Abstract
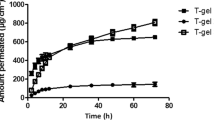
Postoperative pain management is an important aspect of the overall surgical care process. Effective pain management not only provides patient comfort but also promotes faster recovery and reduces the risk of complications. Bupivacaine (BUP) and Lidocaine (LID) transdermal drug deliveries via thermoplastic polyurethane matrix (TPU) and iontophoresis technique are proposed here as alternative routes for postoperative pain instead of the injection route. Under applied electric field, the amounts of BUP and LID released were 95% and 97% from the loaded amounts, which were higher than the passive patch of 40%. The time to equilibrium of BUP turned out to be faster than the time to equilibrium of LID by approximately 1.5 times. This was due to 2 factors namely the drug molecular weight and the drug pKa value; they play an important role in the selection of a suitable drug for fast-acting or long-acting for the postoperative patients. By using this transdermal patch via iontophoresis system, BUP was deemed as the suitable drug for fast-acting due to the shorter time to equilibrium, whereas LID was the suitable drug for long-acting. The in-vitro drug release – permeation study through a porcine skin indicated the efficiency and potential of the system with the amounts of drug permeated up to 76% for BUP and 81% for LID. The TPU transdermal system was demonstrated here as potential to deliver BUP and LID for postoperative patients.
Graphical Abstract








Similar content being viewed by others
Data availability
Data will be available on request to the authors.
References
Horn R, Kramer J. Postoperative Pain Control. In: StatPearls [Internet]. StatPearls Publishing, Treasure Island (FL), PMID: 31335018. 2024. https://pubmed.ncbi.nlm.nih.gov/31335018/. Accessed 9 Jan 2024.
Gupta A, Kaur K, Sharma S, Goyal S, Arora S, Murthy RSR. Clinical aspects of acute post-operative pain management & its assessment. J Adv Pharm Technol Res. 2010;1(2):97–108.
Yue Y, Zhao D, Yin Q. Hyaluronic acid modified nanostructured lipid carriers for transdermal bupivacaine delivery: in vitro and in vivo anesthesia evaluation. Biomed Pharmacother. 2018;98:813–20.
Liu Y, Cheng M, Zhao J, Zhang X, Huang Z, Zang Y, et al. Transdermal delivery of lidocaine-loaded elastic nano-liposomes with microneedle array pretreatment. Biomedicines. 2021;9:592.
Michel-Levy JM. Pharmacokinetics and pharmacodynamics of local anesthetics. Topics in Local Anesthetics. IntechOpen; 2020. pp. 1–16.
Hu J-W, Yen M-W, Wang A-J, Chu I-M. Effect of oil structure on cyclodextrin-based Pickering emulsions for bupivacaine topical application. Colloids Surf B Biointerfaces. 2018;161:51–8.
Xia Y, Chen E, Tibbits DL, Reilley TE, McSweeney TD. Comparison of effects of lidocaine hydrochloride, buffered lidocaine, diphenhydramine, and normal saline after intradermal injection. J Clin Anesth. 2002;14(5):339–43.
Pete DD, D’Souza MS. Chapter 12 - local anesthetics. Side effects of drugs Annual 42. Amsterdam: Elsevier; 2020. pp. 155–63.
Patel D, Chaudhary SA, Parmar B, Bhura N. Transdermal drug delivery system: a review. Pharm Innov. 2012;1(4):66–75.
Alkilani AZ, McCrudden MTC, Donnelly RF. Transdermal drug delivery: innovative pharmaceutical developments based on disruption of the barrier properties of the stratum corneum. Pharmaceutics. 2015;7:438–70.
Ramadon D, McCrudden MTC, Courtenay AJ, Donnelly RF. Enhancement strategies for transdermal drug delivery systems: current trends and applications. Drug Deliv Transl Res. 2022;12:758–91.
Mihalache C, Rata DM, Cadinoiu AN, Patras X, Sindilar EV, Bacaita SE, et al. Bupivacaine-loaded chitosan hydrogels for topical anesthesia in dentistry. Polym Int. 2020;69:1152–60.
Suksaeree J, Maneewattanapinyo P. Ionic liquid drug–based polymeric matrices for transdermal delivery of lidocaine and diclofenac. J Polym Environ. 2020;28:2771–9.
Suksaeeree J, Waiprib R, Pichakorn W. Improving the hydrophilic properties of deproteinized natural rubber latex films for lidocaine transdermal patches by starch blending. J Polym Environ. 2022;30:1574–86.
Maneewattanapinyo P, Yeesamun A, Watthana F, Panrat K, Pichayakorn W, Suksaeree J. Controlled release of lidocaine–diclofenac ionic liquid drug from freeze-thawed gelatin/poly(vinyl alcohol) transdermal patches. AAPS PharmSciTech. 2019;20(322):1–9.
Maneewattanapinyo P, Yeesamun A, Watthana F, Panrat K, Pichayakorn W, Suksaeree J. Transdermal patches of lidocaine/aspirin ionic liquid drug-loaded gelatin/polyvinyl alcohol composite film prepared by freeze-thawed procedure. Acad Bras Cienc. 2020;92(2):e20191073.
Rawat S, Vengurlekar S, Rakesh B, Jain S, Srikarti G. Transdermal Delivery by Iontophoresis. Indian J Pharm Sci. 2008;70(1):5–10.
Seeni RZ, Zheng M, Lio DCS, Wiraja C, Yusoff MFBM, Koh WTY, et al. Targeted delivery of anesthetic agents to bone tissues using conductive microneedles enhanced iontophoresis for painless dental anesthesia. Adv Funct Mater. 2021;31(47):2105686.
Yu L, Liu Y, Sang M. Iontophoresis-assisted pediatric transdermal delivery of ropivacaine to enhance anesthetic effect. Trop J Pharm Res. 2021;20(4):681–6.
Martin DJ, Osman AF, Andriani Y, Edwards GA. 11 - thermoplastic polyurethane (TPU)-based polymer nanocomposites. Advances in Polymer nanocomposites. Cambridge: Woodhead Publishing Series in Composites Science and Engineering; 2012. pp. 321–50.
Claeys B, Vervaeck A, Hillewaere XKD, Possemiers S, Hansen L, de Beer T, et al. Thermoplastic polyurethanes for the manufacturing of highly dosed oral sustained release matrices via hot melt extrusion and injection molding. Eur J Pharm Biopharm. 2015;90:44–52.
Basu A, Farah S, Kunduru KR, Doppalapudi S, Khan W, Domb AJ. 8– polyurethanes for controlled drug delivery. Advances in polyurethane biomaterials. Cambridge: Woodhead Publishing; 2016. pp. 217–46.
Wang H, Liu X, Christiansen DE, Fattahpour S, Wang K, Song H, et al. Thermoplastic polyurethane with controllable degradation and critical anti-fouling properties. Biomater Sci. 2021;9:1381–96.
Mandru M, Bercea M, Gradinaru LM, Ciobanu C, Drobota M, Vlad S, et al. Polyurethane/poly(vinyl alcohol) hydrogels: Preparation, characterization and drug delivery. Eur Polym J. 2019;118:137–45.
Morarad R, Naeowong W, Niamlang S, Sirivat A. Iontophoresis of basal insulin controlled delivery based on thermoplastic polyurethane. J Drug Deliv Sci Technol. 2022;76:103756.
Korsmeyer RW, Gurny R, Doelker E, Buri P, Peppas NA. Mechanisms of solute release from porous hydrophilic polymers. Int J Pharm. 1983;15:25–35.
Higuchi T. Mechanism of sustained-action medication: theoretical analysis of rate of release of solid drugs dispersed in solid matrices. J Pharm Sci. 1963;52(12):1145–9.
Morarad R, Naeowong W, Sirivat A. Iontophoretically controlled insulin delivery via water-soluble conductive polymer PANI:PSS and thermoplastic polyurethane matrix. Drug Deliv Transl Res. 2024;14(1):280–93.
Tong L, Wang X, He X, Nie G, Zhang J, Zhang B, et al. Electrically conductive TPU nanofibrous composite with high stretchability for flexible strain sensor. Nanoscale Res Lett. 2018;13:86.
Mi H, Salick MR, Jing X, Jacques BR, Crone WC, Peng X, et al. Characterization of thermoplastic polyurethane/polylactic acid (TPU/PLA) tissue engineering scaffolds fabricated by microcellular injection molding. Mater Sci Eng C. 2013;33:4767–76.
Oh J, Kim YK, Hwang S-H, Kim H-C, Jung J-H, Jeon C, et al. Synthesis of thermoplastic polyurethanes containing bio-based polyester polyol and their fiber property. Polymers. 2022;14(10):2033.
Zain NM, Ahmad SH, Ahad NA, Ali ES. Influence of isocyanate structures on mechanical performance of aluminum bonded with green polyurethane adhesive. Adv Mater Res. 2014;879:119–27.
Martins ML, Eckert J, Jacobsen H, dos Santos EC, Ignazzi R, de Araujo DR, et al. Raman and Infrared spectroscopies and X-ray diffraction data on bupivacaine and ropivacaine complexed with 2-hydroxypropyl– β– cyclodextrin. Data Br. 2017;15:25–9.
deFD JS, dosS SMD, dasNRF J, M BM, B DF, H W, et al. Antinociceptive effects of bupivacaine and its sulfobutylether-β-cyclodextrin inclusion complex in orofacial pain. Naunyn Schmiedebergs Arch Pharmacol. 2022;395:1405–17.
Kochhar JS, Lim WXS, Zou S, Foo WY, Pan J, Kang L. Microneedle integrated transdermal patch for fast onset and sustained delivery of lidocaine. Mol Pharm. 2013;10:4272–80.
Bahmani S, Khajavi R, Ehsani M, Rahimi MK, Kalaee MR. Transdermal drug delivery system of lidocaine hydrochloride based on dissolving gelatin/sodium carboxymethylcellulose microneedles. AASP Open. 2023;9:7.
Alejo T, Uson L, Landa G, Prieto M, Argón CY, Garcia-Salinas S, et al. Nanogels with high loading of anesthetic nanocrystals for extended duration of sciatic nerve block. ACS Appl Mater Interfaces. 2021;13:17220–35.
Shepherd SD, O’Buckley SC, Harrington JM, Haines LG, Rothrock GD, Johnson LM, et al. A moldable sustained release bupivacaine formulation for tailored treatment of postoperative dental pain. Sci Rep. 2018;8(1):12172.
Lu X, Qu J, Huang J. Mechanical, thermal and rheologicalproperties of hollow glass microsphere filledthermoplastic polyurethane compositesblended by normal vane extruder. Plast Rubber Compos. 2015;44(8):306–13.
Anacleto SS, Borges MMC, de Oliveira HL, Vicente AR, de Figueiredo EC, de Oliveira MAL, et al. Evaluation of physicochemical properties as supporting information on quality control of raw materials and veterinary pharmaceutical formulations. J Pharm Anal. 2018;8:168–75.
Gala U, Chuong MC, Varanasi R, Chauhan H. Characterization and comparison of lidocaine-tetracaine and lidocaine-camphor eutectic mixtures based on their crystallization and hydrogen-bonding abilities. AAPS PharmSciTech. 2015;16(3):528–36.
McMorland GH, Douglas MJ, Jeffery WK, Ross PLE, Axelson JE, Kim JHK, et al. Effect of pH-adjustment of bupivacaine on onset and duration of epidural analgesia in parturients. Can Anaesth Soc J. 1986;33(5):537–41.
Benson HAE. Skin structure, function, and permeation. In: Benson HAE, Watkinson AC, editors. Topical and transdermal drug delivery: principles and practice. New Jersey: John Wiley & Sons, Inc.; 2012. pp. 3–23.
Wang Y, Thakur R, Fan Q, Michniak B. Transdermal iontophoresis: combination strategies to improve transdermal iontophoretic drug delivery. Eur J Pharm Biopharm. 2005;60:179–91.
Zao J, Du L, Li M, Liu B, Zhu W, Jin Y. Transdermal enhancement effect and mechanism of iontophoresis for non-steroidal anti-inflammatory drugs. Int J Pharm. 2014;466(1–2):76–82.
Taylor A, McLeod G. Basic pharmacology of local anaesthetics. BJA Educ. 2020;20(2):34–41.
Lee CR, Kim MS, Lee HB, Lee HK, Rhee JM, Khang G. The effect of molecular weight of drugs on transdermal delivery system using microneedle device. Key Eng Mater. 2007;342–343:945–8.
Pollard JB, Luginbühl ML. High doses of local anaesthetic during spinal anaesthesia may increase the risk of life-threatening vagal reactions. Br J Anaesth. 2003;90(4):525–6.
Dreyer SJ, Beckworth WJ. 2 - commonly used medications in procedures. Pain procedures in clinical practice. Amsterdam: Elsevier; 2011. pp. 5–12.
Scully C. (2014) 3 - Perioperative care. In: Scully’s Medical Problems in Dentistry. London: Churchill Livingstone; 2014. pp. 51–96.
Weibel S, Jokinen J, Pace NL, Schhnabel A, Hollmann MW, Hahnenkamp K, et al. Efficacy and safety of intravenous lidocaine for postoperative analgesia and recovery after surgery: a systematic review with trial sequential analysis. Br J Anaesth. 2016;116(6):770–83.
Acknowledgements
This work was supported by the Petroleum and Petrochemical College, the 100th Anniversary Chulalongkorn University Fund for Doctoral Scholarship, the 90th Anniversary of Chulalongkorn University Scholarship, the Conductive and Electroactive Polymers Research Unit of Chulalongkorn University, the Thailand Science Research and Innovation Fund Chulalongkorn University (TSRI-CU), Health Systems Research Institute (HSRI), and the National Research Council of Thailand (NRCT).
Author information
Authors and Affiliations
Contributions
Rawita Morarad: Methodology, Investigation, Writing - Original Draft; Ketchada Uerpairojkit: Writing - Review & Editing; Pornpan Chalermkitpanit: Writing - Review & Editing; Anuvat Sirivat: Writing - Review & Editing, Supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No animal and human studies have been performed in this research.
Consent for publication
All authors agree to publish this manuscript.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morarad, R., Uerpairojkit, K., Chalermkitpanit, P. et al. Comparative study of iontophoresis-assisted transdermal delivery of bupivacaine and lidocaine as anesthetic drugs. Drug Deliv. and Transl. Res. (2024). https://doi.org/10.1007/s13346-024-01627-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s13346-024-01627-5