Abstract
Aim
The incidence of cardiovascular and renal events was investigated in patients with type 2 diabetes who were classified according to anemia and the components of dialysis-independent chronic kidney disease (CKD) in a prospective observational study.
Methods
A population of 778 Japanese patients with type 2 diabetes was prospectively analyzed for 4 years. The outcomes were the incidence of cardiovascular events and renal events.
Results
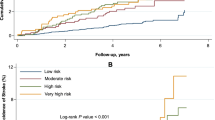
In all subjects, the incidence of cardiovascular and renal events was found to be 5% and 11%, respectively. Even after adjusting for a reduced estimated glomerular filtration rate (eGFR <60 mL/min/1.73 m2), the incidence of cardiovascular events was significantly higher (hazard ratio [HR]: 5.73) in patients with anemia and albuminuria than in those without anemia and albuminuria. The incidence of renal events was significantly higher in patients with no anemia and albuminuria (HR: 2.93) and further in those with anemia and albuminuria (HR: 7.56) than in those without anemia and albuminuria even after adjusting for a reduced eGFR.
Conclusion
Anemia combined with albuminuria is a risk factor for vascular events in patients with type 2 diabetes, regardless of the eGFR.




Similar content being viewed by others
References
Anand I, McMurray JJ, Whitmore J, Warren M, Pham A, McCamish MA, et al. Anemia and its relationship to clinical outcome in heart failure. Circulation. 2004;110:149–54. https://doi.org/10.1161/01.CIR.0000134279.79571.73.
Vlagopoulos PT, Tighiouart H, Weiner DE, Griffith J, Pettitt D, Salem DN, et al. Anemia as a risk factor for cardiovascular disease and all-cause mortality in diabetes: the impact of chronic kidney disease. J Am Soc Nephrol. 2005;16:3403–10. https://doi.org/10.1681/ASN.2005030226.
Mohanram A, Zhang Z, Shahinfar S, Keane WF, Brenner BM, Toto RD. Anemia and end-stage renal disease in patients with type 2 diabetes and nephropathy. Kidney Int. 2004;66:1131–8. https://doi.org/10.1111/j.1523-1755.2004.00863.x.
Yamamoto T, Miyazaki M, Nakayama M, Yamada G, Matsushima M, Sato M, et al. Impact of hemoglobin levels on renal and non-renal clinical outcomes differs by chronic kidney disease stages: the Gonryo study. Clin Exp Nephrol. 2016;20:595–602. https://doi.org/10.1007/s10157-015-1190-3.
Go AS, Yang J, Ackerson LM, Lepper K, Robbins S, Massie BM, et al. Hemoglobin level, chronic kidney disease, and the risks of death and hospitalization in adults with chronic heart failure: the Anemia in Chronic Heart Failure: outcomes and Resource Utilization (ANCHOR) Study. Circulation. 2006;113:2713–23. https://doi.org/10.1161/CIRCULATIONAHA.105.577577.
Silverberg D, Wexler D, Blum M, Wollman Y, Iaina A. The cardio-renal anaemia syndrome: does it exist? Nephrol Dial Transplant. 2003;18(Suppl 8):viii7-12. https://doi.org/10.1093/ndt/gfg1084.
Thomas MC, MacIsaac RJ, Tsalamandris C, Power D, Jerums G. Unrecognized anemia in patients with diabetes: a cross-sectional survey. Diabetes Care. 2003;26:1164–9. https://doi.org/10.2337/diacare.26.4.1164.
Akizawa T, Makino H, Matsuo S, Watanabe T, Imai E, Nitta K, et al. Management of anemia in chronic kidney disease patients: baseline findings from Chronic Kidney Disease Japan Cohort Study. Clin Exp Nephrol. 2011;15:248–57. https://doi.org/10.1007/s10157-010-0396-7.
Joss N, Patel R, Paterson K, Simpson K, Perry C, Stirling C. Anaemia is common and predicts mortality in diabetic nephropathy. QJM. 2007;100:641–7. https://doi.org/10.1093/qjmed/hcm080.
Loutradis C, Skodra A, Georgianos P, Tolika P, Alexandrou D, Avdelidou A, et al. Diabetes mellitus increases the prevalence of anemia in patients with chronic kidney disease: a nested case-control study. World J Nephrol. 2016;5:358–66. https://doi.org/10.5527/wjn.v5.i4.358.
Palaka E, Grandy S, van Haalen H, McEwan P, Darlington O. The impact of CKD anaemia on patients: incidence, risk factors, and clinical outcomes—A systematic literature review. Int J Nephrol. 2020;2020:7692376. https://doi.org/10.1155/2020/7692376.
Deray G, Heurtier A, Grimaldi A, Launay Vacher V, Isnard BC. Anemia and diabetes. Am J Nephrol. 2004;24:522–6. https://doi.org/10.1159/000081058.
Mehdi U, Toto RD. Anemia, diabetes, and chronic kidney disease. Diabetes Care. 2009;32:1320–6. https://doi.org/10.2337/dc08-0779.
Ito H, Antoku S, Furusho M, Shinozaki M, Abe M, Mifune M, et al. The prevalence of the risk factors for atherosclerosis among type 2 diabetic patients is greater in the progressive stages of chronic kidney disease. Nephron Extra. 2013;3:66–72. https://doi.org/10.1159/000353592.
Ito H, Takeuchi Y, Ishida H, Otawa A, Shibayama A, Antoku S, et al. Mild anemia is frequent and associated with micro- and macroangiopathies in patients with type 2 diabetes mellitus. J Diabetes Investig. 2010;1:273–8. https://doi.org/10.1111/j.2040-1124.2010.00060.x.
Tong PC, Kong AP, So WY, Ng MH, Yang X, Ng MC, et al. Hematocrit, independent of chronic kidney disease, predicts adverse cardiovascular outcomes in Chinese patients with type 2 diabetes. Diabetes Care. 2006;29:2439–44. https://doi.org/10.2337/dc06-0887.
Zoppini G, Targher G, Chonchol M, Negri C, Stoico V, Pichiri I, et al. Anaemia, independent of chronic kidney disease, predicts all-cause and cardiovascular mortality in type 2 diabetic patients. Atherosclerosis. 2010;210:575–80. https://doi.org/10.1016/j.atherosclerosis.2009.12.008.
Levin A, Djurdjev O, Duncan J, Rosenbaum D, Werb R. Haemoglobin at time of referral prior to dialysis predicts survival: an association of haemoglobin with long-term outcomes. Nephrol Dial Transplant. 2006;21:370–7. https://doi.org/10.1093/ndt/gfi209.
Ito H, Yamashita H, Nakashima M, Takaki A, Yukawa C, Matsumoto S, et al. Current metabolic status affects urinary liver-type fatty-acid binding protein in normoalbuminuric patients with type 2 diabetes. J Clin Med Res. 2017;9:366–73. https://doi.org/10.14740/jocmr2934w.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–28. https://doi.org/10.1056/NEJMoa1504720.
Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016;375:323–34. https://doi.org/10.1056/NEJMoa1515920.
Ito H, Matsumoto S, Izutsu T, Kusano E, Kondo J, Inoue H, et al. Different renoprotective effects of luseogliflozin depend on the renal function at the baseline in patients with type 2 diabetes: a retrospective study during 12 months before and after initiation. PLoS One. 2021;16:e0248577. https://doi.org/10.1371/journal.pone.0248577.
Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375:311–22. https://doi.org/10.1056/NEJMoa1603827.
Locatelli F, Covic A, Eckardt KU, Wiecek A, Vanholder R, ERA-EDTA ERBP Advisory Board. Anaemia management in patients with chronic kidney disease: a position statement by the Anaemia Working Group of European Renal Best Practice (ERBP). Nephrol Dial Transplant. 2009;24:348–54. https://doi.org/10.1093/ndt/gfn653.
KDOQI, National Kidney Foundation. KDOQI clinical practice guidelines and clinical practice recommendations for anemia in chronic kidney disease. Am J Kidney Dis. 2006;47(5 Suppl 3):S11-145. https://doi.org/10.1053/j.ajkd.2006.03.010.
Examination Committee of Criteria for ‘Obesity Disease’ in Japan, Japan Society for the Study of Obesity. New criteria for ‘obesity disease’ in Japan. Circ J. 2002;66:987–92. https://doi.org/10.1253/circj.66.987.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92. https://doi.org/10.1053/j.ajkd.2008.12.034.
Yamamoto H, Nishi S, Tomo T, Masakane I, Saito K, Nangaku M, et al. 2015 Japanese Society for Dialysis Therapy: guidelines for renal anemia in chronic kidney disease. Ren Replace Ther. 2017;3:36. https://doi.org/10.1186/s41100-017-0114-y.
Ninomiya T, Perkovic V, de Galan BE, Zoungas S, Pillai A, Jardine M, Advance Collaborative Group, et al. Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J Am Soc Nephrol. 2009;20:1813–21. https://doi.org/10.1681/ASN.2008121270.
Tanaka N, Babazono T, Takagi M, Yoshida N, Toya K, Nyumura I, et al. Albuminuria and reduced glomerular filtration rate for predicting the renal outcomes in type 2 diabetic patients. Nephrology (Carlton). 2015;20:531–8. https://doi.org/10.1111/nep.12446.
Moriya T, Suzuki Y, Inomata S, Iwano M, Kanauchi M, Haneda M. Renal histological heterogeneity and functional progress in normoalbuminuric and microalbuminuric Japanese patients with type 2 diabetes. BMJ Open Diabetes Res Care. 2014;2:e000029. https://doi.org/10.1136/bmjdrc-2014-000029.
Shimizu M, Furuichi K, Toyama T, Kitajima S, Hara A, Kitagawa K, Kanazawa Study Group for Renal Diseases and Hypertension, et al. Long-term outcomes of Japanese type 2 diabetic patients with biopsy-proven diabetic nephropathy. Diabetes Care. 2013;36:3655–62. https://doi.org/10.2337/dc13-0298.
Yamanouchi M, Furuichi K, Hoshino J, Toyama T, Hara A, Shimizu M, Research Group of Diabetic Nephropathy, the Ministry of Health, Labour and Welfare, the Japan Agency for Medical Research and Development, et al. Nonproteinuric versus proteinuric phenotypes in diabetic kidney disease: a propensity score-matched analysis of a nationwide, biopsy-based cohort study. Diabetes Care. 2019;42:891–902. https://doi.org/10.2337/dc13-0298.
Ito H, Antoku S, Izutsu T, Kusano E, Matsumoto S, Yamasaki T, et al. The prognosis of subjects showing a reduced estimated glomerular filtration rate without albuminuria in Japanese patients with type 2 diabetes: a cohort study for diabetic kidney disease. Clin Exp Nephrol. 2020;24:1033–43. https://doi.org/10.1007/s10157-020-01935-3.
Akizawa T, Gejyo F, Nishi S, Iino Y, Watanabe Y, Suzuki M, et al. Positive outcomes of high hemoglobin target in patients with chronic kidney disease not on dialysis: a randomized controlled study. Ther Apher Dial. 2011;15:431–40. https://doi.org/10.1111/j.1744-9987.2011.00931.x.
Hayashi T, Suzuki A, Shoji T, Togawa M, Okada N, Tsubakihara Y, et al. Cardiovascular effect of normalizing the hematocrit level during erythropoietin therapy in predialysis patients with chronic renal failure. Am J Kidney Dis. 2000;35:250–6. https://doi.org/10.1016/s0272-6386(00)70334-9.
Kuriyama S, Tomonari H, Yoshida H, Hashimoto T, Kawaguchi Y, Sakai O. Reversal of anemia by erythropoietin therapy retards the progression of chronic renal failure, especially in nondiabetic patients. Nephron. 1997;77:176–85. https://doi.org/10.1159/000190270.
Gouva C, Nikolopoulos P, Ioannidis JP, Siamopoulos KC. Treating anemia early in renal failure patients slows the decline of renal function: a randomized controlled trial. Kidney Int. 2004;66:753–60. https://doi.org/10.1111/j.1523-1755.2004.00797.x.
Tsubakihara Y, Gejyo F, Nishi S, Iino Y, Watanabe Y, Suzuki M, et al. High target hemoglobin with erythropoiesis-stimulating agents has advantages in the renal function of non-dialysis chronic kidney disease patients. Ther Apher Dial. 2012;16:529–40. https://doi.org/10.1111/j.1744-9987.2012.01082.x.
Singh AK, Carroll K, McMurray JJV, Solomon S, Jha V, Johansen KL, et al. Daprodustat for the treatment of anemia in patients not undergoing dialysis. N Engl J Med. 2021;385:2313–24. https://doi.org/10.1056/NEJMoa2113380.
Sofue T, Nakagawa N, Kanda E, Nagasu H, Matsushita K, Nangaku M, et al. Prevalence of anemia in patients with chronic kidney disease in Japan: a nationwide, cross-sectional cohort study using data from the Japan Chronic Kidney Disease Database (J-CKD-DB). PLoS One. 2020;15:e0236132. https://doi.org/10.1371/journal.pone.0236132.
Ito H, Matsumoto S, Izutsu T, Kusano E, Nishio S, Antoku S, et al. Comparison of the changes in the factors associated with the renal prognosis of non-elderly and elderly subjects treated with empagliflozin- a retrospective observation study in Japanese patients with type 2 diabetes. Diabetes Metab Syndr Obes. 2019;12:1783–94. https://doi.org/10.2147/DMSO.S221655.
UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352:854–65. https://doi.org/10.1016/S0140-6736(98)07037-8.
Collins BS, Hilliard ME, Isaacs D, Johnson EL, Kahan S, Khunti K, Leon J, Lyons SK, Perry ML, Prahalad P, et al. 9. Pharmacologic approaches to glycemic treatment: standards of care in diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S140-57. https://doi.org/10.2337/dc23-S009.
Ito H, Ishida H, Takeuchi Y, Antoku S, Abe M, Mifune M, et al. Long-term effect of metformin on blood glucose control in non-obese patients with type 2 diabetes mellitus. Nutr Metab (Lond). 2010;7:83. https://doi.org/10.1186/1743-7075-7-83.
Kohro T, Yamazaki T, Sato H, Harada K, Ohe K, Komuro I, et al. Trends in antidiabetic prescription patterns in Japan from 2005 to 2011. Int Heart J. 2013;54:93–7. https://doi.org/10.1536/ihj.54.93.
Ito H, Shinozaki M, Nishio S, Abe M. SGLT2 inhibitors in the pipeline for the treatment of diabetes mellitus in Japan. Expert Opin Pharmacother. 2016;17:2073–84. https://doi.org/10.1080/14656566.2016.1232395.
Acknowledgements
The authors thank Tomoko Koyanagi in the secretarial section of Edogawa Hospital for her valuable help with data collection.
Funding
The authors received no financial support for this study.
Author information
Authors and Affiliations
Contributions
HI contributed to the conception, design, analysis, interpretation, writing first draft, editing, and final approval. SM contributed to reviewing drafts, editing, and final approval. HI, TI, EK, SA, TY, TM, and MT contributed to data collection and final approval. All of the authors are in agreement with the content of the manuscript and have approved this submission.
Corresponding author
Ethics declarations
Conflict of interest
H Ito has received lecture fees from Eli Lilly Japan KK, Novo Nordisk Pharma Ltd., Sumitomo Pharma Co., Ltd. and Boehringer Ingelheim. S Matsumoto, H Inoue, T Izutsu, E Kusano, S Antoku, T Yamasaki, T Mori, and M Togane have no conflicts of interest.
Ethical approval
The study was conducted in accordance with the principles expressed in the 2008 Declaration of Helsinki. The Ethics Committee of Edogawa Hospital approved the study protocol (approved numbers: 2015-18 and 2022-1, approved date: July 6, 2015 and November 24, 2021, respectively) and waived the need for written informed consent because the data were analyzed anonymously for this analysis based on information stored in the hospital. The trial is retrospectively registered on UMIN-CTR, identifier UMIN000047632 (1 May, 2022).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
13340_2023_637_MOESM1_ESM.pptx
Supplementary file1 (PPTX 115 KB) Supplementary Fig. 1. Kaplan-Meier analyses of the components of cardiovascular events in the groups with and without anemia. (A) Cardiovascular death, (B) nonfatal myocardial infarction, (C) heart failure, and (D) nonfatal stroke. Supplementary Fig. S2. Kaplan-Meier analyses of the components of renal events in the groups with and without anemia. (A) End-stage kidney disease, (B) decline in eGFR by ≥30%. Supplementary Fig. S3. Kaplan-Meier analyses of the components of cardiovascular events in the groups with anemia with a hemoglobin level of <110 g/L, with anemia with a hemoglobin level of ≥110 g/L, and without anemia. Supplementary Fig. S4. Kaplan-Meier analyses of the components of renal events in the groups with anemia with a hemoglobin level of <110 g/L and anemia with a hemoglobin level of ≥110 g/L and without anemia. Supplementary Fig. S5. Kaplan-Meier analyses of cardiovascular events in the groups classified by anemia and uACR with (A) and without (B) a reduced eGFR. Supplementary Fig. S5. Kaplan-Meier analyses of renal events in the groups classified by anemia and uACR with (A) and without (B) a reduced eGFR
About this article
Cite this article
Ito, H., Matsumoto, S., Inoue, H. et al. Anemia combined with albuminuria increases the risk of cardiovascular and renal events, regardless of a reduced glomerular filtration rate, in patients with type 2 diabetes: a prospective observational study. Diabetol Int 14, 344–355 (2023). https://doi.org/10.1007/s13340-023-00637-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-023-00637-x