy, C.S. Hill, Alterations in components of the TGF-β superfamily signaling pathways in human cancer. Cytokine Growth Factor Rev. 17, 41–58 (2006)
A.B. Roberts, L.M. Wakefield, The two faces of transforming growth factor beta in carcinogenesis. Proc. Natl. Acad. Sci. U. S. A. 100, 8621–8623 (2003)
C.H. Heldin, M. Vanlandewijck, A. Moustakas, Regulation of EMT by TGFβ in cancer. FEBS Lett. 586, 1959–1970 (2012)
G.F. Weber, The metastasis gene osteopontin: a candidate target for cancer therapy. Biochim. Biophys. Acta 1552, 61–85 (2001)
H. Rangaswami, A. Bulbule, G.C. Kundu, Osteopontin: role in cell signaling and cancer progression. Trends Cell Biol. 16, 79–87 (2006)
N.I. Johnston, V.K. Gunasekharan, A. Ravindranath, C. O’Connell, P.G. Johnston, P.G. El-Tanani, Osteopontin as a target for cancer therapy. Front. Biosci. 13, 4361–4372 (2008)
J.L. Lee, M.J. Wang, P.R. Sudhir, G.D. Chen, C.W. Chi, J.Y. Chen, Osteopontin promotes integrin activation through outside-in and inside-out mechanisms: OPN-CD44V interaction enhances survival in gastrointestinal cancer cells. Cancer Res. 67, 2089–2097 (2007)
A Bellahcène, V. Castronovo, K.U. Ogbureke, L.W. Fisher, N.S. Fedarko, Small integrin-binding ligand N-linked glycoproteins (SIBLINGs): multifunctional proteins in cancer. Nat. Rev. Cancer 8, 212–226 (2008)
D. Coppola, M. Szabo, D. Boulware, P. Muraca, M. Alsarraj, A.F. Chambers, T.J. Yeatman, Correlation of osteopontin protein expression and pathological stage across a wide variety of tumor histologies. Clin. Cancer Res. 10, 184–190 (2004)
M. Higashiyama, T. Ito, E. Tanaka, Y. Shimada, Prognostic significance of osteopon- tin expression in human gastric carcinoma. Ann. Surg. Oncol. 14, 3419–3427 (2007)
P.V. Korita, T. Wakai, Y. Shirai, Y. Matsuda, J. Sakata, X. Cui, Y. Ajioka, K. Hatakeyama, Overexpression of osteopontin independently correlates with vascular invasion and poor prognosis in patients with hepatocellular carcinoma. Hum. Pathol. 39, 1777–1783 (2008)
N. Patani, F. Jouhra, W. Jiang, K. Mokbel, Osteopontin expression profiles predict pathological and clinical outcome in breast cancer. Anticancer Res. 28, 4105–4110 (2008)
G.F. Weber, G.S. Lett, N.C. Haubein, Osteopontin is a marker for cancer aggressiveness and patient survival. Br. J. Cancer 103, 861–869 (2010)
J. Zhang, O. Yamada, Y. Matsushita, H. Chagan-Yasutan, T. Hattori, Transactivation of human osteopontin promoter by human T-cell leukemia virus type 1-encoded tax protein. Leuk. Res. 34, 763–768 (2010)
J. Zhang, O. Yamada, T. Sakamoto, H. Yoshida, T. Iwai, Y. Matsushita, H. Shimamura, H. Araki, K. Shimotohno, Down-regulation of viral replication by adenoviral-mediated expression of siRAN against cellular cofactors for hepatitis C virus. Virology 320, 135–143 (2004)
J. Zhang, O. Yamada, S. Kida, Y. Matsushita, S. Yamaoka, H. Chagan-Yasutan, T. Hattori, Identification of CD44 as a downstream target of noncanonical NF-κB pathway activated by human T-cell leukemia virus type 1-encoded tax protein. Virology 413, 244–252 (2011)
T. Standal, M. Borset, A. Sundan, Role of osteopontin in adhesion, migration, cell survival and bone remodeling. Exp. Oncol. 26, 179–184 (2004)
C.R. Chen, Y. Kang, P.M. Siegel, J. Massagué, E2F4/5 and p107 as smad cofactors linking the TGFbeta receptor to c-myc repression. Cell 110, 19–32 (2002)
Y. Kang, C.R. Chen, J. Massagué, A self-enabling TGFbeta response coupled to stress signaling: smad engages stress response factor ATF3 for Id1 repression in epithelial cells. Mol. Cell 11, 915–926 (2003)
N.G. Denissova, C. Pouponnot, J. Long, D. He, F. Liu, Transforming growth factor -inducible independent binding of SMAD to the Smad7 promoter. Proc. Natl. Acad. Sci. 97, 6397–6402 (2000)
N.T. Liberati, M. Moniwa, A.J. Borton, J.R. Davie, X.F. Wang, An essential role for mad homology domain 1 in the association of Smad3 with histone deacetylase activity. J. Biol. Chem. 276, 22595–22603 (2001)
T. Alliston, L. Choy, P. Ducy, G. Karsenty, R. Derynck, TGF-β-induced repression of CBFA1 by Smad3 decreases cbfa1 and osteocalcin expression and inhibits osteoblast differentiation. EMBO J. 20, 2254–2272 (2001)
J.S. Kang, T. Alliston, R. Delston, R. Derynck, Repression of Runx2 function by TGF-β through recruitment of class II histone deacetylases by Smad3. EMBO J. 24, 2543–2555 (2005)
R. Sakata, S. Minami, Y. Sowa, M. Yoshida, T. Tamaki, Trichostatin a activates the osteopontin gene promoter through AP1 site. Biochem. Biophys. Res. Commun. 315, 959–963 (2004)
D.T. Denhardt, D. Mistretta, A.F. Chambers, S. Krishna, J.F. Porter, S. Raghuram, S.R. Rittling, Transcriptional regulation of osteopontin and the metastatic phenotype evidence for a ras-activated enhancer in the human OPN promoter. Clin. Exp. Metastasis 20, 77–84 (2003)
X. Shi, S. Bai, L. Li, X. Cao, Hoxa-9 represses transforming growth factor-beta- induced osteopontin gene transcription. J. Biol. Chem. 276, 850–855 (2001)
T.G. Hullinger, Q. Pan, H.L. Viswanathan, M.J. Somerman, TGFbeta and BMP-2 activation of the OPN promoter: roles of smad- and hox-binding elements. Exp. Cell Res. 262, 69–74 (2001)
C.H. Heldin, A. Moustakas, Role of smads in TGFβ signaling. Cell Tissue Res. 347, 21–36 (2012)
J. Massagué, TGFβ signalling in context. Nat. Rev. Mol. Cell Biol. 13, 616–630 (2012)
K. Matsuzaki, Smad phospho-isoforms direct context-dependent TGF-β signaling. Cytokine Growth Factor Rev. 24, 385–399 (2013)
D. Padua, X.H. Zhang, Q. Wang, C. Nadal, W.L. Gerald, R.R. Gomis, J. Massagué, TGFbeta primes breast tumors for lung metastasis seeding through angiopoietin-like 4. Cell 133, 66–77 (2008)
S. Gizzo, M. Quaranta, G.B. Nardelli, M. Noventa. Lipophilic Statins as Anticancer Agents: Molecular Targeted Actions and Proposal in Advanced Gynaecological Malignancies. Curr. Drug Targets 16, 1142--1159 (2015)
A. Vitagliano, M. Noventa, S. Gizzo. Emerging evidence regarding statins use as novel endometriosis targeted treatment: real "magic pills" or "trendy" drugs? Some considerations. Eur. J. Obstet. Gynecol. Reprod. Biol. 184, 125-126 (2015)
A. Vitagliano, M. Noventa, M. Quaranta, S. Gizzo. Statins as Targeted "Magical Pills" for the Conservative Treatment of Endometriosis: May Potential Adverse Effects on Female Fertility Represent the "Dark Side of the Same Coin"? A Systematic Review of Literature. Reprod. Sci. (2015). doi:10.1177/1933719115584446
M. Matsuura, T. Suzuki, M. Suzuki, R. Tanaka, E. Ito, T. Saito, Statin-mediated reduction of osteopontin expression induces apoptosis and cell growth arrest in ovarian clear cell carcinoma. Oncol. Rep. 25, 41–47 (2011)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal studies
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Zhang, J., Yamada, O., Kida, S. et al. Down-regulation of osteopontin mediates a novel mechanism underlying the cytostatic activity of TGF-β. Cell Oncol. 39, 119–128 (2016). https://doi.org/10.1007/s13402-015-0257-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-015-0257-1