Abstract
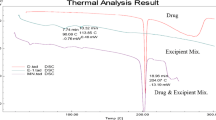
The most promising active ingredient of Crocus sativus L., crocetin (CCT), has been demonstrated to possess many biological activities. However, only a few studies have been conducted on CCT formulation, especially in oral formulation, mainly due to its insolubility in water, which limits its application for oral administration. This article reports an equilibrium saturation solubility and single-pass intestinal perfusion studies conducted to classify the biopharmaceutics classification system (BCS) of CCT. To enhance in vitro dissolution and in vivo oral bioavailability, ternary solid dispersions of CCT (CCT-SDs) with soluplus (SOL) as hydrophilic carrier and meglumine (MEG) as alkalizer were optimized using response surface methodology (RSM) with central composite design (CCD) experiments. Four different preparation methods were evaluated using the optimal formulation, including solvent evaporation, ball milling, spray drying, and freeze-drying. Prepared formulations were characterized by TG-DSC, FTIR, X-RPD, and SEM; the pharmacokinetic studies were performed in rats after oral administration. The cumulative dissolution rate of CCT-SDs containing SOL and MEG prepared by the ball milling method was 97.1% at 15 min and remained at 95.6% at 480 min, which was significantly higher than that of untreated CCT. The lower crystallinity, smaller particle size, and higher microenvironment pH (pHM) were observed in CCT-SDs prepared by the ball milling method. In vivo absorption of CCT-SDs (Cmax = 52.789 ± 12.441 μg/mL and AUC0-12 = 191.748 ± 35.043 μg/mL·h) was greater than untreated CCT (Cmax = 5.918 ± 1.388 μg/mL and AUC0-12 = 44.309 ± 7.264 μg/mL·h). In conclusion, the current study provides ternary solid dispersion formulation of CCT to increase the in vitro dissolution and in vivo bioavailability, which will benefit the commercial production and future clinical applications of CCT.
Graphical abstract








Similar content being viewed by others
Availability of data and materials
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
References
Xing B, Li S, Yang J, Lin D, Feng Y, Lu J, et al. Phytochemistry, pharmacology, and potential clinical applications of saffron: a review. J Ethnopharmacol. 2021;281:114555.
Javadi B, Sahebkar A, Emami SA. A survey on saffron in major islamic traditional medicine books. Iran J Basic Med Sci. 2013;16(1):1–11.
Bastani S, Vahedian V, Rashidi M, Mir A, Mirzaei S, Alipourfard I, et al. An evaluation on potential anti-oxidant and anti-inflammatory effects of Crocin. Biomed Pharmacother. 2022;153.
Zeinali M, Zirak MR, Rezaee SA, Karimi G, Hosseinzadeh H. Immunoregulatory and anti-inflammatory properties of Crocus sativus (Saffron) and its main active constituents: a review. Iran J Basic Med Sci. 2019;22(4):334–44.
Lambrianidou A, Koutsougianni F, Papapostolou I, Dimas K. Recent advances on the anticancer properties of saffron (Crocus sativus L.) and its major constituents. Molecules. 2020;26(1).
Lin S, Li Q, Jiang S, Xu Z, Jiang Y, Liu L, et al. Crocetin ameliorates chronic restraint stress-induced depression-like behaviors in mice by regulating MEK/ERK pathways and gut microbiota. J Ethnopharmacol. 2021;268.
Xu Z, Lin S, Tong Z, Chen S, Cao Y, Li Q, et al. Crocetin ameliorates non-alcoholic fatty liver disease by modulating mitochondrial dysfunction in L02 cells and zebrafish model. J Ethnopharmacol. 2022;285.
Kermanshahi S, Ghanavati G, Abbasi-Mesrabadi M, Gholami M, Ulloa L, Motaghinejad M, et al. Novel neuroprotective potential of crocin in neurodegenerative disorders: an illustrated mechanistic review. Neurochem Res. 2020;45(11):2573–85.
Guo ZL, Li MX, Li XL, Wang P, Wang WG, Du WZ, et al. Crocetin: a systematic review. Front Pharmacol. 2021;12.
Asai A, Nakano T, Takahashi M, Nagao A. Orally administered crocetin and crocins are absorbed into blood plasma as crocetin and its glucuronide conjugates in mice. J Agr Food Chem. 2005;53(18):7302–6.
Lautenschlager M, Sendker J, Huwel S, Galla HJ, Brandt S, Dufer M, et al. Intestinal formation of trans-crocetin from saffron extract (Crocus sativus L.) and in vitro permeation through intestinal and blood brain barrier. Phytomedicine. 2015;22(1):36–44.
Giaccio M. Crocetin from saffron: an active component of an ancient spice. Crit Rev Food Sci. 2004;44(3):155–72.
Kalepu S, Nekkanti V. Insoluble drug delivery strategies: review of recent advances and business prospects. Acta Pharma Sin B. 2015;5(5):442–53.
Xu Z, Lin S, Li Q, Jiang S, Wang P. Recent advances in techniques for enhancing the solubility of hydrophobic drugs. Pak J Pharm Sci. 2022;35(1):95–112.
Yang X. Design and optimization of crocetin loaded PLGA nanoparticles against diabetic nephropathy via suppression of inflammatory biomarkers: a formulation approach to preclinical study. Drug Deliv. 2019;26(1):849–59.
Langroodi FA, Ghahestani ZH, Alibolandi M, Ebrahimian M, Hashemi M. Evaluation of the effect of crocetin on antitumor activity of doxorubicin encapsulated in PLGA nanoparticles. Nanomed J. 2016;3(1):23–34.
Puglia C, Santonocito D, Musumeci T, Cardile V, Graziano A, Salerno L, et al. Nanotechnological approach to increase the antioxidant and cytotoxic efficacy of crocin and crocetin. Planta Med. 2019;85(3):258–65.
Soltani F, Ramezani M, Amel FS, Mokhtarzadeh A, Hashemi M. Comparison study of the effect of alkyl-modified and unmodified PAMAM and PPI dendrimers on solubility and antitumor activity of crocetin. Artif Cell Nanomed B. 2017;45(7):1356–62.
Huang Y, Dai WG. Fundamental aspects of solid dispersion technology for poorly soluble drugs. Acta Pharm Sin B. 2014;4(1):18–25.
Borde S, Paul SK, Chauhan H. Ternary solid dispersions: classification and formulation considerations. Drug Dev Ind Pharm. 2021;47(7):1011–28.
Christina B, Taylor LS, Mauer LJ. Physical stability of l-ascorbic acid amorphous solid dispersions in different polymers: a study of polymer crystallization inhibitor properties. Food Res Int. 2015;76(3):867–77.
Zhang Z, Dong L, Guo J, Li L, Tian B, Zhao Q, et al. Prediction of the physical stability of amorphous solid dispersions: relationship of aging and phase separation with the thermodynamic and kinetic models along with characterization techniques. Expert Opin Drug Del. 2021;18(2):249–64.
Novo DC, Gao C, Qi Q, Mosquera-Giraldo LI, Spiering GA, Moore RB, et al. Designing synergistic crystallization inhibitors: bile salt derivatives of cellulose with enhanced hydrophilicity. Carbohyd Polym. 2022;292.
Jennotte O, Koch N, Lechanteur A, Evrard B. Development of amorphous solid dispersions of cannabidiol: influence of the carrier, the hot-melt extrusion parameters and the use of a crystallization inhibitor. J Drug Deliv Sci Tec. 2022;71.
Meng F, Gala U, Chauhan H. Classification of solid dispersions: correlation to (i) stability and solubility (ii) preparation and characterization techniques. Drug Dev Ind Pharm. 2015;41(9):1401–15.
Ueda H, Hirakawa Y, Tanaka H, Miyano T, Sugita K. Applicability of an experimental grade of hydroxypropyl methylcellulose acetate succinate as a carrier for formation of solid dispersion with indomethacin. Pharmaceutics. 2021;13(3).
Zhao G, Zhang J, Cai P, Ou L, Liang X, Dong W, et al. Effect of carrier material on the thermodynamic properties and recrystallization kinetics of andrographolide-solid dispersion. J Pharm Pharmacol. 2022;74(5):761–8.
Xu Z, Lin S, Gong J, Feng P, Cao Y, Li Q, et al. Exploring the protective effects and mechanism of crocetin from saffron against NAFLD by network pharmacology and experimental validation. Front Med-Lausanne. 2021;8.
Tong Y, Yan Y, Zhu X, Liu R, Gong F, Zhang L, et al. Simultaneous quantification of crocetin esters and picrocrocin changes in Chinese saffron by high-performance liquid chromatography-diode array detector during 15 years of storage. Pharmacogn Mag. 2015;11(43):540–5.
Monteiro PF, Silva-Barcellos NM, Caldeira TG, Reis A, Ribeiro AS, de Souza J. Effects of experimental conditions on solubility measurements for BCS classification in order to improve the biowaiver guidelines. Braz J Pharm Sci. 2021;57.
Xie ZH, Wang ZH, Lv HX. Rapamycin loaded TPGS-Lecithins-Zein nanoparticles based on core-shell structure for oral drug administration. Int J Pharmaceut. 2019;568.
Stampfl U, Radeleff B, Sommer C, Stampfl S, Dahlke A, Bellemann N, et al. Midterm results of uterine artery embolization using narrow-size calibrated embozene microspheres. Cardiovasc Inter Rad. 2011;34(2):295–305.
Markovic M, Zur M, Fine-Shamir N, Haimov E, Gonzalez-Alvarez I, Dahan A. Segmental-dependent solubility and permeability as key factors guiding controlled release drug product development. Pharmaceutics. 2020;12(3).
Zakeri-Milani P, Barzegar-Jalali M, Azimi M, Valizadeh H. Biopharmaceutical classification of drugs using intrinsic dissolution rate (IDR) and rat intestinal permeability. Eur J Pharm Biopharm. 2009;73(1):102–6.
Yang Y, Fan CM, He X, Ren K, Zhang JK, He YJ, et al. Study on biopharmaceutics classification and oral bioavailability of a novel multikinase inhibitor NCE for cancer therapy. Int J Mol Sci. 2014;15(5):7199–212.
Al-Akayleh F, Al-Naji I, Adwan S, Al-Remawi M, Shubair M. Enhancement of curcumin solubility using a novel solubilizing polymer Soluplus(R). J Pharm Innov. 2022;17(1):142–54.
Zi P, Zhang C, Ju CY, Su ZG, Bao YS, Gao J, et al. Solubility and bioavailability enhancement study of lopinavir solid dispersion matrixed with a polymeric surfactant - Soluplus. Eur J Pharm Sci. 2019;134:233–45.
Lamichhane S, Seo JE, Keum T, Noh G, Bashyal S, Cho SW, et al. Enhancing solubility and bioavailability of coenzyme Q(10:) formulation of solid dispersions using Soluplus (R) as a carrier. Arch Pharm Res. 2022;45(1):29–37.
Jia SY, Ning SQ, Leng YT, Jing QF, Xu ZY, Ren FZ. Stabilizing effect of Soluplus on erlotinib metastable crystal form in microparticles and amorphous solid dispersions. Polymers (Basel). 2022;14(6).
Dong LN, Mai YP, Liu Q, Zhang WN, Yang JH. Mechanism and improved dissolution of glycyrrhetinic acid solid dispersion by alkalizers. Pharmaceutics. 2020;12(1).
Haser A, Haight B, Berghaus A, Machado A, Martin C, Zhang F. Scale-up and in-line monitoring during continuous melt extrusion of an amorphous solid dispersion. AAPS PharmSciTech. 2018;19(7):2818–27.
Choi DH, Choi JS. Cilostazol solubilization and stabilization using a polymer-free solid dispersion system. J Pharm Innov. 2022;17(2):521–33.
Salah I, Abou Shamat M, Cook MT. Soluplus solutions as thermothickening materials for topical drug delivery. J Appl Polym Sci. 2019;136(1).
Rani S, Mishra S, Sharma M, Nandy A, Mozumdar S. Solubility and stability enhancement of curcumin in Soluplus (R) polymeric micelles: a spectroscopic study. J Disper Sci Technol. 2020;41(4):523–36.
Jake I, Afrina A, Nazrul I. Formulation and delivery strategies of ibuprofen: challenges and opportunities. Drug Dev Ind Pharm. 2018;44(9):1563.
Hassouna F, El Dahab MA, Fulem M, Haiek AD, Laachachi A, Kopecky D, et al. Multi-scale analysis of amorphous solid dispersions prepared by freeze drying of ibuprofen loaded acrylic polymer nanoparticles. J Drug Deliv Sci Tec. 2019;53.
Wong KH, Xie YN, Huang X, Kadota K, Yao XS, Yu Y, et al. Delivering crocetin across the blood-brain barrier by using gamma-cyclodextrin to treat Alzheimer’s disease. Sci Rep (UK). 2020;10(1).
Jog R, Gokhale R, Burgess DJ. Solid state drug-polymer miscibility studies using the model drug ABT-102. Int J Pharmaceut. 2016;509(1–2):285–95.
Ha NS, Tran T, Tran P, Park JB, Lee BJ. Dissolution-enhancing mechanism of alkalizers in poloxamer-based solid dispersions and physical mixtures containing poorly water-soluble valsartan. Chem Pharm Bull. 2011;59(7):844–50.
Chen WL, di Carlo C, Devery D, McGrath DJ, McHugh PE, Kleinsteinberg K, et al. Fabrication and characterization of gefitinib-releasing polyurethane foam as a coating for drug-eluting stent in the treatment of bronchotracheal cancer. Int J Pharmaceut. 2018;548(2):803–11.
Da Silva K, Ramos F, Chaves JV, Brandao DO, Lins TB, Macedo RO, et al. Characterization of solid dispersions of a powerful statin using thermoanalytical techniques. J Therm Anal Calorim. 2019;138(5):3701–14.
Mustafa WW, Fletcher J, Khoder M, Alany RG. Solid dispersions of gefitinib prepared by spray drying with improved mucoadhesive and drug dissolution properties. AAPS Pharmscitech. 2022;23(1).
Funding
This research has been supported financially by the Key Research and Development Project of Zhejiang Province (No. 2022C03050) and the Science and Technology Research Project of Education Department of Jiangxi Province (No. GJJ171211).
Author information
Authors and Affiliations
Contributions
ZT: conceptualization, methodology, formal analysis, investigation, writing original draft. XL: methodology, formal analysis, investigation. YT: methodology, investigation. PF: methodology, investigation. FL: methodology, investigation. XJ: methodology, investigation. ZX: methodology, investigation. FP: methodology, investigation. ZX: conceptualization, formal analysis, writing—review and editing, project administration. PW: conceptualization, formal analysis, resources, writing—review and editing, supervision.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable. No animal studies have been performed in this research.
Consent for publication
Not applicable. No human studies have been performed in this research.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tong, Z., Liu, X., Tao, Y. et al. Enhancement of dissolution and oral bioavailability by adjusting microenvironment pH in crocetin ternary solid dispersions: Optimization, characterization, in vitro evaluation, and pharmacokinetics. Drug Deliv. and Transl. Res. (2023). https://doi.org/10.1007/s13346-023-01497-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s13346-023-01497-3