Abstract
Introduction
Insulin degludec (degludec) is a basal insulin with a long duration of action. This post-marketing surveillance study monitored safety and glycemic control during use of degludec for 3 years in normal clinical practice in Japan.
Materials and methods
This multicenter, open-label, observational study included patients with diabetes receiving degludec in Japan between 2013 and 2019. The primary outcome was incidence of adverse events occurring over 3 years of treatment. The pre-specified, secondary outcomes were severe hypoglycemic episodes and changes in HbA1c and fasting plasma glucose levels.
Results
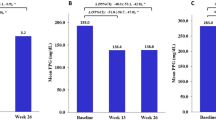
Of 4167 patients enrolled, 4022 were included in the safety assessments and 3918 in the assessments of glycemic control. Mean age was 58.9 years; 74.1% of patients had type 2 diabetes, and mean HbA1c at baseline was 8.7%. Adverse events and serious adverse events were observed in 19.1% and 8.9% of patients, respectively. Cardiac disorders and neoplasms were reported in 2.0% and 1.8% of patients, respectively, with the majority of these incidents reported as serious adverse events. Adverse drug reactions were seen in 8.0% of patients, mainly hypoglycemia. Hypoglycemic events were observed in 5.6% of patients, and severe hypoglycemic events in 1.7%. No serious allergic or injection-site reactions were seen. Respective changes (from baseline to 3 years’ observation) in HbA1c and fasting plasma glucose levels were − 0.55% and − 36.3 mg/dL, and 19.6% of patients reached HbA1c < 7.0%.
Conclusions
Using degludec for 3 years in normal clinical practice had a good safety and tolerability profile. Improvements in glycemic control were also seen.

Similar content being viewed by others
Data availability
The data analyzed during the current study are available from the corresponding author on reasonable request.
References
Mathieu C, Gillard P, Benhalima K. Insulin analogues in type 1 diabetes mellitus: getting better all the time. Nat Rev Endocrinol. 2017;13(7):385–99.
Tibaldi JM. Evolution of insulin: from human to analog. Am J Med. 2014;127(10 Suppl):S25-38.
Heise T, Hermanski L, Nosek L, Feldman A, Rasmussen S, Haahr H. Insulin degludec: four times lower pharmacodynamic variability than insulin glargine under steady-state conditions in type 1 diabetes. Diabetes Obes Metab. 2012;14(9):859–64.
Goldenberg RM, Aroda VR, Billings LK, Christiansen ASL, Meller Donatsky A, Parvaresh Rizi E, et al. Effect of insulin degludec versus insulin glargine U100 on time in range: SWITCH PRO, a crossover study of basal insulin-treated adults with type 2 diabetes and risk factors for hypoglycaemia. Diabetes Obes Metab. 2021;23(11):2572–81.
Yamamoto C, Miyoshi H, Fujiwara Y, Kameda R, Ichiyama M, Nomoto H, et al. Degludec is superior to glargine in terms of daily glycemic variability in people with type 1 diabetes mellitus. Endocr J. 2016;63(1):53–60.
Liu W, Yang X, Huang J. Efficacy and safety of insulin degludec versus insulin glargine: a systematic review and meta-analysis of fifteen clinical trials. Int J Endocrinol. 2018;2018:8726046.
Preumont V, Buysschaert M. Current status of insulin degludec in type 1 and type 2 diabetes based on randomized and observational trials. Diabetes Metab. 2020;46(2):83–8.
Thuillier P, Alavi Z, Kerlan V. Long-term safety and efficacy of insulin degludec in the management of type 2 diabetes. Diabetes Metab Syndr Obes. 2015;8:483–93.
Zhou W, Tao J, Zhou X, Chen H. Insulin degludec, a novel ultra-long-acting basal insulin versus insulin glargine for the management of type 2 diabetes: a systematic review and meta-analysis. Diabetes Ther. 2019;10(3):835–52.
Dongerkery SP, Schroeder PR, Shomali ME. Insulin and its cardiovascular effects: what is the current evidence? Curr Diab Rep. 2017;17(12):120.
Jensen MH, Hejlesen O, Vestergaard P. Risk of major cardiovascular events, severe hypoglycaemia, and all-cause mortality for users of insulin degludec versus insulin glargine U100-A Danish cohort study. Diabetes Metab Res Rev. 2020;36(1): e3225.
Neugebauer R, Schroeder EB, Reynolds K, Schmittdiel JA, Loes L, Dyer W, et al. Comparison of mortality and major cardiovascular events among adults with type 2 diabetes using human vs analogue insulins. JAMA Netw Open. 2020;3(1): e1918554.
Pratley RE, Emerson SS, Franek E, Gilbert MP, Marso SP, McGuire DK, et al. Cardiovascular safety and lower severe hypoglycaemia of insulin degludec versus insulin glargine U100 in patients with type 2 diabetes aged 65 years or older: Results from DEVOTE (DEVOTE 7). Diabetes Obes Metab. 2019;21(7):1625–33.
Yang CT, Li KY, Yang CY, Ou HT, Kuo S. A nationwide cohort study for comparative vascular safety of long-acting insulin analogue versus intermediate-acting human insulin in type 2 diabetes. Sci Rep. 2021;11(1):4152.
Baricevic I, Jones DR, Roberts DL, Lutzen A, Lundby A, Worm J, et al. A framework for the in vitro evaluation of cancer-relevant molecular characteristics and mitogenic potency of insulin analogues. Carcinogenesis. 2015;36(9):1040–50.
Sciacca L, Vella V, Frittitta L, Tumminia A, Manzella L, Squatrito S, et al. Long-acting insulin analogs and cancer. Nutr Metab Cardiovasc Dis. 2018;28(5):436–43.
Vigneri R, Sciacca L, Vigneri P. Rethinking the relationship between insulin and cancer. Trends Endocrinol Metab. 2020;31(8):551–60.
Wu JW, Filion KB, Azoulay L, Doll MK, Suissa S. Effect of long-acting insulin analogs on the risk of cancer: a systematic review of observational studies. Diabetes Care. 2016;39(3):486–94.
Tajima N, Noda M, Origasa H, Noto H, Yabe D, Fujita Y, et al. Evidence-based practice guideline for the treatment for diabetes in Japan 2013. Diabetol Int. 2015;6(3):151–87.
Machin D, Campbell M, Tan S, Tan S. Sample size tables for clinical studies. 3rd ed. Oxford: Wiley Blackwell Publications; 2009. p. 142–52.
Marso SP, McGuire DK, Zinman B, Poulter NR, Emerson SS, Pieber TR, et al. Efficacy and safety of degludec versus glargine in type 2 diabetes. N Engl J Med. 2017;377(8):723–32.
Kaku K, Wolden ML, Hyllested-Winge J, Nørtoft E. Insulin degludec in clinical practice: a review of Japanese real-world data. Diabetes Ther. 2017;8(1):189–95.
Acknowledgements
The authors would like to thank all the study investigators and coordinators. Medical writing and editorial support for the development of this manuscript, under the direction of the authors, were provided by Patrick Hoggard, PhD, and Helen Marshall, BA, of Ashfield MedComms, an Inizio company, and funded by Novo Nordisk A/S. Novo Nordisk A/S participated in the study design, site selection, study coordination, data management, data analysis, and study report preparation.
Funding
Novo Nordisk A/S funded this study.
Author information
Authors and Affiliations
Contributions
TM, LLNH, SN, and MM all fulfil the International Committee of Medical Journal Editors (ICMJE) criteria for authorship. The study was conceptualized, designed, and conducted by employees of Novo Nordisk not in the author list. Authors LLNH and SN were involved in the analysis of the data. TM, LLNH, SN, and MM were involved in data interpretation and the development and critical review of each draft, and all approve the final version to be published.
Corresponding author
Ethics declarations
Conflict of interest
Takashi Murata has received honoraria from Eli Lilly Japan, Sanofi, Kowa Pharmaceutical, Novo Nordisk, Kyowa Kirin, and Takeda Pharmaceutical; and grants from Sanofi and Kowa Pharmaceutical. Lise Lotte N. Husemoen and Satoko Nemoto are employed by Novo Nordisk. Munehide Matsuhisa has received honoraria from Sanofi, Takeda Pharmaceutical, Eli Lilly Japan, Mitsubishi Tanabe Pharma Corporation, Astellas Pharma, Novo Nordisk, Orizuru Therapeutics, Sumitomo Pharma, Abbott Japan, and MSD; research funding from Sysmex, Nissui, and Tokushima Data Service; and subsidies or donations from Astellas Pharma, Nippon Boehringer Ingelheim, Daiichi Sankyo, Mitsubishi Tanabe Pharma, Novartis, Sanofi, Novo Nordisk, Takeda Pharmaceutical, MSD, and Ono Pharmaceutical.
Ethical approval
The study was conducted according to requirements of the revised Declaration of Helsinki, the Guidelines for Good Pharmacoepidemiology Practices, the Japanese Ministry of Health, Labour and Welfare Notification No. 171, “Ordinance Concerning the Standards for Conducting Post-Marketing Surveys and Studies on Drugs”, and the Japanese Ministry of Health, Labour and Welfare Notification No. 135, “Ordinance Concerning the Standards for Post-Marketing Safety Management of Drugs, Medical Devices, Cosmetics and Medical Devices” (GVP; issued 22 September 2004). The protocol and any amendments were approved at each investigator site, as required locally. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and/or with the Helsinki Declaration of 1964 and later versions.
Informed consent
All participants or legally acceptable representatives (for children) provided written informed consent. Prior to study-related activities and commencement of degludec, the physician had to provide written and oral study information to the patient/representative to be read and understood.
Approval date of registry and the registration no. of the study/trial
This study was pre-registered to ensure transparency and minimize selective reporting bias. The first submitted date was 07 November 2013 and the first posted date was 14 November 2013. The ClinicalTrials.gov registration number is NCT01984372.
Animal studies
N/A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Murata, T., Husemoen, L.L.N., Nemoto, S. et al. Safety and glycemic control with insulin degludec use in clinical practice: results from a 3-year Japanese post-marketing surveillance study. Diabetol Int 15, 76–85 (2024). https://doi.org/10.1007/s13340-023-00657-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-023-00657-7