Abstract
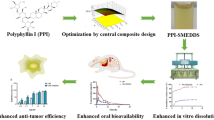
The study aimed to enhance the solubility, dissolution, and oral bioavailability of standardized Piper longum fruits ethanolic extract (PLFEE) via fourth-generation ternary solid dispersion (SD) for melanoma therapy. With the use of solvent evaporation method, the standardized PLFEE was formulated into SD, optimized using Box-Wilson’s central composite design (CCD), and evaluated for pharmaceutical performance and in vivo anticancer activity against melanoma (B16F10)–bearing C57BL/6 mice. The optimized SD showed good accelerated stability, high yield, drug content, and content uniformity for bioactive marker piperine (PIP). The X-ray diffraction (XRD), differential scanning calorimetry (DSC), polarized light microscopy (PLM), and selected area electron diffraction (SAED) analysis revealed its amorphous nature. The attenuated total reflectance-Fourier transform infrared spectroscopy (ATR-FTIR) and high-performance thin layer chromatography (HPTLC) revealed the compatibility of excipients with the PLFEE. The contact angle measurement and in vitro dissolution study revealed excellent wetting of SD and improved dissolution profile as compared to the plain PLFEE. The in vivo oral bioavailability of SD reflected a significant (p < 0.05) improvement in bioavailability (Frel = 188.765%) as compared to plain extract. The in vivo tumor regression study revealed the improved therapeutic activity of SD as compared to plain PLFEE. Further, the SD also improved the anticancer activity of dacarbazine (DTIC) as an adjuvant therapy. The overall result revealed the potential of developed SD for melanoma therapy either alone or as an adjuvant therapy with DTIC.
Graphical Abstract










Similar content being viewed by others
Availability of data and materials
All the data are encompassed in this manuscript. The scientific data in terms of graphs and figures were generated using MS office package, a 21-day free trial version of Origin Pro 2021 (Microcal Software, Inc., Northampton, USA), GraphPad Prism 5.0 (GraphPad Software Inc., San Diego, CA, USA), and ImageJ software (National Institutes of Health, Bethesda, MD).
References
National Institutes of Health (NIH)-2023, National Cancer Institute (NCI), Cancer stat facts: melanoma of the skin; https://seer.cancer.gov/statfacts/html/melan.html.
International Agency for Research on Cancer (IARC)-2023, World Health Organization (WHO), Cancer Today, Estimated number of new cases of melanoma of skin in 2020 among both sexs at all ages; https://gco.iarc.fr/today/online-analysis-pie?v=2020&mode=population&mode_population=continents&population=900&populations=900&key=total&sex=0&cancer=16&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&nb_items=7&group_cancer=0&include_nmsc=1&include_nmsc_other=1&half_pie=0&donut=0
Albuquerque KRS, Pacheco NM, del Rosario Loyo Casao T, de Melo FCSA, Novaes RD, Gonçalves RV. Applicability of plant extracts in preclinical studies of melanoma: a systematic review. Mediators Inflamm.
Gilchrest BA, Eller MS, Geller AC, Yaar M. The pathogenesis of melanoma induced by ultraviolet radiation. N Engl J Med. 1999;340(17):1341–8.
Postow MA, Hamid O, Carvajal RD. Mucosal melanoma: pathogenesis, clinical behavior, and management. Curr Oncol Rep. 2012;14(5):441–8.
Rastrelli M, Tropea S, Rossi CR, Alaibac M. Melanoma: epidemiology, risk factors, pathogenesis, diagnosis and classification. In Vivo. 2014;28(6):1005–11.
Li J, Zhang Y, Tao J. Targeted nanoparticles for drug delivery to melanoma: from bench to bedside. In: Nanoscience in dermatology. Elsevier. 2016;203–215.
Russo AE, Torrisi E, Bevelacqua Y, Perrotta R, Libra M, McCubrey JA, Spandidos DA, Stivala F, Malaponte G. Melanoma: molecular pathogenesis and emerging target therapies. Int J Oncol. 2009;34(6):1481–9.
Li J, Wang Y, Liang R, An X, Wang K, Shen G, Tu Y, Zhu J, Tao J. Recent advances in targeted nanoparticles drug delivery to melanoma. Nanomedicine. 2015;11(3):769–94.
Kratz F, Senter P, Steinhagen H. Drug delivery in oncology: from basic research to cancer therapy. John Wiley & Sons; 2013.
Newman DJ, Cragg GMJJONP. Natural products as sources of new drugs over the nearly four decades from 01/1981 to 09/2019. 2020;83(3):770–803.
Dehelean CA, Marcovici I, Soica C, Mioc M, Coricovac D, Iurciuc S, Cretu OM, Pinzaru I. Plant-derived anticancer compounds as new perspectives in drug discovery and alternative therapy. Molecules. 2021;26(4):1109.
Garcia-Oliveira P, Otero P, Pereira AG, Chamorro F, Carpena M, Echave J, Fraga-Corral M, Simal-Gandara J, Prieto MA. Status and challenges of plant-anticancer compounds in cancer treatment. Pharmaceuticals. 2021;14(2):157.
Pandey S. In vivo antitumor potential of extracts from different parts of Bauhinia variegata linn. Against b16f10 melanoma tumour model in c57bl/6 mice. Appl Can Res. 2017;37(1):1–14
Kinjo J, Nakano D, Fujioka T, Okabe H. Screening of promising chemotherapeutic candidates from plants extracts. J Nat Med. 2016;70(3):335–60.
Kumar S, Kamboj J, Sharma S. Overview for various aspects of the health benefits of Piper longum linn. fruit. J Acupunct Meridian Stud. 2011;4(2):134–40
Tiwari A, Mahadik KR, Gabhe SYJMIDD. Piperine: a comprehensive review of methods of isolation, purification, and biological properties. 2020;7:100027.
National Institute of Health (NIH), U.S. National Library of Medicine; https://clinicaltrials.gov/ct2/results?cond=Piperine%2C+cancer&term=&cntry=&state=&city=&dist=.
Pradeep C, Kuttan G. Piperine is a potent inhibitor of nuclear factor-κB (NF-κB), c-Fos, CREB, ATF-2 and proinflammatory cytokine gene expression in B16F–10 melanoma cells. Int Immunopharmacol. 2004;4(14):1795–803.
Fofaria NM, Kim S-H, Srivastava SK. Piperine causes G1 phase cell cycle arrest and apoptosis in melanoma cells through checkpoint kinase-1 activation. PLoS ONE. 2014;9(5): e94298.
Pradeep C, Kuttan G. Effect of piperine on the inhibition of lung metastasis induced B16F–10 melanoma cells in mice. Clin Exp Metastasis. 2002;19(8):703–8.
Song X, Gao T, Lei Q, Zhang L, Yao Y, Xiong J. Piperlongumine induces apoptosis in human melanoma cells via reactive oxygen species mediated mitochondria disruption. Nutr Cancer. 2018;70(3):502–11.
Kim KS, Kim JA, Eom SY, Lee SH, Min KR, Kim Y. Inhibitory effect of piperlonguminine on melanin production in melanoma B16 cell line by downregulation of tyrosinase expression. Pigment Cell Res. 2006;19(1):90–8.
Brożyna AA, Jóźwicki W, Carlson JA, Slominski AT. Melanogenesis affects overall and disease-free survival in patients with stage III and IV melanoma. Hum Pathol. 2013;44(10):2071–4.
Sunila E, Kuttan G. Piper longum inhibits VEGF and proinflammatory cytokines and tumor-induced angiogenesis in C57BL/6 mice. Int Immunopharmacol. 2006;6(5):733–41.
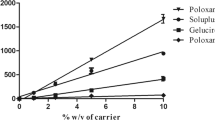
Thenmozhi K, Yoo YJ. Enhanced solubility of piperine using hydrophilic carrier-based potent solid dispersion systems. Drug Dev Ind Pharm. 2017;43(9):1501–9.
Smilkov K, Ackova DG, Cvetkovski A, Ruskovska T, Vidovic B, Atalay M. Piperine: old spice and new nutraceutical? Curr Pharm Des. 2019;25(15):1729–39.
Aodah A, Pavlik A, Karlage K, Myrdal PB. Preformulation studies on piperlongumine PloS one. 2016;11(3): e0151707.
Zhang X, Xing H, Zhao Y, Ma Z. Pharmaceutical dispersion techniques for dissolution and bioavailability enhancement of poorly water-soluble drugs. Pharmaceutics. 2018;10(3):74.
Khadka P, Ro J, Kim H, Kim I, Kim JT, Kim H, Cho JM, Yun G, Lee J. Pharmaceutical particle technologies: an approach to improve drug solubility, dissolution and bioavailability. Asian J Pharm Sci. 2014;9(6):304–16.
Williams HD, Trevaskis NL, Charman SA, Shanker RM, Charman WN, Pouton CW, Porter CJ. Strategies to address low drug solubility in discovery and development. Pharmacol Rev. 2013;65(1):315–499.
Mohapatra D, Agrawal AK, Sahu AN. Exploring the potential of solid dispersion for improving solubility, dissolution & bioavailability of herbal extracts, enriched fractions, and bioactives. J Microencapsul. 2021;38(7–8):594–612.
Gala UH, Miller DA. Williams III RO (2020) Harnessing the therapeutic potential of anticancer drugs through amorphous solid dispersions. Biochim Biophys Acta Rev Cancer. 1873;1: 188319.
Chiou WL, Riegelman S. Pharmaceutical applications of solid dispersion systems. J Pharm Sci. 1971;60(9):1281–302.
Huang Y, Dai W-G. Fundamental aspects of solid dispersion technology for poorly soluble drugs. Acta Pharm Sin B. 2014;4(1):18–25.
Jermain SV, Brough C, Williams RO III. Amorphous solid dispersions and nanocrystal technologies for poorly water-soluble drug delivery–An update. Int J Pharm. 2018;535(1–2):379–92.
Allawadi D, Singh N, Singh S, Arora S. Solid dispersions: a review on drug delivery system and solubility enhancement. ChemInform. 2014;45(18):no-no.
Connors K, Higuchi T. Phase solubility techniques. Adv Anal Chem Instrum. 1965;4(2).
Ha E-S, Baek I-h, Cho W, Hwang S-J, Kim M-S. Preparation and evaluation of solid dispersion of atorvastatin calcium with Soluplus® by spray drying technique. Chem Pharm Bull. 2014;62(6):545–51.
Shaker MA. Dissolution and bioavailability enhancement of Atorvastatin: Gelucire semi-solid binary system. J Drug Deliv Sci Technol. 2018;43:178–84.
Kyaw Oo M, Mandal UK, Chatterjee B. Polymeric behavior evaluation of PVP K30-poloxamer binary carrier for solid dispersed nisoldipine by experimental design. Pharm Dev Technol. 2017;22(1):2–12.
Saoji SD, Dave VS, Dhore PW, Bobde YS, Mack C, Gupta D, Raut NA. The role of phospholipid as a solubility-and permeability-enhancing excipient for the improved delivery of the bioactive phytoconstituents of Bacopa monnieri. Eur J Pharm Sci. 2017;108:23–35.
Rahman SNR, Pawde DM, Katari O, Hmingthansanga V, Shunmugaperumal T. Systematic optimization, in vitro drug release, and preliminary nonclinical toxicity assessment of nonphospholipid-based topical ophthalmic emulsions containing 0.05 or 0.1% w/w cyclosporin A for dry-eye syndrome management. AAPS Pharm Sci Tech. 21 2020;(2):36.
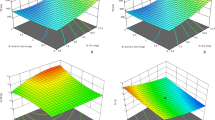
Sharma N, Singh S. Central composite designed ezetimibe solid dispersion for dissolution enhancement: synthesis and in vitro evaluation. Ther Deliv. 2019;10(10):643–58.
Khar RK. Lachman/liebermans: the theory and practice of industrial pharmacy. Cbs Publishers & Distribu. 2013.
Shamma RN, Basha M. Soluplus®: a novel polymeric solubilizer for optimization of carvedilol solid dispersions: formulation design and effect of method of preparation. Powder Technol. 2013;237:406–14.
Pramod K, Suneesh CV, Shanavas S, Ansari SH, Ali J. Unveiling the compatibility of eugenol with formulation excipients by systematic drug-excipient compatibility studies. J Anal Sci Technol. 2015;6(1):1–14.
Gouda R, Baishya H, Qing Z. Application of mathematical models in drug release kinetics of carbidopa and levodopa ER tablets. J Dev Drugs. 2017;6(02):1–8.
Kumar DN, Chaudhuri A, Dehari D, Shekher A, Gupta SC, Majumdar S, Krishnamurthy S, Singh S, Kumar D, Agrawal AKJL. Combination therapy comprising paclitaxel and 5-fluorouracil by using folic acid functionalized bovine milk exosomes improves the therapeutic efficacy against breast cancer. 2022;12(8):1143.
Mohapatra D, Alam MB, Pandey V, Pratap R, Dubey PK, Parmar AS, Sahu AN. Carbon dots from an immunomodulatory plant for cancer cell imaging, free radical scavenging and metal sensing applications. Nanomedicine. 2021;16(23):2039–59.
Zhang Y, Huo M, Zhou J, Xie S. PKSolver: an add-in program for pharmacokinetic and pharmacodynamic data analysis in Microsoft Excel. Comput Methods Programs Biomed. 2010;99(3):306–14.
OECD guidelines for the testing of chemicals : acute oral toxicity – up-and-down-procedure (UDP); https://www.oecd.org/env/test-no-425-acute-oral-toxicity-up-and-down-procedure-9789264071049-en.htm.
Tsubaki M, Takeda T, Obata N, Kawashima K, Tabata M, Imano M, Satou T, Nishida S. Combination therapy with dacarbazine and statins improved the survival rate in mice with metastatic melanoma. J Cell Physiol. 2019;234(10):17975–89.
Gorgani L, Mohammadi M, Najafpour GD, Nikzad M. Piperine—the bioactive compound of black pepper: from isolation to medicinal formulations. Compr Rev Food Sci Food Saf. 2017;16(1):124–40.
United States Pharmacopeia (USP) 30, 〈467〉, Residual solvents, VERSION-8/TEMPLATE/ V8_USPNF/V8_USPNF.3F; https://www.uspnf.com/sites/default/files/usp_pdf/EN/USPNF/generalChapter467Current.pdf.
Impurities: guideline for residual solvents Q3C(R8), Step 4 version, 22 April 2021. International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human use, ICH Harmonised Guideline; https://database.ich.org/sites/default/files/ICH_Q3C-R8_Guideline_Step4_2021_0422_1.pdf.
Sahu A N and Mohapatra D, Herbal drug formulation and standardization. 1 edn. (21 June 2021), ISBN-10: 9390658365, ISBN-13: 978-9390658367, Ane Books Pvt Ltd., Darya Ganj, New Delhi - 110002.
Li S, Han Q, Qiao C, Song J, Cheng CL, Xu H. Chemical markers for the quality control of herbal medicines: an overview. Chin Med. 2008;3(1):1–16.
Colombo M, de Lima MG, Michels LR, Figueiró F, Bassani VL, Teixeira HF, Koester LS. Solid dispersion of kaempferol: formulation development, characterization, and oral bioavailability assessment. AAPS Pharm SciTech. 2019;20(3):1–9.
Hwang DH, Kim Y-I, Cho KH, Poudel BK, Choi JY, Kim D-W, Shin Y-J, Bae O-N, Yousaf AM, Yong CS. A novel solid dispersion system for natural product-loaded medicine: silymarin-loaded solid dispersion with enhanced oral bioavailability and hepatoprotective activity. J Microencapsul. 2014;31(7):619–26.
Kaur P, Singh SK, Garg V, Gulati M, Vaidya Y. Optimization of spray drying process for formulation of solid dispersion containing polypeptide-k powder through quality by design approach. Powder Technol. 2015;284:1–11.
Saokham P, Muankaew C, Jansook P, Loftsson T. Solubility of cyclodextrins and drug/cyclodextrin complexes. Molecules. 2018;23(5):1161.
Alopaeus JF, Hagesæther E, Tho I. Micellisation mechanism and behaviour of Soluplus®–furosemide micelles: preformulation studies of an oral nanocarrier-based system. Pharmaceuticals. 2019;12(1):15.
Solubility Enhancement with BASF Pharma Polymers. Solubilizer Compendium, Pharma Ingredients & Services: Lampertheim, Germany. 2011; https://pharmaceutical.basf.com/global/images/b_03_110921e_solubility_enhance_compendium.pdf.
Nair AR, Lakshman YD, Anand VSK, Sree KN, Bhat K, Dengale SJJAP. Overview of extensively employed polymeric carriers in solid dispersion technology. 2020;21(8):1–20.
Bide Y, Fashapoyeh MA, Shokrollahzadeh S. Structural investigation and application of Tween 80-choline chloride self-assemblies as osmotic agent for water desalination. Sci Rep. 2021;11(1):1–11.
Chen B, Wang X, Zhang Y, Huang K, Liu H, Xu D, Li S, Liu Q, Huang J, Yao H. Improved solubility, dissolution rate, and oral bioavailability of main biflavonoids from Selaginella doederleinii extract by amorphous solid dispersion. Drug Deliv. 2020;27(1):309–22.
Khan AW, Kotta S, Ansari SH, Sharma RK, Ali J. Enhanced dissolution and bioavailability of grapefruit flavonoid Naringenin by solid dispersion utilizing fourth generation carrier. Drug Dev Ind Pharm. 2015;41(5):772–9.
Zi P, Zhang C, Ju C, Su Z, Bao Y, Gao J, Sun J, Lu J, Zhang C. Solubility and bioavailability enhancement study of lopinavir solid dispersion matrixed with a polymeric surfactant-Soluplus. Eur J Pharm Sci. 2019;134:233–45.
Nitave SA, Chougule NB, Koumaravelou K. Formulation and evaluation of solid dispersion tablet of Andrographis paniculata extract. Pharmacog J. 2018;10(5).
Rehman S, Nabi B, Fazil M, Khan S, Bari NK, Singh R, Ahmad S, Kumar V, Baboota S, Ali J. Role of P-glycoprotein inhibitors in the bioavailability enhancement of solid dispersion of Darunavir. Biomed Res Int. 2017.
Liu P, Zhou J-Y, Chang J-H, Liu X-G, Xue H-F, Wang R-X, Li Z-S, Li C-S, Wang J, Liu C-Z. Soluplus-mediated diosgenin amorphous solid dispersion with high solubility and high stability: development, characterization and oral bioavailability. Drug Des Devel Ther. 2020;14:2959.
Slamova M, Školáková T, Školáková A, Patera J, Zámostný P. Preparation of solid dispersions with respect to the dissolution rate of active substance. J Drug Deliv Sci Technol. 2020;56: 101518.
Rashid R, Kim DW, ud Din F, Mustapha O, Yousaf AM, Park JH, Kim JO, Yong CS, Choi H-G,. Effect of hydroxypropylcellulose and Tween 80 on physicochemical properties and bioavailability of ezetimibe-loaded solid dispersion. Carbohydr Polym. 2015;130:26–31.
Beg S, Hasnain MS, Rahman M, Swain S. Introduction to quality by design (QbD): fundamentals, principles, and applications. In: Pharmaceutical quality by design. Elsevier. 2019;1–17.
Paidi SK, Jena SK, Ahuja BK, Devasari N, Suresh S. Preparation, in-vitro and in-vivo evaluation of spray-dried ternary solid dispersion of biopharmaceutics classification system class II model drug. J Pharm Pharmacol. 2015;67(5):616–29.
Dhillon N, Midha K, Nagpal M, Pahwa R. Formulation, optimization and characterization of solid dispersion of Glibenclamide. Pharm Methods. 2015;6(2).
Aulton ME, Taylor K. Aulton’s pharmaceutics: the design and manufacture of medicines. 5th edn. Elsevier Health Sciences. 2018.
Ezawa T, Inoue Y, Tunvichien S, Suzuki R, Kanamoto I. Changes in the physicochemical properties of piperine/β-cyclodextrin due to the formation of inclusion complexes. Int J Med Chem. 2016.
Ezawa T, Inoue Y, Murata I, Takao K, Sugita Y, Kanamoto I. Characterization of the dissolution behavior of piperine/cyclodextrins inclusion complexes. AAPS Pharm SciTech. 2018;19(2):923–33.
Imam SS, Alshehri S, Alzahrani TA, Hussain A, Altamimi MA. Formulation and evaluation of supramolecular food-grade piperine HP β CD and TPGS complex: dissolution, physicochemical characterization, molecular docking, in vitro antioxidant activity, and antimicrobial assessment. Molecules. 2020;25(20):4716.
Stasiłowicz A, Rosiak N, Tykarska E, Kozak M, Jenczyk J, Szulc P, Kobus-Cisowska J, Lewandowska K, Płazińska A, Płaziński W. Combinations of piperine with hydroxypropyl-β-cyclodextrin as a multifunctional system. Int J Mol Sci. 2021;22(8):4195.
Zaini E, Fitriani L, Ismed F, Horikawa A, Uekusa HJSP. Improved solubility and dissolution rates in novel multicomponent crystals of piperine with succinic acid. 2020;88(2):21.
Lavra ZMM, Pereira de Santana D, Ré MI. Solubility and dissolution performances of spray-dried solid dispersion of Efavirenz in Soluplus. Drug Dev Ind Pharm. 2017;43(1):42–54.
Thakral NK, Ray AR, Bar-Shalom D, Eriksson AH, Majumdar DK. Soluplus-solubilized citrated camptothecin—a potential drug delivery strategy in colon cancer. AAPS Pharm SciTech. 2012;13(1):59–66.
Weerapol Y, Tubtimsri S, Jansakul C, Sriamornsak P. Improved dissolution of Kaempferia parviflora extract for oral administration by preparing solid dispersion via solvent evaporation. Asian J Pharm Sci. 2017;12(2):124–33.
Ding Y, Ding Y, Wang Y, Wang C, Gao M, Xu Y, Ma X, Wu J, Li L. Soluplus®/TPGS mixed micelles for co-delivery of docetaxel and piperine for combination cancer therapy. Pharm Dev Technol. 2020;25(1):107–15.
Lee J-Y, Kang W-S, Piao J, Yoon I-S, Kim D-D, Cho H-J. Soluplus®/TPGS-based solid dispersions prepared by hot-melt extrusion equipped with twin-screw systems for enhancing oral bioavailability of valsartan. Drug Des Devel Ther. 2015;9:2745.
Nanaki S, Eleftheriou RM, Barmpalexis P, Kostoglou M, Karavas E, Bikiaris D. Evaluation of dissolution enhancement of aprepitant drug in ternary pharmaceutical solid dispersions with Soluplus® and Poloxamer 188 prepared by melt mixing. Sci. 2019;1(2):48.
Zhang J, Lu A, Thakkar R, Zhang Y, Maniruzzaman M. Development and evaluation of amorphous oral thin films using solvent-free processes: comparison between 3D printing and hot-melt extrusion technologies. Pharmaceutics. 2021;13(10):1613.
Biswas S, Mukherjee PK, Kar A, Bannerjee S, Charoensub R, Duangyod T. Optimized piperine–phospholipid complex with enhanced bioavailability and hepatoprotective activity. Pharm Dev Technol. 2021;26(1):69–80.
Badria FA, Abdelaziz AE, Hassan AH, Elgazar AA, Mazyed EA. Development of provesicular nanodelivery system of curcumin as a safe and effective antiviral agent: Statistical optimization, in vitro characterization, and antiviral effectiveness. Molecules. 2020;25(23):5668.
Balata G, Shamrool H. Spherical agglomeration versus solid dispersion as different trials to optimize dissolution and bioactivity of silymarin. J Drug Deliv Sci Technol. 2014;24(5):478–85.
Nguyen MN-U, Van Vo T, Tran PH-L, Tran TT-D. Zein-based solid dispersion for potential application in targeted delivery. J Pharm Investig. 2017;47(4):357–64.
Lu Y, Tang N, Lian R, Qi J, Wu W. Understanding the relationship between wettability and dissolution of solid dispersion. Int J Pharm. 2014;465(1–2):25–31.
Salević A, Prieto C, Cabedo L, Nedović V, Lagaron JM. Physicochemical, antioxidant and antimicrobial properties of electrospun poly (ε-caprolactone) films containing a solid dispersion of sage (Salvia officinalis L.) extract. Nanomaterials. 2019;9(2):270.
Shah N, Iyer RM, Mair H-J, Choi D, Tian H, Diodone R, Fahnrich K, Pabst-Ravot A, Tang K, Scheubel E. Improved human bioavailability of vemurafenib, a practically insoluble drug, using an amorphous polymer-stabilized solid dispersion prepared by a solvent-controlled coprecipitation process. J Pharm Sci. 2013;102(3):967–81.
Agrawal AM, Dudhedia MS, Zimny E. Hot melt extrusion: development of an amorphous solid dispersion for an insoluble drug from mini-scale to clinical scale. AAPS Pharm SciTech. 2016;17:133–47.
Farmoudeh A, Rezaeiroshan A, Abbaspour M, Nokhodchi A, Ebrahimnejad P. Solid dispersion pellets: an efficient pharmaceutical approach to enrich the solubility and dissolution rate of deferasirox. Biomed Res Int. 2020.
Nandi U, Ajiboye AL, Patel P, Douroumis D, Trivedi V. Preparation of solid dispersions of simvastatin and soluplus using a single-step organic solvent-free supercritical fluid process for the drug solubility and dissolution rate enhancement. Pharmaceuticals. 2021;14(9):846.
Zhang Q, Polyakov NE, Chistyachenko YS, Khvostov MV, Frolova TS, Tolstikova TG, Dushkin AV, Su W. Preparation of curcumin self-micelle solid dispersion with enhanced bioavailability and cytotoxic activity by mechanochemistry. Drug Deliv. 2018;25(1):198–209.
Mohamed JMM, Alqahtani A, Ahmad F, Krishnaraju V, Kalpana K. Stoichiometrically governed curcumin solid dispersion and its cytotoxic evaluation on colorectal adenocarcinoma cells. Drug Des Devel Ther. 2020;4639–4658.
Song I-S, Cha J-S, Choi M-K. Characterization, in vivo and in vitro evaluation of solid dispersion of curcumin containing d-α-Tocopheryl polyethylene glycol 1000 succinate and mannitol. Molecules. 2016;21(10):1386.
Kuzu OF, Nguyen FD, Noory MA, Sharma A. Current state of animal (mouse) modeling in melanoma research. Cancer Growth Metastasis. 2015;8:CGM. S21214.
Kwon H-K, Hwang J-S, So J-S, Lee C-G, Sahoo A, Ryu J-H, Jeon WK, Ko BS, Im C-R, Lee SH. Cinnamon extract induces tumor cell death through inhibition of NFκB and AP1. BMC Cancer. 2010;10:1–10.
Kwon H-K, Jeon WK, Hwang J-S, Lee C-G, So J-S, Park J-A, Ko BS, Im S-H. Cinnamon extract suppresses tumor progression by modulating angiogenesis and the effector function of CD8+ T cells. Cancer Lett. 2009;278(2):174–82.
Zhang Q-Q, Zhou D-L, Ding Y, Liu H-Y, Lei Y, Fang H-Y, Gu Q-L, He X-D, Qi C-L, Yang YJMR. Andrographolide inhibits melanoma tumor growth by inactivating the TLR4/NF-κB signaling pathway. 2018;24(6):545–555.
Jin J-l, Gong J, Yin T-j, Lu Y-j, Xia J-j, Xie Y-y, Di Y, He L, Guo J-l, Sun J. PTD4-apoptin protein and dacarbazine show a synergistic antitumor effect on B16–F1 melanoma in vitro and in vivo. Eur J Pharmacol. 2011;654(1):17–25.
Surcel M, Constantin C, Caruntu C, Zurac S, Neagu M. Inflammatory cytokine pattern is sex-dependent in mouse cutaneous melanoma experimental model. J Immunol Res. 2017.
Li C, Han X. Co-delivery of dacarbazine and all-trans retinoic acid (ATRA) using lipid nanoformulations for synergistic antitumor efficacy against malignant melanoma. Nanoscale Res Lett. 2020;15(1):1–10.
Alexander A, Qureshi A, Kumari L, Vaishnav P, Sharma M, Saraf S, Saraf S. Role of herbal bioactives as a potential bioavailability enhancer for active pharmaceutical ingredients. Fitoterapia. 2014;97:1–14.
Nabekura T, Yamaki T, Ueno K, Kitagawa SJCC. Pharmacology Inhibition of P-glycoprotein and multidrug resistance protein 1 by dietary phytochemicals. Cancer Chemother Pharmacol. 2008;62:867–73.
Dudhatra GB, Mody SK, Awale MM, Patel HB, Modi CM, Kumar A, Kamani DR, Chauhan BN. A comprehensive review on pharmacotherapeutics of herbal bioenhancers. Sci World J. 2012
Malvi P, Chaube B, Singh SV, Mohammad N, Vijayakumar MV, Singh S, Chouhan S, Bhat MK. Elevated circulatory levels of leptin and resistin impair therapeutic efficacy of dacarbazine in melanoma under obese state. Cancer Metab. 2018;6(1):1–14.
Reid JM, Kuffel MJ, Miller JK, Rios R, Ames MM. Metabolic activation of dacarbazine by human cytochromes P450: the role of CYP1A1, CYP1A2, and CYP2E1. Clin Cancer Res. 1999;5(8):2192–7.
Acknowledgements
The authors are very much thankful to the infrastructural and instrumental facilities provided by the Central Instrument Facility, IIT (BHU); Department of Pharmaceutical Engineering & Technology, IIT (BHU); Department of Physics, IIT (BHU); and Centre for Genetics Disorders, BHU Varanasi, India. The sophisticated analytical instrument facility (SAIF), Indian Institute of Technology (IIT), Mumbai, India, and Rajiv Gandhi Centre for Biotechnology, Thiruvananthapuram, Kerala, India, were also highly acknowledged for GCHS analysis and DNA-based molecular characterization, respectively.
Funding
The financial support for this research was provided as a scholarship to Debadatta Mohapatra by the Ministry of Human Resource Development (MHRD), Government of India. The authors declare that this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Debadatta Mohapatra performed most of the experimental works, collected, processed, analyzed, validated, interpreted data, and wrote the original manuscript. Dulla Naveen Kumar, Singh Shreya, and Vivek Pandey participated in the experiment, reviewed, edited, and scientifically revised the manuscript. Alakh N Sahu, Ashish Kumar Agrawal, and Pawan K. Dubey contributed to conceptualization, project administration, supervision, experiment designing, evaluating, drawing conclusions from data, providing expert assistance, reviewing, and editing the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The experiments on animals were carried out following an approved protocol from Institutional Animal Ethics Committee (IAEC Approval Number: IIT(BHU)/IAEC/2022/001 and IIT(BHU)/IAEC/2023/056).
Consent to participate
Not applicable.
Consent for publicatioon
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mohapatra, D., Kumar, D.N., Shreya, S. et al. Quality by design–based development and optimization of fourth-generation ternary solid dispersion of standardized Piper longum extract for melanoma therapy. Drug Deliv. and Transl. Res. 13, 3094–3131 (2023). https://doi.org/10.1007/s13346-023-01375-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-023-01375-y