Abstract
Background
Many patients with type 2 diabetes (T2DM) suffer from diabetic peripheral neuropathy (DPN) and impaired muscle coordination. These changes may lead to walking instability, and gait abnormalities resulting in increased fall risk and lower limb amputations. The aim of this study was to assess the impact of DPN and patient footwear on the gait in patients with diabetes, in addition to Comparing the peak plantar pressure (PPP) in patients with and without DPN and assessing its association with gait abnormalities.
Methodology
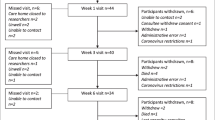
This is an observational case–control study. Forty Subjects with T2DM were divided into two age and sex-matched groups, 20 subjects each. Group A: subjects with DPN. Group B: subjects without DPN. All study participants were subjected to a thorough history taking, clinical examinations focusing on detailed foot examination, PPP assessment, and functional gait evaluation.
Results
The results obtained in this study showed a median gait assessment score of 21 (17.0–22.5) for group A and 26 (23.5–26.0) for group B which was statistically significant (p < 0.001). There was no statistically significant difference between both groups (p > 0.05) regarding the assessment of footwear appropriateness. Comparing the PPP measurement among both studied groups, the prevalence of an elevated PPP was 80% in group A compared to 65% in group B, which was statistically non-significant, p = 0.288.
Conclusions
Gait abnormalities are common among patients with T2DM even in the absence of DPN. However, the presence of DPN was the strongest independent risk factor for gait abnormalities among the studied factors.
Similar content being viewed by others
Data availability
Data is available through the corresponding author upon justified request.
Abbreviations
- ACAD:
-
Atherosclerotic coronary artery disease
- BMI:
-
Body mass index
- DNS:
-
Diabetic neuropathy symptom score
- DPN:
-
Diabetic peripheral neuropathy
- DSPN:
-
Distal symmetric polyneuropathy
- FGA:
-
Functional gait assessment
- HbA1c:
-
Glycosylated hemoglobin
- PPP:
-
Peak plantar pressure
- T2DM:
-
Type 2 diabetes
- VPT:
-
Vibration perception threshold
References
IDF Diabetes Atlas 9th edition 2019 [Internet]. Diabetesatlas.org. 2021. Available from: https://diabetesatlas.org/en/. Accessed 26 Oct 2021
Assaad Khalil SH, Megallaa MH, Rohoma KH, Ismael H, AbouSeif M, Kharboush I, Elkaffash D, Hassanein M, Wahab MM, Malaty A, Sallam H. Prevalence of type 2 diabetes mellitus in a sample of the adult population of Alexandria. Egypt Diabetes Res Clin Pract. 2018;1(144):63–73.
Elmadhoun WM, Noor SK, Ibrahim AA, Bushara SO, Ahmed MH. Prevalence of diabetes mellitus and its risk factors in urban communities of north Sudan: population-based study. J Diabetes. 2016;8(6):839–46.
Noor SK, Bushara SO, Sulaiman AA, Elmadhoun WM, Ahmed MH. Undiagnosed diabetes mellitus in rural communities in Sudan: prevalence and risk factors. East Mediterr Health J. 2015;21(3):164–70.
Noor SK, Elmadhoun WM, Bushara SO, Almobarak AO, Salim RS, Forawi SA, et al. Glycaemic control in Sudanese individuals with type 2 diabetes: population based study. Diabetes Metab Syndr. 2017;11(Suppl 1):S147-151.
Amin N, Doupis J. Diabetic foot disease: from the evaluation of the “foot at risk” to the novel diabetic ulcer treatment modalities. World J Diabetes. 2016;7(7):153–216. https://doi.org/10.4239/wjd.v7.i7.153.
Khanolkar MP, Bain SC, Stephens JW. The diabetic foot. QJM. 2008;101(9):685–95.
Edmonds M, Manu C, Vas P. The current burden of diabetic foot disease. J Clin Orthop Trauma. 2021;17:88–93. https://doi.org/10.1016/j.jcot.2021.01.017.
Bartus CL, Margolis DJ. Reducing the incidence of foot ulceration and amputation in diabetes. Curr Diab Rep. 2004;4(6):413–8.
Bus SA, Maas M, de Lange A, Michels RP, Levi M. Elevated plantar pressures in neuropathic diabetic patients with claw/hammer toe deformity. J Biomech. 2005;38(9):1918–25.
Payne C, Turner D, Miller K. Determinants of plantar pressures in the diabetic foot. J Diabetes Complic. 2002;16(4):277–83.
Fernando DJ, Masson EA, Veves A, Boulton AJ. Relationship of limited joint mobility to abnormal foot pressures and diabetic foot ulceration. Diabetes Care. 1991;14(1):8–11.
Cavanagh PR, Ulbrecht JS. Biomechanics of the diabetic foot: a quantitative approach to the assessment of neuropathy, deformity and plantar pressure. In: Cavanagh PR, Ulbrecht JS, editors. Disorders of the foot and ankle: medical and surgical management, vol. 2. Philadelphia: Saunders; 1991. p. 1864–907.
Kwon OY, Minor SD, Maluf KS, Mueller MJ. Comparison of muscle activity during walking in subjects with and without diabetic neuropathy. Gait Posture. 2003;18(1):105–13.
Mueller MJ, Minor SD, Sahrmann SA, Schaaf JA, Strube MJ. Differences in the gait characteristics of patients with diabetes and peripheral neuropathy compared with age-matched controls. Phys Ther. 1994;74(4):299–308.
Maluf KS, Mueller MJ, Strube MJ, Engsberg JR, Johnson JE. Tendon Achilles lengthening for the treatment of neuropathic ulcers causes a temporary reduction in forefoot pressure associated with changes in plantar flexor power rather than ankle motion during gait. J Biomech. 2004;37(6):897–906.
Shaw JE, Van Schie CH, Carrington AL, Abbott CA, Boulton AJ. An analysis of dynamic forces transmitted through the foot in diabetic neuropathy. Diabetes Care. 1998;21(11):1955–9.
Sacco ID, Amadio AC. Influence of the diabetic neuropathy on the behavior of electromyographic and sensorial responses in treadmill gait. Clin Biomech. 2003;18(5):426–34.
Andersen H. Motor dysfunction in diabetes. Diabetes Metab Res Rev. 2012;28(Suppl 1):89–92.
Van Deursen R. Mechanical loading and off-loading of the plantar surface of the diabetic foot. Clin Infect Dis. 2004;39:S87-91.
Hazari A, Maiya AG, Shivashankara KN, Agouris I, Monteiro A, Jadhav R, et al. Kinetics and kinematics of diabetic foot in type 2 diabetes mellitus with and without peripheral neuropathy: a systematic review and meta-analysis. Springerplus. 2016;5(1):1819.
Fernando M, Crowther R, Lazzarini P, Sangla K, Cunningham M, Buttner P, et al. Biomechanical characteristics of peripheral diabetic neuropathy: a systematic review and meta-analysis of findings from the gait cycle, muscle activity and dynamic barefoot plantar pressure. Clin Biomech. 2013;28(8):831–45.
Fernando ME, Crowther RG, Pappas E, Lazzarini PA, Cunningham M, Sangla KS, et al. Plantar pressure in diabetic peripheral neuropathy patients with active foot ulceration, previous ulceration and no history of ulceration: a meta-analysis of observational studies. PLoS One. 2014;9(6): e99050.
Wrisley DM, Marchetti GF, Kuharsky DK, Whitney SL. Reliability, internal consistency, and validity of data obtained with the functional gait assessment. Phys Ther. 2004;84(10):906–18.
Mann RW. The role of impact forces and foot pronation: a new paradigm. Clin J Sport Med. 2002;12(1):57–8.
Firestine SM, Poon SW, Mueller EJ, Stubbe J, Davisson VJ. Reactions catalyzed by 5-aminoimidazole ribonucleotide carboxylases from Escherichia coli and Gallus gallus: a case for divergent catalytic mechanisms? Biochem. 1994;33(39):11927–34.
Sacco ID, Amadio AC. A study of biomechanical parameters in gait analysis and sensitive cronaxie of diabetic neuropathic patients. Clin Biomech. 2000;15(3):196–202.
Salsich GB, Mueller MJ, Sahrmann SA. Passive ankle stiffness in subjects with diabetes and peripheral neuropathy versus an age-matched comparison group. Phys Ther. 2000;80(4):352–62.
Menz HB, Latt MD, Tiedemann A, San Kwan MM, Lord SR. Reliability of the GAITRite® walkway system for the quantification of temporo-spatial parameters of gait in young and older people. Gait Posture. 2004;20(1):20–5.
Marathe PH, Gao HX, Close KL. American diabetes association standards of medical care in diabetes 2017. J diabetes. 2017;9(4):320–4.
Keutmann S, Zylla S, Dahl M, Friedrich N, Landgraf R, Heinemann L, Kallner A, Nauck M, Petersmann A. Measurement uncertainty impacts diagnosis of diabetes mellitus: reliable minimal difference of plasma glucose results. Diabetes Ther. 2020;11(1):293–303.
Gorman BS, Primavera LH, Allison DB. POWPAL: a program for estimating effect sizes, statistical power, and sample sizes. Educ psychol meas. 1995;55(5):773–6.
American Diabetes Association. 3. Comprehensive medical evaluation and assessment of comorbidities: standards of medical care in diabetes—2018. Diabetes Care. 2018;41(suppl1):S28–37.
Garrow AP, Boulton AJ. Vibration perception threshold—a valuable assessment of neural dysfunction in people with diabetes. Diabetes Metab Res Rev. 2006;22:411–9.
Shillo P, Sloan G, Greig M, Hunt L, Selvarajah D, Elliott J, Gandhi R, Wilkinson ID, Tesfaye S. Painful and painless diabetic neuropathies: what is the difference? Curr Diab Rep. 2019;19(6):32.
Meijer JW, Smit AJ, Sonderen EV, Groothoff JW, Eisma WH, Links TP. Symptom scoring systems to diagnose distal polyneuropathy in diabetes: the diabetic neuropathy symptom score. Diabet Med. 2002;19(11):962–5.
Vernon W, Parry A, Potter M. A theory of shoe wear pattern influence incorporating a new paradigm for the podiatric medical profession. J Am Podiatr Med Assoc. 2004;94(3):261–8.
Bus SA, de Lange A. A comparison of the 1-step, 2-step, and 3-step protocols for obtaining barefoot plantar pressure data in the diabetic neuropathic foot. Clin Biomech. 2005;20:892–9.
Assaad-Khalil SH, Zaki A, Rehim AA, Megallaa MH, Gaber N, Gamal H, Rohoma KH. Prevalence of diabetic foot disorders and related risk factors among Egyptian subjects with diabetes. Prim Care Diabetes. 2015;9(4):297–303.
Jiang X, Deng F, Rui S, Ma Y, Wang M, Deng B, Wang H, Du C, Chen B, Yang X, Boey J, Armstrong DG, Deng W, Duan X. The evaluation of gait and balance for patients with early diabetic peripheral neuropathy: a cross-sectional study. Risk Manag Healthc Policy. 2022;30(15):543–52. https://doi.org/10.2147/RMHP.S361698.
Stegemöller EL, Buckley TA, Pitsikoulis C, Barthelemy E, Roemmich R, Hass CJ. Postural instability and gait impairment during obstacle crossing in Parkinson’s disease. Arch Phys Med Rehabil. 2012;93(4):703–9.
Almurdhi MM, Brown SJ, Bowling FL, Boulton AJ, Jeziorska M, Malik RA, Reeves ND. Altered walking strategy and increased unsteadiness in participants with impaired glucose tolerance and type 2 diabetes relates to small-fibre neuropathy but not vitamin D deficiency. Diabet Med. 2017;34(6):839–45.
AlAyed MY, Younes N, Al-Smady M, Khader YS, Robert AA, Ajlouni K. Prevalence of foot ulcers, foot at risk and associated risk factors among jordanian diabetics. Curr Diabetes Rev. 2017;13(2):182–91.
Akashi PM, Sacco IC, Watari R, Hennig E. The effect of diabetic neuropathy and previous foot ulceration in EMG and ground reaction forces during gait. Clin Biomech. 2008;23(5):584–92.
Qiu X, Tian DH, Han CL, Chen W, Wang ZJ, Mu ZY, Liu KZ. Plantar pressure changes and correlating risk factors in Chinese patients with type 2 diabetes: preliminary 2-year results of a prospective study. Chin Med J. 2015;128(24):3283.
Syed N, Maiya AG, Hanifa N, Goud S. Plantar pressures in diabetes with no known neuropathy. J diabetes. 2013;5(3):302–8.
Halawa MR, Eid YM, El-Hilaly RA, Abdelsalam MM, Amer AH. Relationship of plantar pressure and glycemic control in type 2 diabetic patients with and without neuropathy. Diabetes Metab Syndr. 2018;12(2):99–104.
Sacco IC, Hamamoto AN, Tonicelli LM, Watari R, Ortega NR, Sartor CD. Abnormalities of plantar pressure distribution in early, intermediate, and late stages of diabetic neuropathy. Gait Posture. 2014;40(4):570–4.
Funding
The authors did not receive support from any organization for the submitted work. No funding was received to assist with the preparation of this manuscript. No funding was received for conducting this study. No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to all the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. The authors have no competing interests to declare that are relevant to the content of this article. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Ethical approval
The study design was approved by the ethics committee of Alexandria University. The study followed the criteria set by the declaration of Helsinki. Confidentiality and personal privacy were respected at all levels of the study. IRB approval number is 0106242 dated 16/JAN/2020.
Informed consent
The participating study population signed an informed consent before any study-related procedure took place. Patients felt free to withdraw from the study at any time without any consequences. Participants also signed an additional consent for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Khalil, S.H.A., Deeb, H.M.A.E., Ajang, M.O.D. et al. Impact of diabetic peripheral neuropathy on gait abnormalities in patients with type 2 diabetes mellitus. Diabetol Int 15, 58–66 (2024). https://doi.org/10.1007/s13340-023-00652-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-023-00652-y