Abstract
The cell-surface receptor tyrosine kinase c-mesenchymal-epithelial transition factor (c-Met) is overexpressed in a wide range of solid tumors, making it an appropriate target antigen for the development of anticancer therapeutics. Various antitumor c-Met-targeting therapies (including monoclonal antibodies [mAbs] and tyrosine kinases) have been developed for the treatment of c-Met-overexpressing tumors, most of which have so far failed to enter the clinic because of their efficacy and complications. Antibody–drug conjugates (ADCs), a new emerging class of cancer therapeutic agents that harness the target specificity of mAbs to deliver highly potent small molecules to the tumor with the minimal damage to normal cells, could be an attractive therapeutic approach to circumvent these limitations in patients with c-Met-overexpressing tumors. Of great note, there are currently nine c-Met-targeting ADCs being examined in different phases of clinical studies as well as eight preclinical studies for treating various solid tumors. The purpose of this study is to present a broad overview of clinical- and preclinical-stage c-Met-targeting ADCs.
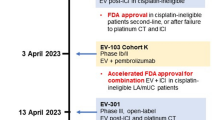
Graphical Abstract




Similar content being viewed by others
Data availability
The data included in this review were retrieved from published studies.
References
Kim KH, Kim H. Progress of antibody-based inhibitors of the HGF-cMET axis in cancer therapy. Exp Mol Med. 2017;49(3): e307.
Tempest PR, Stratton MR, Cooper CS. Structure of the met protein and variation of met protein kinase activity among human tumour cell lines. Br J Cancer. 1988;58(1):3–7.
Gherardi E, Birchmeier W, Birchmeier C, Vande WG. Targeting MET in cancer: rationale and progress. Nat Rev Cancer. 2012;12(2):89–103.
Mo HN, Liu P. Targeting MET in cancer therapy. Chronic Dis Transl Med. 2017;3(3):148–53.
Zhang Y, Xia M, Jin K, Wang S, Wei H, Fan C, et al. Function of the c-Met receptor tyrosine kinase in carcinogenesis and associated therapeutic opportunities. Mol Cancer. 2018;17(1):45.
Donate LE, Gherardi E, Srinivasan N, Sowdhamini R, Aparicio S, Blundell TL. Molecular evolution and domain structure of plasminogen-related growth factors (HGF/SF and HGF1/MSP). Protein Sci. 1994;3(12):2378–94.
Birchmeier C, Birchmeier W, Gherardi E, Vande Woude GF. Met, metastasis, motility and more. Nat Rev Mol Cell Biol. 2003;4(12):915–25.
Zhang Y, Guo L, Li Y, Feng GH, Teng F, Li W, et al. MicroRNA-494 promotes cancer progression and targets adenomatous polyposis coli in colorectal cancer. Mol Cancer. 2018;17(1):1.
Zhang Z, Li D, Yun H, Tong J, Liu W, Chai K, et al. Opportunities and challenges of targeting c-Met in the treatment of digestive tumors. Front Oncol. 2022;12: 923260.
Gu FF, Zhang Y, Liu YY, Hong XH, Liang JY, Tong F, et al. Lung adenocarcinoma harboring concomitant SPTBN1-ALK fusion, c-Met overexpression, and HER-2 amplification with inherent resistance to crizotinib, chemotherapy, and radiotherapy. J Hematol Oncol. 2016;9(1):66.
Christensen JG, Burrows J, Salgia R. c-Met as a target for human cancer and characterization of inhibitors for therapeutic intervention. Cancer Lett. 2005;225(1):1–26.
Nakamura M, Ono YJ, Kanemura M, Tanaka T, Hayashi M, Terai Y, et al. Hepatocyte growth factor secreted by ovarian cancer cells stimulates peritoneal implantation via the mesothelial-mesenchymal transition of the peritoneum. Gynecol Oncol. 2015;139(2):345–54.
Zeng ZS, Weiser MR, Kuntz E, Chen CT, Khan SA, Forslund A, et al. c-Met gene amplification is associated with advanced stage colorectal cancer and liver metastases. Cancer Lett. 2008;265(2):258–69.
Mizuno S, Nakamura T. HGF-MET cascade, a key target for inhibiting cancer metastasis: the impact of NK4 discovery on cancer biology and therapeutics. Int J Mol Sci. 2013;14(1):888–919.
Sattler M, Reddy MM, Hasina R, Gangadhar T, Salgia R. The role of the c-Met pathway in lung cancer and the potential for targeted therapy. Ther Adv Med Oncol. 2011;3(4):171–84.
Blumenschein GR Jr, Mills GB, Gonzalez-Angulo AM. Targeting the hepatocyte growth factor-cMET axis in cancer therapy. J Clin Oncol. 2012;30(26):3287–96.
Li G, Schaider H, Satyamoorthy K, Hanakawa Y, Hashimoto K, Herlyn M. Downregulation of E-cadherin and Desmoglein 1 by autocrine hepatocyte growth factor during melanoma development. Oncogene. 2001;20(56):8125–35.
Koochekpour S, Jeffers M, Rulong S, Taylor G, Klineberg E, Hudson EA, et al. Met and hepatocyte growth factor/scatter factor expression in human gliomas. Cancer Res. 1997;57(23):5391–8.
Ma PC, Jagadeeswaran R, Jagadeesh S, Tretiakova MS, Nallasura V, Fox EA, et al. Functional expression and mutations of c-Met and its therapeutic inhibition with SU11274 and small interfering RNA in non-small cell lung cancer. Cancer Res. 2005;65(4):1479–88.
Spigel DR, Ervin TJ, Ramlau RA, Daniel DB, Goldschmidt JH Jr, Blumenschein GR Jr, et al. Randomized phase II trial of Onartuzumab in combination with erlotinib in patients with advanced non-small-cell lung cancer. J Clin Oncol. 2013;31(32):4105–14.
Fujita S, Sugano K. Expression of c-met proto-oncogene in primary colorectal cancer and liver metastases. Jpn J Clin Oncol. 1997;27(6):378–83.
Resnick MB, Routhier J, Konkin T, Sabo E, Pricolo VE. Epidermal growth factor receptor, c-MET, beta-catenin, and p53 expression as prognostic indicators in stage II colon cancer: a tissue microarray study. Clin Cancer Res. 2004;10(9):3069–75.
Lengyel E, Prechtel D, Resau JH, Gauger K, Welk A, Lindemann K, et al. C-Met overexpression in node-positive breast cancer identifies patients with poor clinical outcome independent of Her2/neu. Int J Cancer. 2005;113(4):678–82.
Sawada K, Radjabi AR, Shinomiya N, Kistner E, Kenny H, Becker AR, et al. c-Met overexpression is a prognostic factor in ovarian cancer and an effective target for inhibition of peritoneal dissemination and invasion. Cancer Res. 2007;67(4):1670–9.
Verhoef EI, Kolijn K, De Herdt MJ, van der Steen B, Hoogland AM, Sleddens HF, et al. MET expression during prostate cancer progression. Oncotarget. 2016;7(21):31029–36.
Cazes A, Betancourt O, Esparza E, Mose ES, Jaquish D, Wong E, et al. A MET targeting antibody-drug conjugate overcomes gemcitabine resistance in pancreatic cancer. Clin Cancer Res. 2021;27(7):2100–10.
Lee HE, Kim MA, Lee HS, Jung EJ, Yang HK, Lee BL, et al. MET in gastric carcinomas: comparison between protein expression and gene copy number and impact on clinical outcome. Br J Cancer. 2012;107(2):325–33.
Ansell PJ, Camidge DR, Baijal S, Xia X, Vasilopoulos A, Li M, et al. Evaluation of the prevalence of MET and protein tyrosine kinase 7 expression in non-small cell lung cancer to evaluate overlap of ADC antigens. J Clin Oncol. 2023;41(16_suppl):e21105–e.
Lin E, Lo Y, Parikh K, Smrecek N, Goliwas K, Deshane J, et al. 4P Optimizing utilization of antibody-drug conjugates in NSCLC by identification of subsets using RNA sequencing. ESMO Open. 2023;8(1).
Liu X, Newton RC, Scherle PA. Developing c-MET pathway inhibitors for cancer therapy: progress and challenges. Trends Mol Med. 2010;16(1):37–45.
Cecchi F, Rabe DC, Bottaro DP. Targeting the HGF/Met signalling pathway in cancer. Eur J Cancer. 2010;46(7):1260–70.
Peters S, Adjei AA. MET: a promising anticancer therapeutic target. Nat Rev Clin Oncol. 2012;9(6):314–26.
Lee D, Sung ES, Ahn JH, An S, Huh J, You WK. Development of antibody-based c-Met inhibitors for targeted cancer therapy. Immunotargets Ther. 2015;4:35–44.
Parikh PK, Ghate MD. Recent advances in the discovery of small molecule c-Met Kinase inhibitors. Eur J Med Chem. 2018;143:1103–38.
Ou SH, Kwak EL, Siwak-Tapp C, Dy J, Bergethon K, Clark JW, et al. Activity of crizotinib (PF02341066), a dual mesenchymal-epithelial transition (MET) and anaplastic lymphoma kinase (ALK) inhibitor, in a non-small cell lung cancer patient with de novo MET amplification. J Thorac Oncol. 2011;6(5):942–6.
Yakes FM, Chen J, Tan J, Yamaguchi K, Shi Y, Yu P, et al. Cabozantinib (XL184), a novel MET and VEGFR2 inhibitor, simultaneously suppresses metastasis, angiogenesis, and tumor growth. Mol Cancer Ther. 2011;10(12):2298–308.
Yap TA, Olmos D, Brunetto AT, Tunariu N, Barriuso J, Riisnaes R, et al. Phase I trial of a selective c-MET inhibitor ARQ 197 incorporating proof of mechanism pharmacodynamic studies. J Clin Oncol. 2011;29(10):1271–9.
Aoyama A, Katayama R, Oh-Hara T, Sato S, Okuno Y, Fujita N. Tivantinib (ARQ 197) exhibits antitumor activity by directly interacting with tubulin and overcomes ABC transporter-mediated drug resistance. Mol Cancer Ther. 2014;13(12):2978–90.
Sheridan C. Genentech to salvage anti-MET antibody with subgroup analysis. Nat Biotechnol. 2014;32(5):399–400.
Garber K. MET inhibitors start on road to recovery. Nat Rev Drug Discov. 2014;13(8):563–5.
Grullich C. Cabozantinib: a MET, RET, and VEGFR2 tyrosine kinase inhibitor. Recent Results Cancer Res. 2014;201:207–14.
Heigener DF, Reck M. Crizotinib. Recent Results Cancer Res. 2014;201:197–205.
Monzavi N, Zargar SJ, Gheibi N, Azad M, Rahmani B. Angiopoietin-like protein 8 (betatrophin) may inhibit hepatocellular carcinoma through suppressing of the Wnt signaling pathway. Iran J Basic Med Sci. 2019;22(10):1166–71.
Asadian S, Piryaei A, Gheibi N, Aziz Kalantari B, Reza Davarpanah M, Azad M, et al. Rhenium Perrhenate ((188)ReO(4)) induced apoptosis and reduced cancerous phenotype in liver cancer cells. Cells. 2022;11(2).
Fujiwara Y, Kenmotsu H, Yamamoto N, Shimizu T, Yonemori K, Ocampo C, et al. Phase 1 study of telisotuzumab vedotin in Japanese patients with advanced solid tumors. Cancer Med. 2021;10(7):2350–8.
Zhang Y, Jain RK, Zhu M. Recent Progress and Advances in HGF/MET-Targeted Therapeutic Agents for Cancer Treatment. Biomedicines. 2015;3(1):149–81.
Pietronave S, Forte G, Locarno D, Merlin S, Zamperone A, Nicotra G, et al. Agonist monoclonal antibodies against HGF receptor protect cardiac muscle cells from apoptosis. Am J Physiol Heart Circ Physiol. 2010;298(4):H1155–65.
Prat M, Crepaldi T, Pennacchietti S, Bussolino F, Comoglio PM. Agonistic monoclonal antibodies against the Met receptor dissect the biological responses to HGF. J Cell Sci. 1998;111(Pt 2):237–47.
Jin H, Yang R, Zheng Z, Romero M, Ross J, Bou-Reslan H, et al. MetMAb, the one-armed 5D5 anti-c-Met antibody, inhibits orthotopic pancreatic tumor growth and improves survival. Cancer Res. 2008;68(11):4360–8.
Patnaik A, Weiss GJ, Papadopoulos KP, Hofmeister CC, Tibes R, Tolcher A, et al. Phase I ficlatuzumab monotherapy or with erlotinib for refractory advanced solid tumours and multiple myeloma. Br J Cancer. 2014;111(2):272–80.
Jun HT, Sun J, Rex K, Radinsky R, Kendall R, Coxon A, et al. AMG 102, a fully human anti-hepatocyte growth factor/scatter factor neutralizing antibody, enhances the efficacy of temozolomide or docetaxel in U-87 MG cells and xenografts. Clin Cancer Res. 2007;13(22 Pt 1):6735–42.
Fujita R, Blot V, Wong E, Stewart C, Lieuw V, Richardson R, et al. A novel non-agonist c-Met antibody drug conjugate with superior potency over a c-Met tyrosine kinase inhibitor in c-Met amplified and non-amplified cancers. Cancer Biol Ther. 2020;21(6):549–59.
Lai KC, Muvaffak A, Li M, Themeles M, Sikka S, Donahue K, et al. Abstract 45: In vitro and in vivo activity of a novel c-Met-targeting antibody-drug conjugate using a DNA-alkylating, indolinobenzodiazepine payload. Cancer Res. 2017;77(13_Supplement):45-.
Yaghoubi S, Karimi MH, Lotfinia M, Gharibi T, Mahi-Birjand M, Kavi E, et al. Potential drugs used in the antibody-drug conjugate (ADC) architecture for cancer therapy. J Cell Physiol. 2020;235(1):31–64.
Abdollahpour-Alitappeh M, Lotfinia M, Gharibi T, Mardaneh J, Farhadihosseinabadi B, Larki P, et al. Antibody-drug conjugates (ADCs) for cancer therapy: Strategies, challenges, and successes. J Cell Physiol. 2019;234(5):5628–42.
Najminejad Z, Dehghani F, Mirzaei Y, Mer AH, Saghi SA, Abdolvahab MH, et al. Clinical perspective: Antibody-drug conjugates for the treatment of HER2-positive breast cancer. Mol Ther. 2023;31(7):1874–903.
Fu Z, Li S, Han S, Shi C, Zhang Y. Antibody drug conjugate: the “biological missile” for targeted cancer therapy. Signal Transduct Target Ther. 2022;7(1):93.
Esapa B, Jiang J, Cheung A, Chenoweth A, Thurston DE, Karagiannis SN. Target antigen attributes and their contributions to clinically approved antibody-drug conjugates (ADCs) in haematopoietic and solid cancers. Cancers (Basel). 2023;15(6).
Marcucci F, Caserta CA, Romeo E, Rumio C. Antibody-drug conjugates (ADC) against cancer stem-like cells (CSC)-is there still room for optimism? Front Oncol. 2019;9:167.
Fan J, Zhuang X, Yang X, Xu Y, Zhou Z, Pan L, et al. A multivalent biparatopic EGFR-targeting nanobody drug conjugate displays potent anticancer activity in solid tumor models. Signal Transduct Target Ther. 2021;6(1):320.
Joubert N, Beck A, Dumontet C, Denevault-Sabourin C. Antibody-drug conjugates: The last decade. Pharmaceuticals (Basel). 2020;13(9).
Hussain AF, Grimm A, Sheng W, Zhang C, Al-Rawe M, Brautigam K, et al. Toward homogenous antibody drug conjugates using enzyme-based conjugation approaches. Pharmaceuticals (Basel). 2021;14(4).
Conilh L, Sadilkova L, Viricel W, Dumontet C. Payload diversification: a key step in the development of antibody–drug conjugates. J Hematol Oncol. 2023;16(1):3.
Strickler JH, Weekes CD, Nemunaitis J, Ramanathan RK, Heist RS, Morgensztern D, et al. First-in-human phase I, dose-escalation and -expansion study of telisotuzumab vedotin, an antibody-drug conjugate targeting c-Met, in patients with advanced solid tumors. J Clin Oncol. 2018;36(33):3298–306.
Wang J, Anderson MG, Oleksijew A, Vaidya KS, Boghaert ER, Tucker L, et al. ABBV-399, a c-Met antibody-drug conjugate that targets both MET-amplified and c-Met-overexpressing tumors, irrespective of MET pathway dependence. Clin Cancer Res. 2017;23(4):992–1000.
Camidge DR, Morgensztern D, Heist RS, Barve M, Vokes E, Goldman JW, et al. Phase I study of 2- or 3-week dosing of telisotuzumab vedotin, an antibody-drug conjugate targeting c-Met, monotherapy in patients with advanced non-small cell lung carcinoma. Clin Cancer Res. 2021;27(21):5781–92.
Horinouchi H, Shibata Y, Looman J, Sui Y, Noon E, Lu S. Phase 2 study of telisotuzumab vedotin (Teliso-V) monotherapy in patients with previously untreated MET-amplified locally advanced/metastatic non-squamous non-small cell lung cancer (NSQ NSCLC). J Clin Oncol. 2023;41(16_suppl):TPS9149–TPS.
Batth IS, Jaiswal BS, Maji D, Sparks R, Glauser W, Uziel T, et al. c-MET mutations sensitize to antibody-drug conjugate telisotuzumab vedotin through efficient internalization and rapid intracellular drug delivery. Cancer Res. 2023;83(7_Supplement):540-.
Strickler JH, Nemunaitis JJ, Weekes CD, Ramanathan RK, Angevin E, Morgensztern D, Heist RS, et al. Phase 1, open-label, dose-escalation and expansion study of ABBV-399, an antibody drug conjugate (ADC) targeting c-Met, in patients (pts) with advanced solid tumors. Am Soc Clin Oncol. 2016;2510–2510.
Angevin E, Kelly K, Heist R, Morgensztern D, Weekes C, Bauer T, et al. First-in-human phase 1, dose-escalation and-expansion study of ABBV-399, an antibody-drug conjugate (ADC) targeting c-Met, in patients (pts) with advanced solid tumors. Ann Oncol. 2016;27:vi118.
Camidge DR, Barlesi F, Goldman JW, Morgensztern D, Heist R, Vokes E, et al. A phase 1b study of telisotuzumab vedotin in combination with nivolumab in patients with NSCLC. JTO Clin Res Rep. 2022;3(1):100262.
Camidge DR, Barlesi F, Goldman JW, Morgensztern D, Heist R, Vokes E, et al. Phase Ib study of telisotuzumab vedotin in combination with erlotinib in patients with c-met protein-expressing non-small-cell lung cancer. J Clin Oncol. 2023;41(5):1105–15.
Camidge, D. Ross, Fabrice Barlesi, Jonathan W. Goldman, Daniel Morgensztern, Rebecca Heist, Everett Vokes, Alex Spira et al. Phase Ib study of telisotuzumab vedotin in combination with erlotinib in patients with c-met protein–expressing non–small-cell lung cancer. J Clin Oncol. 2019;41(5):1105.
Camidge R, Heist RS, Goldman J, Angevin E, Strickler J, Morgensztern D, et al. An open-label, multicenter, phase I study of ABBV-399 (telisotuzumab vedotin, teliso-V) as monotherapy (T) and in combination with erlotinib (T+ E) in non-small cell lung cancer (NSCLC). Ann Oncol. 2018;29:viii496–7.
Angevin E, Strickler J, Weekes C, Heist R, Morgensztern D, Fan X, et al. MA09. 09 First-in-human phase 1 study of ABBV-399, an antibody-drug conjugate (ADC) targeting c-Met, in patients with non-small cell lung cancer (NSCLC). J Thorac Oncol. 2017;12(1):S395–6.
Murakami H, Wakuda K, Kenmotsu H, Todaka A, Yokota T, Yamamoto N, et al. Preliminary results of safety and PK of Telisotuzumab Vedotin (T) in Japanese patients with advanced solid tumors. Ann Oncol. 2019;30:vi125.
Camidge D, Goldman J, Cole G, Sun Z, Ocampo C, Komarnitsky P, et al. 1414TiP evaluating telisotuzumab vedotin in combination with osimertinib in patients with advanced non-small cell lung cancer: a phase I/Ib study cohort. Ann Oncol. 2020;31:S894.
Camidge DR, Bar J, Horinouchi H, Goldman JW, Moiseenko FV, Filippova E, Cicin I, et al. Telisotuzumab vedotin (Teliso-V) monotherapy in patients (pts) with previously treated c-Met–overexpressing (OE) advanced non-small cell lung cancer (NSCLC). 2022;9016–6.
Camidge D, Moiseenko F, Cicin I, Horinouchi H, Filippova E, Bar J, et al. OA15. 04 telisotuzumab vedotin (teliso-v) monotherapy in patients with previously treated c-met+ advanced non-small cell lung cancer. J Thorac Oncol. 2021;16(10):S875.
Waqar SN, Redman MW, Arnold SM, Hirsch FR, Mack PC, Schwartz LH, et al. A phase II study of telisotuzumab vedotin in patients with c-met-positive stage IV or recurrent squamous cell lung cancer (LUNG-MAP Sub-study S1400K, NCT03574753). Clin Lung Cancer. 2021;22(3):170–7.
Camidge DR, Goldman J, Vasilopoulos A, Ansell P, Xia S, Bolotin E, et al. Abstract CT214: Preliminary efficacy of telisotuzumab vedotin (Teliso-V) treatment in the 2L/3L setting in MET gene amplified (MET Amp), c-Met protein overexpressing (c-Met OE), non-squamous, non-small cell lung cancer (NSQ NSCLC): Retrospective analysis of LUMINOSITY. Cancer Res. 2023;83(8_Supplement):CT214–CT.
Jin Y, Zhang Z, Zou S, Li F, Chen H, Peng C, et al. A novel c-MET-targeting antibody-drug conjugate for pancreatic cancer. Front Oncol. 2021;11: 634881.
Yang CY, Wang L, Sun X, Tang M, Quan HT, Zhang LS, et al. SHR-A1403, a novel c-Met antibody-drug conjugate, exerts encouraging anti-tumor activity in c-Met-overexpressing models. Acta Pharmacol Sin. 2019;40(7):971–9.
The light of life extension: Hengrui's heavy-handed ADC, a dose of "later medicine". 17 Sep 2023. Available from: https://inf.news/en/news/0aaae0b499c153cb6f27d667cd74e0dc.html.
Yang C, Zhao X, Sun X, Li J, Wang W, Zhang L, et al. Preclinical pharmacokinetics of a novel anti-c-Met antibody-drug conjugate, SHR-A1403, in rodents and non-human primates. Xenobiotica. 2019;49(9):1097–105.
Tong M, Gao M, Xu Y, Fu L, Li Y, Bao X, et al. SHR-A1403, a novel c-mesenchymal-epithelial transition factor (c-Met) antibody-drug conjugate, overcomes AZD9291 resistance in non-small cell lung cancer cells overexpressing c-Met. Cancer Sci. 2019;110(11):3584–94.
Gymnopoulos M, Betancourt O, Blot V, Fujita R, Galvan D, Lieuw V, et al. TR1801-ADC: a highly potent cMet antibody-drug conjugate with high activity in patient-derived xenograft models of solid tumors. Mol Oncol. 2020;14(1):54–68.
RemeGen and Innovent Collaborate on Clinical Trials to Evaluate the Potential of RC88 and RC108 Combined with PD-1 Therapy for Advanced Solid Tumors. 09 Jul, 2023. Available from: https://www.prnewswire.com/news-releases/remegen-and-innovent-collaborate-on-clinical-trials-to-evaluate-the-potential-of-rc88-and-rc108-combined-with-pd-1-therapy-for-advanced-solid-tumors-301872574.html.
Innovent and RemeGen Enter into Clinical Trial Collaboration Investigating Combination Therapy of TYVYT® (sintilimab injection) and Novel ADC Candidates for Advanced Solid Tumors in China. 25 Jun, 2023. Available from: https://www.prnewswire.com/news-releases/innovent-and-remegen-enter-into-clinical-trial-collaboration-investigating-combination-therapy-of-tyvyt-sintilimab-injection-and-novel-adc-candidates-for-advanced-solid-tumors-in-china-301862538.html.
Targeting c-Met, Remegen ADC drug RC108 was approved for clinical use in the United States for the treatment of solid tumors. 03 Jan 2023. Available from: https://www.echemi.com/cms/1144318.html.
Zhou HY, Wang SJ, Liu ZH, Ma K, Wang L, Jiang J. The PK bioanalysis method study of c-Met antibody-drug conjugate (RC108) in cynomolgus monkey. Acta Pharm Sinica. 2023;1663–8.
Groothuis PG, Jacobs DCH, Hermens IAT, Damming D, Berentsen K, Mattaar-Hepp E, et al. Preclinical profile of BYON3521 predicts an effective and safe MET antibody-drug conjugate. Mol Cancer Ther. 2023;22(6):765–77.
Patrick G, Daniëlle J, Inge H, Désirée D, Ellen M, Myrthe R, et al. BYON3521, a novel effective and safe c-Met targeting antibody-drug conjugate. 2021. Available from: https://www.byondis.com/what-we-do/posters-publications/aacr2021/byon3521.
Kotecki N, van Herpen CML, Curigliano C, Hendriks M, Vermaas TC, Corrigan L, et al. Abstract CT185: First in human dose-escalation trial with the c-MET targeting antibody-drug conjugate BYON3521. Cancer Res. 2023;83(8_Supplement):CT185-CT.
Groothuis P, Jacobs D, Hermens I, Damming D, Mattaar E, Rouwette M, et al. Abstract 926: BYON3521, a novel effective and safe c-Met targeting antibody-drug conjugate. Cancer Res. 2021;81(13_Supplement):926-.
Gera N, Fitzgerald K, Ramesh V, Patel P, Kien L, Kanojia D, et al. Abstract 5000: MYTX-011: A novel cMET-targeting antibody drug conjugate (ADC) engineered to increase on-target uptake in and efficacy against cMET expressing tumors. Cancer Res. 2023;83(7_Supplement):5000-.
Spira AI, Johnson ML, Blumenschein GR, Burns TF, Thompson JR, Deshpande A, Comb WC, Fiske B, Gallant G, Heist RS. Phase 1 multicenter dose escalation and dose expansion study of antibody-drug conjugate (ADC) MYTX-011 in subjects with non-small cell lung cancer. 2023;TPS9147–7.
Reilly RM, Ji C, Matuszak RP, Anderson MG, Tucker L, Klunder N, et al. ABBV-400: An ADC delivering a novel topoisomerase 1 inhibitor to c-Met-positive solid tumors. Cancer Res. 2023;83(7_Supplement):6311-.
Sharma M, Kuboki Y, Camidge DR, Perets R, Sommerhalder D, Yamamoto N, Bar J, et al. Dose escalation results from a first-in-human study of ABBV-400, a novel c-Met–targeting antibody-drug conjugate, in advanced solid tumors. 2023;3015–5.
Shimizu T, Powderly J, Sharma MR, Guan X, Vasilopoulos A, Li M, et al. MO4-2 Phase 1 study of ABBV-400, a novel anti-Met antibody drug conjugate, in advanced solid tumors. Ann Oncol. 2023;34:S1397.
Oh SY, Lee YW, Lee EJ, Kim JH, Park Y, Heo SG, et al. Preclinical study of a biparatopic METxMET antibody-drug conjugate, REGN5093-M114, overcomes MET-driven acquired resistance to EGFR TKIs in EGFR-mutant NSCLC. Clin Cancer Res. 2023;29(1):221–32.
DaSilva JO, Yang K, Surriga O, Nittoli T, Kunz A, Franklin MC, et al. A biparatopic antibody-drug conjugate to Treat MET-expressing cancers, including those that are unresponsive to MET pathway blockade. Mol Cancer Ther. 2021;20(10):1966–76.
Perez Bay AE, Faulkner D, DaSilva JO, Young TM, Yang K, Giurleo JT, et al. A bispecific METxMET antibody-drug conjugate with cleavable linker is processed in recycling and late endosomes. Mol Cancer Ther. 2023;22(3):357–70.
Oh SY, Lim SM, Lee YW, Lee EJ, Kim JH, Heo SG, et al. Abstract LB515A: A MET targeting biparatopic antibody-drug conjugates (ADC), REGN5093-M114, has an antitumor efficacy in NSCLC harboring MET gene alterations. Cancer Res. 2022;82(12_Supplement):LB515A–LBA.
Drilon AE, Awad MM, Gadgeel SM, Villaruz LC, Sabari JK, Perez J, Daly C, et al. A phase 1/2 study of REGN5093-M114, a METxMET antibody-drug conjugate, in patients with mesenchymal epithelial transition factor (MET)-overexpressing NSCLC. 2022;TPS8593–3.
Comer F, Mazor Y, Hurt E, Yang C, Fleming R, Shandilya H, et al. Abstract 5736: AZD9592: An EGFR-cMET bispecific antibody-drug conjugate (ADC) targeting key oncogenic drivers in non-small-cell lung cancer (NSCLC) and beyond. Cancer Res. 2023;83(7_Supplement):5736-.
McGrath L, Zheng Y, Christ S, Sachs CC, Khelifa S, Windmüller C, et al. Evaluation of the relationship between target expression and in vivo anti-tumor efficacy of AZD9592, an EGFR/c-MET targeted bispecific antibody drug conjugate. Cancer Res. 2023;83(7_Supplement):5737-.
Aggarwal C, Azzoli CG, Spira AI, Solomon BJ, Le X, Rolfo C, Planchard D, et al. EGRET: a first-in-human study of the novel antibody-drug conjugate (ADC) AZD9592 as monotherapy or combined with other anticancer agents in patients (pts) with advanced solid tumors. 2023;TPS3156–6.
Fu Y, Gros E, Lee A, Johnson K, Zhang H, Yalamanchili S, et al. Abstract P2–16–03: C-Met is a potential therapeutic target for antibody-drug conjugates in breast cancer. Cancer Res. 2015;75(9_Supplement):P2–16–03.
Li L, Fells C, Guo J, Muyot P, Gros E, Zhang Y, et al. Abstract 3897: A novel c-Met targeting antibody drug conjugate for NSCLC. Cancer Res. 2016;76(14_Supplement):3897-.
Fu Y, Gros E, Lee A, Johnson K, Zhang H, Yalamanchili S, Sun Y, Motamed K, Chen G, Jones B, Kaufmann GF. C-Met is a potential therapeutic target for antibody-drug conjugates in breast cancer. In: Proceedings of the thirty-seventh annual CTRC-AACR San Antonio breast cancer symposium. San Antonio, TX. Philadelphia (PA): AACR; Cancer Res 2015;75(9 Suppl): Abstract nr P2-16-03.
Min B, Jin J, Kim H, Her NG, Park C, Kim D, et al. cIRCR201-dPBD, a novel pyrrolobenzodiazepine dimer-containing site-specific antibody-drug conjugate targeting c-Met overexpression tumors. ACS Omega. 2020;5(40):25798–809.
Datta-Mannan A, Choi H, Jin Z, Lu J, Liu L, Stokell D, Murphy A, Dunn K, Martinez M, Feng Y. Reducing target binding affinity improves the therapeutic index of anti-MET antibody drug conjugate in tumor bearing animals. Authorea Preprints. 2023.
Hudson R, Yao H-P, Suthe SR, Patel D, Wang M-H. Antibody-drug conjugate PCMC1D3-Duocarmycin SA as a novel therapeutic entity for targeted treatment of cancers aberrantly expressing MET receptor tyrosine kinase. Curr Cancer Drug Targets. 2022;22(4):312–27.
Sellmann C, Doerner A, Knuehl C, Rasche N, Sood V, Krah S, et al. Balancing selectivity and efficacy of bispecific epidermal growth factor receptor (EGFR) x c-MET antibodies and antibody-drug conjugates. J Biol Chem. 2016;291(48):25106–19.
Chen G, Li L, Muyot P, Gros E, Zhang Y, Sun Y, et al. Abstract LB-002: A novel c-Met/EGFR bispecific targeting antibody drug conjugate for NSCLC. Cancer Res. 2015;75(15_Supplement):LB-002–LB-
Acknowledgements
We would like to thank the authors and researchers whose valuable studies resulted in writing the manuscript.
Funding
The authors received no financial support for the research, authorship, and publication of this manuscript.
Author information
Authors and Affiliations
Contributions
M.A.A. and Y.N. Conceptualized and designed the study. N.Bagheri., Z.K., A.M., and S.J. also helped and participated in the study design. A.H.M., Y.M., F.M., A.B., Z.K., A.M., A.Sh., Z.A., A.J., N.B., and S.J. researched, collected the data, and prepared the original draft. F.M., A.H.M., Y.M., and A.Sh. retrieved data from the clinical trials (https://clinicaltrials.gov). M.A.A. and A.B. draw the figures. M.A.A., Y.N., Z.K., Z.A., A.H.M., and Y.M. draw the tables. A.H.M., Y.M., F.M., N.Bagheri., A.B., Z.K., A.M., A.Sh., Z.A., A.J., N.B., and S.J. prepared the original draft. M.A.A., Y.N., N.Bagheri., Z.K., and A.J. discussed the necessity for writing this manuscript. M.A.A. and Y.N. reviewed and edited the manuscript, and provided detailed feedback. All the authors read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All the authors read and agreed to the published version of the manuscript.
Competing interests
The authors declare that they have no potential conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mer, A.H., Mirzaei, Y., Misamogooe, F. et al. Progress of antibody–drug conjugates (ADCs) targeting c-Met in cancer therapy; insights from clinical and preclinical studies. Drug Deliv. and Transl. Res. (2024). https://doi.org/10.1007/s13346-024-01564-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s13346-024-01564-3