Abstract
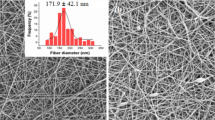
The aim of this work was to develop a transdermal delivery system consisting of a glucosamine sulfate–laden xanthan hydrogel containing a nanoemulsion-loaded diacerein. The system was intended to prevent cartilage degradation typical of osteoarthritis. The nanoemulsion, made of soybean oil as the oil phase; soybean lecithin, Tween 80, and poloxamer 407 as surfactants; and propylene glycol as cosurfactant, was formed within the hydrogel. The hydrodynamic diameter of the nanoemulsion globules was 81.95 ± 0.256 nm with 0.285 ± 0.036 of PDI value and the zeta potential value of the formulation was 39.33 ± 0.812 mV. CryoSEM and TEM studies revealed the uniform morphology of the vehicle. A rheological study exposed the nanoemulsion-loaded hydrogel as a thixotropic system. Satisfactory storage stability under ICH conditions was established by the zeta potential and rheological studies. Furthermore, skin biocompatibility of the hydrogel was ascertained on the basis of skin irritation study. Additionally, the diffusion of the drugs across rat skin followed a controlled non-Fickian anomalous steady mechanism. Following in vivo administration in experimental osteoarthritis, the transdermal hydrogel showed a reduction in tumor necrosis factor-alpha, C-reactive protein, high mobility group box protein, and monocyte chemoattractant protein-1. Finally, histopathological analysis of the animals showed satisfactory chondroprotection in the in vivo study. In conclusion, the developed transdermal systems showed a potential against the progression of experimental osteoarthritis.








Similar content being viewed by others
References
Lee AS, Ellman MB, Yan D, Kroin JS, Cole BJ, Wijnen AJV, et al. A current review of molecular mechanisms regarding osteoarthritis and pain. Gene. 2013;527:440–7.
Steinecker-Frohnwieser B, Weigl L, Kullich W, Lohberger B. The disease modifying osteoarthritis drug diacerein is able to antagonize pro inflammatory state of chondrocytes under mild mechanical stimuli. Osteoarthr Cartil. 2014;22:1044–52.
Jain A, Singh SK, Singh Y, Singh S. Development of lipid nanoparticles of diacerein, an antiosteoarthritic drug for enhancement in bioavailability and reduction in its side effects. J Biomed Nanotechnol. 2013;9:891–900.
Jain A, Mishra SK, Vuddanda PR, Singh SK, Singh R, Singh S. Targeting of diacerein loaded lipid nanoparticles to intra-articular cartilage using chondroitin sulfate as homing carrier for treatment of osteoarthritis in rats. Nanomedicine. 2014;10:1031–40.
Reginster JY, Bruyere O, Neuprez A. Current role of glucosamine in the treatment of osteoarthritis. Rheumatology (Oxford). 2007;46:731–5.
Qu CJ, Karjalainen HM, Helminen HJ, Lammi MJ. The lack of effect of glucosamine sulphate on aggrecan mRNA expression and 35S-sulphate incorporation in bovine primary chondrocytes. Biochim Biophys Acta. 2006;1762:453–9.
Hathcock JN, Shao A. Risk assessment for glucosamine and chondroitin sulfate. Regul Toxicol Pharmacol. 2007;47:78–83.
Sobal G, Menzel J, Sinzinger H. Optimal Te-99m radiolabeling and uptake of glucosamine sulfate by cartilage. A potential tracer for scintigraphic detection of osteoarthritis. Bioconjug Chem. 2009;20:1547–52.
Akarasereenont P, Chatsiricharoenkul S, Pongnarin P. Bioequivalence study of 1,500 mg glucosamine sulfate in Thai healthy volunteers. J Bioequiv Availab. 2012;4(6):91–5.
Shahine EM, Elhadidi AS. Efficacy of glucosamine sulfate in lowering serum level of interleukin-1b in symptomatic primary knee osteoarthritis: clinical and laboratory study. Alex J Med. 2014;50:159–63.
Nagaoka I, Igarashi M, Hua J, Ju Y, Yomogida S, Sakamoto K. Recent aspects of the anti-inflammatory actions of glucosamine. Carbohydr Polym. 2011;84:825–30.
Zhu YB, Zou JJ, Xiao DW, Fan HW, Yu CX, Zhang JJ, et al. Bioequivalence of two formulations of glucosamine sulfate 500-mg capsules in healthy male Chinese volunteers: an open-label, randomized-sequence, single-dose, fasting, two-way crossover study. Clin Ther. 2009;31(7):1551–8.
Bartels EM, Bliddaly H, Schøndorff PK, Altmank RD, Zhang W, Christensen R. Symptomatic efficacy and safety of diacerein in the treatment of osteoarthritis: a meta-analysis of randomized placebo-controlled trials. Osteoarthr Cartil. 2010;18:289–96.
Pavelka K, Trč T, Karpaš K, Vítek P, Sedláčková M, Vlasáková V, et al. The efficacy and safety of diacerein in the treatment of painful osteoarthritis of the knee: a randomized, multicenter,double-blind, placebo-controlled study with primary end points at two months after the end of a three-month treatment period. Arthritis Rheumatol. 2007;56:4055–64.
Kaur D, Kaur J, Kamal SS. Diacerein, its beneficial impact on chondrocytes and notable new clinical applications. Braz J Pharm Sci. 2019;54(4):e17534.
Kong M, Hashim KB, Lin P, Coestesquis G, Xu A, Lebes F, et al. Penetration of topical glucosamine sulfate into the synovial fluid of patients with knee osteoarthritis: a nonrandomized, open-label, single dose, bioavailability study. J Biosci Med. 2019;7(11):76–90.
Chattopadhyay H, Auddy B, Sur T, Sana S, Datta S. Accentuated transdermal application of glucosamine sulphate attenuates experimental osteoarthritis induced by monosodiumiodoacetate. J Mater Chem B. 2016;4:4470–81.
Aziza DE, Abdelbary AA, Elassasy AI. Fabrication of novel elastosomes for boosting the transdermal delivery of diacerein: statistical optimization, ex-vivo permeation, in-vivo skin deposition and pharmacokinetic assessment compared to oral formulation. Drug Deliv. 2018;25(1):815–26.
Gao Y, Cheng X, Wang Z, Wang J, Gao T, Li P, et al. Transdermal delivery of 10,11-methylenedioxycamptothecin by hyaluronic acid based nanoemulsion for inhibition of keloid fibroblast. Carbohydr Polym. 2014;112:376–86.
Kong M, Park HJ. Stability investigation of hyaluronic acid based nanoemulsion and its potential as transdermal carrier. Carbohydr Polym. 2011;83:1303–10.
Solans C, Esquena J, Forgiarini A, Morales D, Uśon N, Izquierdo P. Nanoemulsions: formation and properties. In: Shah D, Moudgil B, Mittal KL, editors. Surfactants in solution: fundamentals and applications, Surfactant Science Series. New York: Marcel Dekker; 2002. p. 525–54.
Sznitowska M, Janicki S, Dabrowska E, Zurowska-Pryczkowska K. Submicron emulsions as drug carriers: studies on destabilization potential of various drugs. European J Pharm Sci. 2001;12:175–9.
Mou D, Chen H, Du D, Mao C, Wan J, Xu H, et al. Hydrogel-thickened nanoemulsion system for topical delivery of lipophilic drugs. Int J Pharm. 2008;353:270–6.
Han G, Wang G, Zhu X, Shao H, Liu F, Yang P, et al. Preparation of xanthan gum injection and its protective effect on articular cartilage in the development of osteoarthritis. Carbohydr Polym. 2012;87:1837–42.
Yaron M, Shirazi I, Yaron I. Anti-interleukin-1 effects of diacerein and rhein in human osteoarthritic synovial tissue and cartilage cultures. Osteoarthr Cartil. 1999;7:272–80.
Toegel S, Wu SQ, Piana C, Unger FM, Wirth M, Goldring MB, et al. Comparison between chondroprotective effects of glucosamine, curcumin, and diacerein in IL-1beta-stimulated C-28/I2 chondrocytes. Osteoarthr Cartil. 2008;16:1205–12.
Kou L, Xiao S, Sun R, Bao S, Yao Q, Chen R. Biomaterial-engineered intra-articular drug delivery systems for osteoarthritis therapy. Drug Deliv. 2019;26(1):870–85.
Seok SH, Lee SA, Park ES. Formulation of a microemulsion-based hydrogel containing celecoxib. J Drug Deliv Sci Technol. 2018;43:409–14.
Manosroi A, Jantrawuta P, Manosroi J. Anti-inflammatory activity of gel containing novel elastic niosomes entrapped with diclofenac diethylammonium. Int J Pharm. 2008;360:156–63.
Jana S, Manna S, Nayak AK, Sen KK, Basu SK. Carbopol gel containing chitosan-egg albumin nanoparticles for transdermal aceclofenac delivery. Colloids Surf B Biointerfaces. 2014;114:36–44.
Sreejith KR, Premalatha K. Novel spectrophotometric methods for estimation of diacerein from formulations. IJRPBS. 2011;2:992–9.
Wu Y, Hussain M, Fassihi R. Development of a simple analytical methodology for determination of glucosamine release from modified release matrix tablets. J Pharmaceut Biomed. 2005;38:263–9.
Ahmed MS, Mamdouh MG, Shadeed GS, Eman AM. Formulation and evaluation of different transdermal drug delivery systems of ketoprofen. Int J Pharm Pharm Sci. 2013;5:600–7.
Patel J, Patel B, Banwait HS, Parmar K. Formulation and evaluation of topical aceclofenac gel using different gelling agent. Int J Drug Dev Res. 2011;3:156–64.
Shah PP, Desai PR, Patel AR, Singh MS. Skin permeating nanogel for the cutaneous co-delivery of two anti-inflammatory drugs. Biomaterials. 2012;33:1607–17.
Lee HS, Morrison E, Frethem C, Zasadzinski J, McCormick A. Cryogenic electron microscopy study of nanoemulsion formation from microemulsions. Langmuir. 2014;30:10826–33.
Malakar J, Sen SO, Nayak AK, Sen KK. Formulation, optimization and evaluation of transferosomal gel for transdermal insulin delivery. Saudi Pharm J. 2012;20:355–63.
Lee YM, Son E, Kim SH, Kim OS, Kim DS. Anti-inflammatory and anti-osteoarthritis effect of Mollugo pentaphylla extract. Pharm Biol. 2019;57(1):74–81.
Yamada EF, Salgueiro AF, Goulart ADS, Mendes VP, Anjos BL, Folmer V, et al. Evaluation of monosodium iodoacetate dosage to induce knee osteoarthritis: relation with oxidative stress and pain. Int J Rheum Dis. 2019;22(3):399–410.
Wen ZH, Tang CC, Chang YC, Huang SY, Hsieh SP, Lee CH, et al. Glucosamine sulphate reduces experimental osteoarthritis and nociception in rats: association with changes of mitogen-activated protein kinase in chondrocytes. Osteoarthr Cartil. 2010;18:1192–202.
Al-Saffar FJ, Ganabadi S, Yaakub H, Fakurazi S. Collagenase and sodium iodoacetate- induced experimental osteoarthritis model in Sprague Dawley rats. Asian J Sci Res. 2009;2:167–79.
Ahmed AS, Li J, Erlandsson-Harris H, Stark A, Bakalkin G, Ahmed M. Suppression of pain and joint destruction by inhibition of the proteasome system in experimental osteoarthritis. Pain. 2012;153:18–26.
Kuroda R, Usas A, Kubo S, Corsi K, Peng H, Rose T, et al. Cartilage repair using bone morphogenetic protein 4 and muscle-derived stem cells. Arthritis Rheum. 2006;54:433–42.
Daghestani HN, Kraus VB. Inflammatory biomarkers in osteoarthritis. Osteoarthr Cartil. 2015;23:1890–6.
Ley C, Ekman S, Ronéus B, Eloranta ML. Interleukin-6 and high mobility group box protein-1 in synovial membranes and osteochondral fragments in equine osteoarthritis. Res Vet Sci. 2009;86:490–7.
Miller RE, Miller RJ, Malfait AM. Osteoarthritis joint pain: the cytokine connection. Cytokine. 2014;70:185–93.
Pearle AD, Scanzello CR, George SS, Mandl L, DiCarlo EF, Crow MK, et al. Elevated C-reactive protein levels in osteoarthritis are associated with local joint inflammation. Arthritis Res Ther. 2004;6(Suppl3):56.S23–4.
Feng Y, Fang W, Li C, Guo H, Li Y, Long X. The expression of high-mobility group box protein-1 in temporomandibular joint osteoarthritis with disc perforation. J Oral Pathol Med. 2016;45:148–52.
Sun L, Wang X, Kaplan DL. A 3D cartilage - inflammatory cell culture system for the modeling of human osteoarthritis. Biomaterials. 2011;32:5581–9.
Xu YK, Ke Y, Wang B, Lin JH. The role of MCP-1-CCR2 ligand-receptor axis in chondrocyte degradation and disease progress in knee osteoarthritis. Biol Res. 2015;48:64–71.
Yilmaz E, Borchert HH. Effect of lipid-containing, positively charged nanoemulsions on skin hydration, elasticity and erythema—an in vivo study. Int J Pharm. 2006;307:232–8.
Antunes FE, Coppola L, Rossi CO, Ranieri GA. Gelation of charged bio-nanocompartments induced by associative and non-associative polysaccharides. Colloids Surf B Biointerfaces. 2008;66:134–40.
Liu W, Hu M, Liu W, Xue C, Xu H, Yang X. Investigation of the carbopol gel of solid lipid nanoparticles for the transdermal iontophoretic delivery of triamcinolone acetonide acetate. Int J Pharm. 2008;364:135–41.
Peltola S, Saarinen-Savolainen P, Kiesvaara J, Suhonen TM, Urtti A. Microemulsions for topical delivery of estradiol. Int J Pharm. 2003;254:99–107.
Hu XB, Kang RR, Tang TT, et al. Topical delivery of 3,5,4′-trimethoxy-trans-stilbene-loaded microemulsion-based hydrogel for the treatment of osteoarthritis in a rabbit model. Drug Deliv and Transl Res. 2019;9:357–65.
Kongtharvonskul J, Woratanarat P, McEvoy M, Attia J, Wongsak S, Kawinwonggowit V, et al. Efficacy of glucosamine plus diacerein versus monotherapy of glucosamine: a double-blind, parallel randomized clinical trial. Arthritis Res Ther. 2016;18:233,1–12.
Mirunalini R, Manimekalai K, Chandrasekaran M. Comparative evaluation of symptom relief and disease modifying effect of chondroitin with glucosamine sulfate and diacerein in osteoarthritis knee. SBV J Basic Clin Appl Health Sci. 2018;2(1):12–5.
Nganvongpanit K, Boonsri B, Sripratak T, Markmee P, Kongtawelert P. Clinical study on the effects of diacerein and diacerein combined with chondroitin sulfate on canine hip osteoarthritis. Kafkas Univ Vet Fak Derg. 2014;20(3):383–92.
Acknowledgments
The authors are grateful to CRNN campus of University of Calcutta for carrying out the Cryo-SEM and TEM analyses.
Funding
This work has been funded by the DST INSPIRE fund (DST/ INSPIRE FELLOWSHIP/2012/575) and supported by the Department of Chemical Technology, C.U.
Author information
Authors and Affiliations
Contributions
H.C. and S.D. conceived and designed the research. H.C. performed the formulation work. H.C., S.D., B.A., and T.S. designed and performed the animal study. M.G. provided animal ethics approval and facilities for in vivo studies. H.C., S.D., B.A., and T.S. analyzed and interpreted the results. H.C. wrote the manuscript, and S.D. edited the manuscript. All authors discussed the results and commented on the manuscript. All authors have given approval to the final version of the manuscript.
Corresponding author
Ethics declarations
The protocol of the experimental design was approved by the Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA), Government of India, and by the Institutional Animal Ethics Committee (Registration no. 1180/ac/08/CPCSEA).
Conflict of interest
The authors declare that they have no conflict of interest
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chattopadhyay, H., Auddy, B., Sur, T. et al. Transdermal co-delivery of glucosamine sulfate and diacerein for the induction of chondroprotection in experimental osteoarthritis. Drug Deliv. and Transl. Res. 10, 1327–1340 (2020). https://doi.org/10.1007/s13346-019-00701-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-019-00701-7