Abstract
The most common form of leishmaniasis is cutaneous leishmaniasis (CL). The major difficulties in the treatment of leishmaniasis include emergence of resistance, toxicity, long-term treatment, and the high cost of the current drugs. Although the therapeutic effect of sorafenib (SF) has been demonstrated in both in vitro and in vivo models of Leishmania infection, the therapeutic applications are limited due to severe drug-related toxicity; this is, in turn, due to non-specific distribution in the body. Thus, topical delivery has the advantage of the site directed delivery of SF. This research study evaluated SF-loaded hybrid nanofibers (NFs) which were composed of polycaprolactone (PCL) and cellulose acetate (CA) for the CL topical treatment. Accordingly, SF-loaded hybrid NFs were prepared using the electrospinning method. Formulation variables including total polymer concentration, drug/polymer ratio, and CA concentration were optimized using a full factorial design. The prepared SF-loaded NFs were then characterized for morphology, diameter, encapsulation efficiency (EE)%, drug loading (DL) %, and percentage of release efficiency during a 24-h period (RE24h%); the mechanical characteristics were also considered. The physical state of the drug in the optimized NF was evaluated by the X-ray diffraction analysis. Finally, its in vivo efficacy was determined in L. major–infected mice. The optimized formulation had a smooth, cylindrical, non-beaded shape fiber with a diameter of 281.44 nm, EE of 97.96%, DL of 7.48%, RE of 51.05%, ultimate tensile strength of 1.08 MPa, and Young’s moduli of 74.96 MPa. The XRD analysis also demonstrated the amorphous state of SF in NF. Further, the in vivo results displayed the higher anti-leishmanial activity of the SF-loaded hybrid NF by efficiently healing lesion and successfully reducing the parasite burden. This, thus, indicated the potential of the clinical capability of the SF-loaded hybrid NF for the effective treatment of CL.
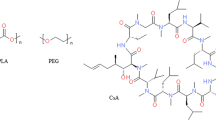
Graphical abstract













Similar content being viewed by others
References
Bates PA. Transmission of Leishmania metacyclic promastigotes by phlebotomine sand flies. Int J Parasitol. 2007;37(10):1097–106.
David CV, Craft N. Cutaneous and mucocutaneous leishmaniasis. Dermatol Ther. 2009;22(6):491–502.
Gupta S, Pal A, Vyas SP. Drug delivery strategies for therapy of visceral leishmaniasis. Expert Opin Drug Deliv. 2010;7(3):371–402.
Peralta MF, Guzman ML, Bracamonte ME, Marco JD, Olivera ME, Carrer DC, et al. Efficacy of topical risedronate and risedronate-Eudragit E complex in a model of cutaneous leishmaniasis induced by Leishmania (Leishmania) amazonensis. Heliyon. 2021;7(5):e07136.
Bilgic-Temel A, Murrell DF, Uzun S. Cutaneous leishmaniasis: a neglected disfiguring disease for women. Int J Women’s Dermatology. 2019;5(3):158–65.
Esfandiari F, Motazedian MH, Asgari Q, Morowvat MH, Molaei M, Heli H. Paromomycin-loaded mannosylated chitosan nanoparticles: synthesis, characterization and targeted drug delivery against leishmaniasis. Acta Trop. 2019;197:105072.
Shahriyar S, Taymouri S, Saberi S, Asadi P, Tabbakhian M. Preparation and characterization of itraconazole loaded nanomicelles based on dextran–behenic acid for cutaneous leishmaniasis treatment. Drug Dev Ind Pharm. 2021;47(3):416–28.
Wang C-F, Mäkilä EM, Kaasalainen MH, Hagström MV, Salonen JJ, Hirvonen JT, et al. Dual-drug delivery by porous silicon nanoparticles for improved cellular uptake, sustained release, and combination therapy. Acta Biomater. 2015;16:206–14.
Sanderson L, Yardley V, Croft SL. Activity of anti-cancer protein kinase inhibitors against Leishmania spp. J Antimicrob Chemother. 2014;69(7):1888–91.
Abou-El-Naga IF, Mady RF, Hussien Mogahed NMF. In vitro effectivity of three approved drugs and their synergistic interaction against Leishmania infantum. Biomedica. 2020;40:89–101.
Bondì ML, Botto C, Amore E, Emma MR, Augello G, Craparo EF, et al. Lipid nanocarriers containing sorafenib inhibit colonies formation in human hepatocarcinoma cells. Int J Pharm. 2015;493(1–2):75–85.
Ahiwale RJ, Chellampillai B, Pawar AP. Investigation of novel sorafenib tosylate loaded biomaterial based nano-cochleates dispersion system for treatment of hepatocellular carcinoma. J Dispers Sci Technol. 2022;43(10):1568–86.
Jain S, Tripathi S, Tripathi PK. Invasomes: potential vesicular systems for transdermal delivery of drug molecules. J Drug Deliv Sci Technol. 2021;61:102166.
Van Bocxlaer K, Yardley V, Murdan S, Croft SL. Topical formulations of miltefosine for cutaneous leishmaniasis in a BALB/c mouse model. J Pharm Pharmacol. 2016;68(7):862–72.
Zamani M, Prabhakaran MP, Ramakrishna S. Advances in drug delivery via electrospun and electrosprayed nanomaterials. Int J Nanomedicine. 2013;8:2997.
Abid S, Hussain T, Raza ZA, Nazir A. Current applications of electrospun polymeric nanofibers in cancer therapy. Mater Sci Eng C. 2019;97:966–77.
Kataria K, Gupta A, Rath G, Mathur RB, Dhakate SR. In vivo wound healing performance of drug loaded electrospun composite nanofibers transdermal patch. Int J Pharm. 2014;469(1):102–10.
Goyal R, Macri LK, Kaplan HM, Kohn J. Nanoparticles and nanofibers for topical drug delivery. J Control Release. 2016;240:77–92.
Esentürk İ, Balkan T, Özhan G, Döşler S, Güngör S, Erdal MS, et al. Voriconazole incorporated nanofiber formulations for topical application: preparation, characterization and antifungal activity studies against Candida species. Pharm Dev Technol. 2020;25(4):440–53.
Alishahi M, Khorram M, Asgari Q, Davani F, Goudarzi F, Emami A, et al. Glucantime-loaded electrospun core-shell nanofibers composed of poly (ethylene oxide)/gelatin-poly (vinyl alcohol)/chitosan as dressing for cutaneous leishmaniasis. Int J Biol Macromol. 2020;163:288–97.
Rahimi M, Tabaei SJS, Ziai SA, Sadri M. Anti-leishmanial effects of chitosan-polyethylene oxide nanofibers containing berberine: an applied model for leishmania wound dressing. Iran J Med Sci. 2020;45(4):286.
Khan G, Patel RR, Yadav SK, Kumar N, Chaurasia S, Ajmal G, et al. Development, optimization and evaluation of tinidazole functionalized electrospun poly (ε-caprolactone) nanofiber membranes for the treatment of periodontitis. RSC Adv. 2016;6(102):100214–29.
Khan G, Yadav SK, Patel RR, Kumar N, Bansal M, Mishra B. Tinidazole functionalized homogeneous electrospun chitosan/poly (ε-caprolactone) hybrid nanofiber membrane: Development, optimization and its clinical implications. Int J Biol Macromol. 2017;103:1311–26.
Zhijiang C, Yi X, Haizheng Y, Jia J, Liu Y. Poly (hydroxybutyrate)/cellulose acetate blend nanofiber scaffolds: preparation, characterization and cytocompatibility. Mater Sci Eng C. 2016;58:757–67.
Unnithan AR, Gnanasekaran G, Sathishkumar Y, Lee YS, Kim CS. Electrospun antibacterial polyurethane–cellulose acetate–zein composite mats for wound dressing. Carbohydr Polym. 2014;102:884–92.
Samadian H, Zamiri S, Ehterami A, Farzamfar S, Vaez A, Khastar H, et al. Electrospun cellulose acetate/gelatin nanofibrous wound dressing containing berberine for diabetic foot ulcer healing: in vitro and in vivo studies. Sci Rep. 2020;10(1):1–12.
Hou J, Sun X, Zhang W, Li L, Teng H. Preparation and characterization of electrospun fibers based on poly (L-lactic acid)/cellulose acetate. Chinese J Polym Sci. 2012;30(6):916–22.
Vatankhah E. Rosmarinic acid-loaded electrospun nanofibers: in vitro release kinetic study and bioactivity assessment. Eng Life Sci. 2018;18(10):732–42.
Kar S, Sharma G, Das PK. Fucoidan cures infection with both antimony-susceptible and-resistant strains of Leishmania donovani through Th1 response and macrophage-derived oxidants. J Antimicrob Chemother. 2011;66(3):618–25.
Maheshwari SU, Kumar SV, Nagiah N, Uma TS. Electrospinning of polyvinylalcohol–polycaprolactone composite scaffolds for tissue engineering applications. Polym Bull. 2013;70(11):2995–3010.
Herrero-Herrero M, Gómez-Tejedor J-A, Vallés-Lluch A. PLA/PCL electrospun membranes of tailored fibres diameter as drug delivery systems. Eur Polym J. 2018;99:445–55.
Zahedi P, Rezaeian I, Jafari SH, Karami Z. Preparation and release properties of electrospun poly (vinyl alcohol)/poly (ɛ-caprolactone) hybrid nanofibers: optimization of process parameters via D-optimal design method. Macromol Res. 2013;21(6):649–59.
Moradkhannejhad L, Abdouss M, Nikfarjam N, Shahriari MH, Heidary V. The effect of molecular weight and content of PEG on in vitro drug release of electrospun curcumin loaded PLA/PEG nanofibers. J Drug Deliv Sci Technol. 2020;56:101554.
Taymouri S, Hashemi S, Varshosaz J, Minaiyan M, Talebi A. Fabrication and evaluation of hesperidin loaded polyacrylonitrile/polyethylene oxide nanofibers for wound dressing application. J Biomater Sci Polym Ed. 2021;32(15):1944–65.
Alavarse AC, de Oliveira Silva FW, Colque JT, da Silva VM, Prieto T, Venancio EC, et al. Tetracycline hydrochloride-loaded electrospun nanofibers mats based on PVA and chitosan for wound dressing. Mater Sci Eng C. 2017;77:271–81.
Eskitoros-Togay ŞM, Bulbul YE, Tort S, Korkmaz FD, Acartürk F, Dilsiz N. Fabrication of doxycycline-loaded electrospun PCL/PEO membranes for a potential drug delivery system. Int J Pharm. 2019;565:83–94.
Chen SC, Huang XB, Cai XM, Lu J, Yuan J, Shen J. The influence of fiber diameter of electrospun poly (lactic acid) on drug delivery. Fibers Polym. 2012;13(9):1120–5.
Kaur D, Dhakate SR, Gupta A. Anti-emetic drug delivery for cancer patients through electrospun composite nanofibers transdermal patch: in vitro study. Adv Mater Lett. 2015;6(1):33–9.
Zupančič Š, Potrč T, Baumgartner S, Kocbek P, Kristl J. Formulation and evaluation of chitosan/polyethylene oxide nanofibers loaded with metronidazole for local infections. Eur J Pharm Sci. 2016;95:152–60.
Zamani M, Morshed M, Varshosaz J, Jannesari M. Controlled release of metronidazole benzoate from poly ε-caprolactone electrospun nanofibers for periodontal diseases. Eur J Pharm Biopharm. 2010;75(2):179–85.
Ramos DM, Abdulmalik S, Arul MR, Rudraiah S, Laurencin CT, Mazzocca AD, et al. Insulin immobilized PCL-cellulose acetate micro-nanostructured fibrous scaffolds for tendon tissue engineering. Polym Adv Technol. 2019;30(5):1205–15.
ElMessiry M, Fadel N. The tensile properties of electrospun poly vinyl chloride and cellulose acetate (PVC/CA) bi-component polymers nanofibers. Alexandria Eng J. 2019;58(3):885–90.
Farzamfar S, Naseri-Nosar M, Samadian H, Mahakizadeh S, Tajerian R, Rahmati M, et al. Taurine-loaded poly (ε-caprolactone)/gelatin electrospun mat as a potential wound dressing material: in vitro and in vivo evaluation. J Bioact Compat Polym. 2018;33(3):282–94.
Ullah A, Saito Y, Ullah S, Haider MK, Nawaz H, Duy-Nam P, et al. Bioactive Sambong oil-loaded electrospun cellulose acetate nanofibers: preparation, characterization, and in-vitro biocompatibility. Int J Biol Macromol. 2021;166:1009–21.
Khoshbakht S, Asghari-Sana F, Fathi-Azarbayjani A, Sharifi Y. Fabrication and characterization of tretinoin-loaded nanofiber for topical skin delivery. Biomater Res. 2020;24(1):1–7.
Nasehi N, Varshosaz J, Taymouri S, Rostami M, Akbari V, Firoozpour L. Sorafenib loaded pluronic F127-lithocholic acid micelles for prostate cancer therapy: formulation, optimization, and in vitro evaluation against LNCaP cells. Int J Polym Mater Polym Biomater. 2020;69(3):158–72.
Aghdam RM, Najarian S, Shakhesi S, Khanlari S, Shaabani K, Sharifi S. Investigating the effect of PGA on physical and mechanical properties of electrospun PCL/PGA blend nanofibers. J Appl Polym Sci. 2012;124(1):123–31.
Yu D-G, Li X-Y, Wang X, Chian W, Liao Y-Z, Li Y. Zero-order drug release cellulose acetate nanofibers prepared using coaxial electrospinning. Cellulose. 2013;20(1):379–89.
Lu H, Wang Q, Li G, Qiu Y, Wei Q. Electrospun water-stable zein/ethyl cellulose composite nanofiber and its drug release properties. Mater Sci Eng C. 2017;74:86–93.
Kamble RN, Gaikwad S, Maske A, Patil SS. Fabrication of electrospun nanofibres of BCS II drug for enhanced dissolution and permeation across skin. J Adv Res. 2016;7(3):483–9.
Song J, Fan X, Shen Q. Daidzein-loaded nanostructured lipid carriers-PLGA nanofibers for transdermal delivery. Int J Pharm. 2016;501(1–2):245–52.
McLoughlin CE, Smith MJ, Auttachoat W, Bowlin GL, White KL. Evaluation of innate, humoral and cell-mediated immunity in mice following in vivo implantation of electrospun polycaprolactone. Biomed Mater. 2012;7(3):35015.
Van Bocxlaer K, Gaukel E, Hauser D, Park SH, Schock S, Yardley V, et al. Topical treatment for cutaneous leishmaniasis: dermato-pharmacokinetic lead optimization of benzoxaboroles. Antimicrob Agents Chemother. 2018;62(5):e02419-e2517.
Santos CM, de Oliveira RB, Arantes VT, Caldeira LR, de Oliveira MC, Egito ES, et al. Amphotericin B-loaded nanocarriers for topical treatment of cutaneous leishmaniasis: development, characterization, and in vitro skin permeation studies. J Biomed Nanotechnol. 2012;8(2):322–9.
Funding
The current research was supported by Research Vice Chancellery of Isfahan University of Medical Sciences (grant number 399358).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All experiments were performed as per the guidelines directed by the Ethical Committee of Isfahan University of Medical Sciences in regard to the care and use of laboratory animals (ethics code number # IR.MUI.RESEARCH.REC.1399.489).
Consent for publication
All authors are happy with this publication.
Competing interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alemomen, M., Taymouri, S., Saberi, S. et al. Preparation, optimization, and in vitro–in vivo evaluation of sorafenib-loaded polycaprolactone and cellulose acetate nanofibers for the treatment of cutaneous leishmaniasis. Drug Deliv. and Transl. Res. 13, 862–882 (2023). https://doi.org/10.1007/s13346-022-01250-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-022-01250-2