Abstract
Glioblastoma multiforme (GBM) is the most prevalent form of brain tumor, which generally has a poor prognosis. According to consensus, recurrence of the tumor and chemotherapy resistance acquisition are the two distinguishing features of GBM originated from glioblastoma stem cells (GSCs). To eliminate these obstacles inherent in GBM chemotherapy, targeting GSCs through a smart drug delivery system has come to the front position of GBM therapeutics. In this study, B19 aptamer (Apt)-conjugated polyamidoamine (PAMAM) G4C12 dendrimer nanoparticles (NPs), called Apt-NPs, were formulated for the co-delivery of paclitaxel (PTX) and temozolomide (TMZ) to U-87 stem cells. These drugs were loaded using a double emulsification solvent evaporation method. As a result, drug-loaded Apt-NPs significantly inhibited the tumor growth of U-87 stem cells, by the initiation of apoptosis via the downregulation of autophagic and multidrug resistance (MDR) genes. Additionally, by their downregulation by qPCR of CD133, CD44, SOX2, and the canonical Wnt/β-catenin pathway, cell proliferation has substantially decreased. Altogether, the results demonstrate that this intelligent drug co-delivery system is capable of effectively transferring PTX and TMZ to U-87 stem cells and without any toxic effect on Apt-NPs alone to U-87 stem cells. Furthermore, the designed dendrimer-based pharmaceutical system along with single-stranded B19 aptamer might be utilized as a new therapeutic strategy for the treatment of U-87 stem cells drug resistance in the GBM.
Graphical abstract







Similar content being viewed by others
Availability of data and materials
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- GBM:
-
Glioblastoma multiforme
- GSCs:
-
Glioblastoma stem cells
- PAMAM:
-
Polyamidoamine
- NPs:
-
Nanoparticles
- PTX:
-
Paclitaxel
- TMZ:
-
Temozolomide
- MDR:
-
Multidrug resistance
- MTIC:
-
5-(3-Methyltriazen-1-yl) imidazole-4-carboxamide
- BBB/BBTB:
-
Blood–brain barrier/blood–brain tumor barrier
- EPR:
-
Permeability and retention
- DTT:
-
1,4-Dithiothreitol
- TNBSA:
-
2,4,6-Trinitrobenzenesulfonic acid solution
- UF:
-
Ultrafiltration
- DEPC:
-
Diethyl pyrocarbonate
- DMSO:
-
Dimethyl sulfoxide
- FTIR:
-
Fourier transform infrared spectroscopy
- FE-SEM:
-
Field emission scanning electron microscopy
- HR-TEM:
-
High-resolution transmission electron microscopy
- SDS:
-
Sodium dodecyl sulfate
- ICC:
-
Immunocytochemistry
- DTX:
-
Docetaxel
References
Taylor OG, Brzozowski JS, Skelding KA. Glioblastoma multiforme: an overview of emerging therapeutic targets. Front Oncol. 2019.
Murayama T, Gotoh N. Drug resistance mechanisms of cancer stem-like cells and their therapeutic potential as drug targets. Cancer Drug Resist. 2019.
Auffinger B, Spencer D, Pytel P, Ahmed AU, Lesniak MS. The role of glioma stem cells in chemotherapy resistance and glioblastoma multiforme recurrence. Expert Rev Neurother. 2015.
Chien CH, Hsueh WT, Chuang JY, Chang KY. Role of autophagy in therapeutic resistance of glioblastoma. J Cancer Metastasis Treat. 2019.
Barzegar Behrooz A, Syahir A, Ahmad S. CD133: beyond a cancer stem cell biomarker. J Drug Target. 2018.
Lee CY. Strategies of temozolomide in future glioblastoma treatment. Onco Targets Ther. 2017.
Baker SD, et al. Absorption, metabolism, and excretion of 14C-temozolomide following oral administration to patients with advanced cancer. Clin Cancer Res. 1999.
Galifianakis NV, Placantonakis DG, Chesler M. Intracellular pH measurements in glioblastoma cells using the pH-sensitive dye BCECF. Methods Mol Biol. 2018.
Appel EA, Rowland MJ, Loh XJ, Heywood RM, Watts C, Scherman OA. Enhanced stability and activity of temozolomide in primary glioblastoma multiforme cells with cucurbit[n]uril. Chem Commun. 2012.
Fruehauf JP, et al. In vitro drug response and molecular markers associated with drug resistance in malignant gliomas. Clin Cancer Res. 2006.
Fung LK, et al. Pharmacokinetics of interstitial delivery of carmustine, 4- hydroperoxycyclophosphamide, and paclitaxel from a biodegradable polymer implant in the monkey brain. Cancer Res. 1998.
Arifin DY, Lee KYT, Wang CH. Chemotherapeutic drug transport to brain tumor. J Control Release. 2009.
Azzabi A, et al. Phase I study of temozolomide plus paclitaxel in patients with advanced malignant melanoma and associated in vitro investigations. Br J Cancer. 2005.
Ni S, Fan X, Wang J, Qi H, Li X. Biodegradable implants efficiently deliver combination of paclitaxel and temozolomide to glioma C6 cancer cells in vitro. Ann Biomed Eng. 2014.
Xu Y, et al. The synergic antitumor effects of paclitaxel and temozolomide co-loaded in mPEG-PLGA nanoparticles on glioblastoma cells. Oncotarget. 2016.
Singh SK, et al. Identification of a cancer stem cell in human brain tumors. Cancer Res. 2003.
Singh SK, et al. Identification of human brain tumour initiating cells. Nature. 2004.
Vora P, et al. The Rational Development of CD133-Targeting Immunotherapies for Glioblastoma. Cell Stem Cell. 2020.
Liou GY. CD133 as a regulator of cancer metastasis through the cancer stem cells. Int J Biochem Cell Biol. 2019.
Hombach-Klonisch S, et al. Glioblastoma and chemoresistance to alkylating agents: Involvement of apoptosis, autophagy, and unfolded protein response. Pharmacol Ther. 2018.
Glaser T, Han I, Wu L, Zeng X. Targeted nanotechnology in glioblastoma multiforme. Front Pharmacol. 2017.
Sercombe L, Veerati T, Moheimani F, Wu SY, Sood AK, Hua S. Advances and challenges of liposome assisted drug delivery. Front Pharmacol. 2015.
Ahmad Z, Shah A, Siddiq M, Kraatz HB. Polymeric micelles as drug delivery vehicles. RSC Adv. 2014.
Jani RK, Krupa G. Active targeting of nanoparticles: an innovative technology for drug delivery in cancer therapeutics. J Drug Deliv Ther. 2019.
Kesharwani P, Jain K, Jain NK. Dendrimer as nanocarrier for drug delivery. Prog Polym Sci. 2014.
Sharma AK, Gothwal A, Kesharwani P, Alsaab H, Iyer AK, Gupta U. Dendrimer nanoarchitectures for cancer diagnosis and anticancer drug delivery. Drug Discov Today. 2017;22(2):314–26.
Chauhan AS. Dendrimers for Drug Delivery. Molecules. 2018;23(4).
Srinageshwar B, et al. PAMAM dendrimers cross the blood–brain barrier when administered through the carotid artery in C57BL/6J mice. Int J Mol Sci. 2017.
Zeng Y, et al. Effects of PAMAM dendrimers with various surface functional groups and multiple generations on cytotoxicity and neuronal differentiation using human neural progenitor cells. J Toxicol Sci. 2016.
Fana M, Gallien J, Srinageshwar B, Dunbar GL, Rossignol J. Pamam dendrimer nanomolecules utilized as drug delivery systems for potential treatment of glioblastoma: a systematic review. Int J Nanomed. 2020.
Ke W, et al. Gene delivery targeted to the brain using an Angiopep-conjugated polyethyleneglycol-modified polyamidoamine dendrimer. Biomaterials. 2009.
Wu X, et al. Second-generation aptamer-conjugated PSMA-targeted delivery system for prostate cancer therapy. Int J Nanomed. 2011.
Wang JL, et al. The effect of surface poly(ethylene glycol) length on in vivo drug delivery behaviors of polymeric nanoparticles. Biomaterials. 2018;182(June):104–13.
Yoon S, Rossi JJ. Aptamers: Uptake mechanisms and intracellular applications. Adv Drug Deliv Rev. 2018.
Shigdar S, et al. RNA aptamers targeting cancer stem cell marker CD133. Cancer Lett. 2013.
Livney YD, Modrejewski J, Walter JG, Engelberg S, Assaraf YG. Cancer cell-selective, clathrin-mediated endocytosis of aptamerdecorated nanoparticles. Oncotarget. 2018.
Wang D, et al. Detection of CD133 expression in U87 glioblastoma cells using a novel anti-CD133 monoclonal antibody. Oncol Lett. 2015.
Platet N, et al. Influence of oxygen tension on CD133 phenotype in human glioma cell cultures. Cancer Lett. 2007.
Zhang L, et al. The necessity for standardization of glioma stem cell culture: a systematic review. Stem Cell Res Ther. 2020.
Yu SC, et al. Isolation and characterization of cancer stem cells from a human glioblastoma cell line U87. Cancer Lett. 2008.
Elliott AD. Confocal microscopy: principles and modern practices. Curr Protoc Cytom. 2020;92(2):e68.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2-ΔΔCT method. Methods. 2001.
Eaton P, et al. A direct comparison of experimental methods to measure dimensions of synthetic nanoparticles. Ultramicroscopy. 2017.
Odeh F, et al. Aptamers chemistry: chemical modifications and conjugation strategies. Molecules. 2019;25(3):1–51.
Haruta K, et al. A novel PEGylation method for improving the pharmacokinetic properties of anti-interleukin-17A RNA aptamers. Nucleic Acid Ther. 2017;27(1):36–44.
Zhu Q, Liu G, Kai M, Miller AOA. DNA aptamers in the diagnosis and treatment of human diseases. Molecules. 2015;20(12):20979–90997.
Germer K, Leonard M, Zhang X. RNA aptamers and their therapeutic and diagnostic applications. Int J Biochem Mol Biol. 2013;4(1):27–40.
Foroozandeh P, Aziz AA. Insight into cellular uptake and intracellular trafficking of nanoparticles. Nanoscale Res Lett. 2018.
Behzadi S, et al. Cellular uptake of nanoparticles: Journey inside the cell. Chem Soc Rev. 2017.
Ceña V, Játiva P. Nanoparticle crossing of blood–brain barrier: a road to new therapeutic approaches to central nervous system diseases. Nanomedicine. 2018.
Danaei M, et al. Impact of particle size and polydispersity index on the clinical applications of lipidic nanocarrier systems. Pharmaceutics. 2018.
Kumari S, Swetha MG, Mayor S. Endocytosis unplugged: multiple ways to enter the cell. Cell Res. 2010.
Contini C, Schneemilch M, Gaisford S, Quirke N. Nanoparticle–membrane interactions. J Exp Nanosci. 2018.
Zhao Y, et al. Nanodrug formed by coassembly of dual anticancer drugs to inhibit cancer cell drug resistance. ACS Appl Mater Interfaces. 2015.
Fröhlich E. The role of surface charge in cellular uptake and cytotoxicity of medical nanoparticles. Int J Nanomed. 2012.
He C, Hu Y, Yin L, Tang C, Yin C. Effects of particle size and surface charge on cellular uptake and biodistribution of polymeric nanoparticles. Biomaterials. 2010.
Chauhan AS, Diwan PV, Jain NK, Tomalia DA. Unexpected in vivo anti-inflammatory activity observed for simple, surface functionalized poly(amidoamine) dendrimers. Biomacromolecules. 2009.
Luo X, Feng M, Pan S, Wen Y, Zhang W, Wu C. Charge shielding effects on gene delivery of polyethylenimine/DNA complexes: PEGylation and phospholipid coating. J Mater Sci Mater Med. 2012.
Barzegar Behrooz A, et al. Smart bomb AS1411 aptamer-functionalized/PAMAM dendrimer nanocarriers for targeted drug delivery in the treatment of gastric cancer. Clin Exp Pharmacol Physiol. 2017;44(1):41–51.
Mishra P, Nayak B, Dey RK. PEGylation in anti-cancer therapy: an overview. Asian J Pharm Sci. 2016.
Zhou G, et al. Aptamer-based therapeutic approaches to target cancer stem cells. Theranostics. 2017.
Xiang D, et al. Superior performance of aptamer in tumor penetration over antibody: Implication of aptamer-based theranostics in solid tumors. Theranostics. 2015.
Li L, et al. Epithelial cell adhesion molecule aptamer functionalized PLGA-lecithin-curcumin-PEG nanoparticles for targeted drug delivery to human colorectal adenocarcinoma cells. Int J Nanomedicine. 2014.
Ding L, et al. Thermoresponsive nanocomposite gel for local drug delivery to suppress the growth of glioma by inducing autophagy. Autophagy. 2017.
Sun T, et al. Targeting transferrin receptor delivery of temozolomide for a potential glioma stem cell-mediated therapy. Oncotarget. 2017.
Singh MK, et al. An innovative in situ method of creating hybrid dendrimer nano-assembly: An efficient next generation dendritic platform for drug delivery. Nanomedicine Nanotechnology Biol Med. 2019.
Buccarelli M, et al. Inhibition of autophagy increases susceptibility of glioblastoma stem cells to temozolomide by igniting ferroptosis. Cell Death Dis. 2018.
Ulasov IV, Lenz G, Lesniak MS. Autophagy in glioma cells: an identity crisis with a clinical perspective. Cancer Lett. 2018.
Yan Y, Xu Z, Dai S, Qian L, Sun L, Gong Z. Targeting autophagy to sensitive glioma to temozolomide treatment. J Exp Clin Cancer Res. 2016.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011.
Nakai E, et al. Enhanced mdr1 expression and chemoresistance of cancer stem cells derived from glioblastoma. Cancer Invest. 2009.
Liu G, et al. Analysis of gene expression and chemoresistance of CD133+ cancer stem cells in glioblastoma. Mol Cancer. 2006.
Ahmed SI, et al. CD133 expression in glioblastoma multiforme: a literature review. Cureus. 2018.
Brown DV, et al. Expression of CD133 and CD44 in glioblastoma stem cells correlates with cell proliferation, phenotype stability and intratumor heterogeneity. PLoS One. 2017.
Brown DV, et al. Coexpression analysis of CD133 and CD44 identifies Proneural and Mesenchymal subtypes of glioblastoma multiforme. Oncotarget. 2015.
Song WS, et al. Sox2, a stemness gene, regulates tumor-initiating and drug-resistant properties in CD133-positive glioblastoma stem cells. J Chin Med Assoc. 2016.
Nager M, Bhardwaj D, Cantí C, Medina L, Nogués P, Herreros J. β-catenin signalling in glioblastoma multiforme and glioma-initiating cells. Chemother Res Pract. 2012.
Hu CMJ, Zhang L. Nanoparticle-based combination therapy toward overcoming drug resistance in cancer. Biochem Pharmacol. 2012.
Persano L, Rampazzo E, Della Puppa A, Pistollato F, Basso G. The three-layer concentric model of glioblastoma: cancer stem cells, microenvironmental regulation, and therapeutic implications. Sci World J. 2011.
McCord M, Mukouyama YS, Gilbert MR, Jackson S. Targeting WNT signaling for multifaceted glioblastoma therapy. Front Cell Neurosci. 2017.
Suwala AK, et al. Inhibition of Wnt/beta-catenin signaling downregulates expression of aldehyde dehydrogenase isoform 3A1 (ALDH3A1) to reduce resistance against temozolomide in glioblastoma in vitro. Oncotarget. 2018.
Zhou C, et al. Pygopus2 inhibits the efficacy of paclitaxel-induced apoptosis and induces multidrug resistance in human glioma cells. Oncotarget. 2017.
He L, Zhou H, Zeng Z, Yao H, Jiang W, Qu H. Wnt/β-catenin signaling cascade: A promising target for glioma therapy. J Cell Physiol. 2019.
Martin-Orozco E, Sanchez-Fernandez A, Ortiz-Parra I, Ayala-San Nicolas M. WNT signaling in tumors: the way to evade drugs and immunity. Front Immunol. 2019.
Lee Y, Lee JK, Ahn SH, Lee J, Nam DH. WNT signaling in glioblastoma and therapeutic opportunities. Lab Investig. 2016.
Tauriello DVF, et al. Wnt/β-catenin signaling requires interaction of the Dishevelled DEP domain and C terminus with a discontinuous motif in Frizzled. Proc Natl Acad Sci USA. 2012.
Major MB, et al. Wilms tumor suppressor WTX negatively regulates WNT/β-catenin signaling. Science 2007;80.
Jaiswal R, Luk F, Dalla PV, Grau GER, Bebawy M. Breast cancer-derived microparticles display tissue selectivity in the transfer of resistance proteins to cells. PLoS One. 2013.
Jaiswal R, Sedger LM. Intercellular vesicular transfer by exosomes, microparticles and oncosomes - Implications for cancer biology and treatments. Front Oncol. 2019.
Schmitt M, Metzger M, Gradl D, Davidson G, Orian-Rousseau V. CD44 functions in Wnt signaling by regulating LRP6 localization and activation. Cell Death Differ. 2015.
Acknowledgements
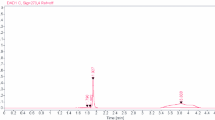
We would like to acknowledge Dr. Tai Boon Tan (Universiti Putra Malaysia) for technical assistance on DLS analyses, Mrs. Marsitah binti Abdul Jalil (Universiti Putra Malaysia) for technical assistance on flow cytometry analyses, Dr. Jamal Adiban (Shahid Beheshti University of Medical Sciences) for assistance in carrier design, and Ms. Fatemeh Tarshizi Moghadam for her help in the graphic illustration. Furthermore, the image of FTIR spectrum was generated using OriginPro 9. Furthermore, we would like to thank EMTech laboratory of UPM for helping some parts of the study. The illustrations were created with BioRender.com.
Funding
This work was supported by the Ministry of Higher Education Malaysia for the Fundamental Research Grant Scheme FRGS/1/2020/STG02/UPM/02/13 (01–01-20-2223FR/5540355).
Author information
Authors and Affiliations
Contributions
Amir Barzegar Behrooz: conceptualization, methodology, writing—original draft preparation; Reza Vazifehmand: methodology, data curation; Asilah Ahmad Tajudin: visualization, investigation, writing—reviewing and editing; Mas Jaffri Masarudin: software, validation; Malihe Masomian: methodology, Zamberi Sekawi: Resources; Amir Syahir: supervision, writing—reviewing and editing, funding acquisition.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study does not involve any animal or human subject; therefore, no ethical approval for this particular study is needed.
Consent for publication
All authors listed in the author list have consented the publication of this manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file3 (.AVI 128 MB)
Rights and permissions
About this article
Cite this article
Behrooz, A.B., Vazifehmand, R., Tajudin, A.A. et al. Tailoring drug co-delivery nanosystem for mitigating U-87 stem cells drug resistance. Drug Deliv. and Transl. Res. 12, 1253–1269 (2022). https://doi.org/10.1007/s13346-021-01017-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-021-01017-1