Abstract
Background and Objective
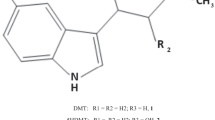
N,N-dimethyltryptamine (DMT) is a psychedelic compound under development for the treatment of major depressive disorder (MDD). This study evaluated the preclinical and clinical pharmacokinetics and metabolism of DMT in healthy subjects.
Methods
The physiochemical properties of DMT were determined using a series of in vitro experiments and its metabolic profile was assessed using monoamine oxidase (MAO) and cytochrome P450 (CYP) inhibitors in hepatocyte and mitochondrial fractions. Clinical pharmacokinetics results are from the phase I component of a phase I/IIa randomised, double-blind, placebo-controlled, parallel-group, dose-escalation trial (NCT04673383). Healthy adults received single escalating doses of DMT fumarate (SPL026) via a two-phase intravenous (IV) infusion. Dosing regimens were calculated based on pharmacokinetic modelling and predictions with progression to each subsequent dose level contingent upon safety and tolerability.
Results
In vitro clearance of DMT was reduced through the inhibition of MAO-A, CYP2D6 and to a lesser extent CYP2C19. Determination of lipophilicity and plasma protein binding was low, indicating that a high proportion of DMT is available for distribution and metabolism, consistent with the very rapid clinical pharmacokinetics. Twenty-four healthy subjects received escalating doses of DMT administered as a 10-min infusion over the dose range of 9–21.5 mg (DMT freebase). DMT was rapidly cleared for all doses: mean elimination half-life was 9–12 min. All doses were safe and well tolerated and there was no relationship between peak DMT plasma concentrations and body mass index (BMI) or weight.
Conclusion
This is the first study to determine, in detail, the full pharmacokinetics profile of DMT following a slow IV infusion in humans, confirming rapid attainment of peak plasma concentrations followed by rapid clearance. These findings provide evidence which supports the development of novel DMT infusion regimens for the treatment of MDD.
Clinical Trial Registration
Registered on ClinicalTrials.gov (NCT04673383).
Similar content being viewed by others
Peak plasma levels of N,N-dimethyltryptamine (DMT) are rapidly attained and cleared following intravenous doses of 9–21.5 mg DMT administered as a 10-min infusion. DMT is rapidly metabolised by monoamine oxidase (MAO) A. Additionally, these are the first published findings to our knowledge that identify specific human cytochrome P450 (CYP) isozymes (2D6 and 2C19) can contribute to the metabolism of DMT in active MAO-A sparce environments. Body weight and body mass index were not shown to correlate with the peak DMT exposure and pharmacokinetic variability. These findings contribute to the development of improved pharmacokinetic and metabolic models of DMT and to the design of IV infusion regimens for the treatment of mental health disorders. |
1 Introduction
A number of clinical trials have supported the use of psychedelics for the treatment of major depressive disorder (MDD) [1,2,3,4,5,6]. Dose-dependent increases in therapeutic efficacy have been observed, attributed to the complex receptor pharmacology and the quality of subjective effects elicited by psychedelic drugs [7]. N,N-dimethyltryptamine (DMT) is the principal psychedelic compound contained in the psychoactive plant brew ayahuasca [8]. A number of studies have evaluated the pharmacokinetics (PK) of DMT in humans, although these have largely been limited to investigations following oral ingestion of ayahuasca [9,10,11,12,13]. However, ayahuasca contains harmala alkaloid constituents which function as monoamine oxidase (MAO) inhibitors to DMT metabolism, rendering it orally bioavailable. In contrast, DMT is not orally bioavailable when administered independently [14]. Injected formulations of DMT are extremely short acting because of its rapid metabolism leading to the formation of its primary metabolite, indole-3-acetic acid (IAA), via oxidative deamination [15,16,17].
A study following bolus intravenous (IV) administration of DMT in healthy volunteers showed that peak blood concentrations were reached at approximately 2 min; however, no other PK variables were reported [16]. Similarly, psychedelic effects are apparent almost immediately and resolve within approximately 30 min. Plasma levels of DMT correlate with changes in brain activity and intensity of psychedelic experience [17, 18] and therefore provide a proxy measure to underlying neuropharmacology. Moreover, it has been suggested that a more complete psychedelic experience can be achieved through modified IV infusion regimens which maintain therapeutic concentrations of DMT over a longer time period [19].
The purpose of the studies presented here was to investigate the PK and metabolism of DMT in humans. We report results evaluating, for the first time to our knowledge, the PK profile of escalating doses of DMT administered as a slow (10 min) IV infusion in psychedelic-naïve healthy subjects, which was conducted in the phase I component of a phase I/IIa clinical trial, hereinafter referred to as phase I. The objective of the phase I study was to determine a safe and well-tolerated infusion dose of DMT that elicits a ‘breakthrough’ psychedelic experience (defined as an immersive and intense experience in which almost all connection to the real world is lost) to give to patients with MDD in the phase IIa component of the clinical trial.
2 Methods
2.1 In Vitro Studies
Methods for the in vitro studies were performed by Sygnature Discovery Ltd. (Nottingham, UK). The in vitro data described were performed as part of a larger investigation of deuterated DMT (SPL028) where DMT was used as a reference control. Only data relating to DMT are presented here to compliment interpretation of clinical PK. Analytical assays were validated by the inclusion of positive control compounds and results were compared to historical control data (full validation data is presented in the supplementary material). All analyses were performed using ultra-high-performance liquid chromatography-tandem mass spectrometry (LC-MS/MS). Materials and reagents used in the in vitro studies were supplied by Sigma-Aldrich (controls and inhibitors), Tebu-bio (mitochondrial fraction), Pharmaron (Male mouse CD-1 blood) and platelet services (Human blood).
2.1.1 Human Hepatocytes
Human hepatocytes from ten donors (male and female) were thawed in a water bath at 37 °C and decanted into hepatocyte buffer solution (26.2 mM NaHCO3, 9 mM HEPES, 2.2 mM D-fructose, Dulbecco’s Modified Eagle Medium, in MilliQ purified water), which was centrifuged, the supernatant removed and resuspended in hepatocyte buffer solution at the final assay concentration (nominal 0.5 million cells/ml). DMT fumarate and compound positive control stocks [sumatriptan (MAO-A), benzylamine (MAO-B), serotonin (MAO-A), diltiazem (CYP3A4 metabolism) and diclofenac (CYP2C9, CYP3A4 and glucuronidation metabolism)] were prepared at 10 mM in DMSO and diluted to 100 × the assay concentration in 9:1 acetonitrile:DMSO.
To investigate the impact of MAO-A and MAO-B inhibition, the stability of a final concentration of DMT fumarate at 5 µM was tested with and without (100 nM clorgyline and 100 nM deprenyl/selegiline), which was added as a cassette 15 min prior to the addition of a final compound stock. A concentration of 1 µM diltiazem and diclofenac markers was selected as in accordance with validated study site standard procedures whereas a concentration of 5 µM for DMT fumarate and MAO substrate markers was initially chosen to increase the signal-to-noise ratio relative to analytical sensitivity. A separate study was also conducted investigating the stability of a final concentration of DMT fumarate at 1 µM in the absence of inhibitors.
Hepatocytes were added to pre-warmed incubation tubes (37 °C) together with compound stock solution 0.9% (v/v) acetonitrile and 0.1% (v/v) DMSO to achieve a final count of 0.362 million viable cells/ml, shaken orbitally though the experiment. Aliquots were taken from the incubation tubes at 4, 8, 15, 30, 45 and 60 min and quenched 1:4 with ice-cold acidified methanol or acetonitrile-containing internal standard before protein precipitation at – 12 °C for a minimum of 12 h before centrifugation at 4 °C. Supernatants were transferred to 96-well plates for ultra-high-performance liquid chromatography-tandem mass spectrometry (LC-MS/MS) analysis.
2.1.2 Human Mitochondrial Fraction
Human liver mitochondrial fractions (XenoTech, Sekisui, mixed gender, 5-donor pool) were assayed, in the presence or absence of selective inhibitors of monoamine oxidase (MAO)-A (clorgyline, 100 nM final concentration) and MAO-B (deprenyl/selegiline, 100 nM final concentration). Similar methodology to the human hepatocyte experiments, with a final liver mitochondrial concentration of 0.5 mg/ml, was used.
For the irreversible inhibition of MAO-A and MAO-B, the inhibitors (100 nM final concentration) were added 15 min prior to the addition of DMT fumarate at 5 µM final concentration. Positive control substrates for MAO-A (serotonin) and MAO-B (benzylamine) were included and screened at 5 µM final substrate concentration. A separate study investigated the metabolic stability of DMT fumarate at 1 µM final concentration without the inclusion of MAO-A or MAO-B inhibitors.
The time points used in the assay were 2, 4, 8, 15, 30, 45 and 60 min and intrinsic clearance (CLint) and t1/2 were calculated in the same way as the human hepatocyte experiment.
2.1.3 Cytochrome P450 (CYP) Phenotyping
Cytochrome P450 (CYP) phenotyping was assessed using DMT fumarate and marker compounds for eight human CYP isozymes (bactozomes) prepared at 10 mM in DMSO and further diluted to 100 × the assay concentration. Marker compounds included carvedilol (CYP1A2, CYP2C9, CYP2C19, CYP2D6, CYP3A4), verapamil (CYP2C8, CYP3A5), bupropion and ticlopidine (CYP2B6), montelukast (CYP2C8), diclofenac (CYP2C9), propranolol (CYP2C19), dextromethorphan (CYP2D6) and midazolam (CYP3A4).
Individual CYP bactosomes (CYPEX Ltd., UK) were thawed at room temperature and diluted to 200 pmol/ml in 0.1 M phosphate buffer. DMT fumarate and marker compounds were added to incubation tubes together with CYP bactosomes and pre-warmed for 5 min at 37 °C before the addition of pre-warmed NADPH (10 mM in 0.1 M phosphate buffer) to achieve final concentrations of 1 μM DMT fumarate/marker compounds and 100 pmol/ml CYP bactosomes in phosphate buffer and 1% (v/v) DMSO.
At each predetermined time point (2, 5, 15, 30, 45 and 60 min) samples were taken and quenched 1:4 with ice-cold methanol- or acetonitrile-containing internal standard. Quenched samples were mixed before protein precipitation at – 12 °C for a minimum of 12 h before centrifugation at 4 °C. Supernatants were transferred to 96-well plates for LC-MS/MS analysis. MS peak areas were used to generate ln (MS response) vs. time plots, from which intrinsic clearance (μM/min/nmol CYP) and half-life (t1/2, min) values were calculated using Eqs. 1, 3 and 5.
Projected CYP isozyme intrinsic clearance (Eq. 2) accounting for estimated CYP abundance in human liver microsomes (μM/min/mg microsomal protein) is calculated using Eq. (5) and estimated CYP abundance values (Table 1).
2.1.4 Blood:Plasma Ratio
Blood:plasma ratio was determined using fresh human blood and plasma samples from a donor panel aliquoted and pre-incubated at 37 °C for 5 min. DMT fumarate (1μM), diclofenac (positive control, 1 μM) and verapamil (positive control, 1 μM) were prepared at 2 mM in DMSO, while chloroquine (positive control, 1 μM) was prepared at 2 mM in water, before all were further diluted to 100 × the final assay concentration in methanol.
Stocks of DMT and controls were separately spiked 1:100 into the blood and plasma samples, which were incubated at 37 °C for 30 min, with shaking for 15 s at 15 and 30 min. After 30 min plasma samples were quenched 1:3 into ice-cold methanol-containing internal standard; blood samples were centrifuged, and an aliquot of the plasma was taken and supernatant quenched 1:3 into ice-cold methanol-containing internal standard before protein precipitation between the matrix-matched plasma samples at – 12 °C for a minimum of 12 h before centrifugation at 4 °C. Supernatants were transferred to 96-well plates for LC-MS/MS analysis.
MS peak areas were used to generate ln (MS response) vs. time plots. Subsequent intrinsic clearance (µl/min/million cells) and half-life (t1/2, min) values were calculated using the following Eqs. 3–5:
2.1.5 Plasma Protein Binding
Plasma protein binding was assayed using thawed pooled donor plasma, which was centrifuged, and the resulting supernatant decanted into a fresh vessel, with pH adjusted to 7.4 using lactic acid or NaOH. DMT fumarate and marker stocks were prepared at 10 mM in DMSO and further diluted to 100 × the assay concentration, which was then spiked 1:100 into the plasma samples to achieve a final concentration of 5 μM, except for DMT fumarate, which was prepared at 1.64 μM because of a technical error.
For each sample, 200 µl of the spiked plasma was added to the red compartment of a Rapid Equilibrium Dialysis (RED) plate (Thermo Fisher Scientific, UK) with 350 µl PBS added to the buffer compartment before sealing the RED plate with a breathable lid and shaking on an orbital shaker in a 37 °C incubator at 5% CO2 for 4 h. A sample of the plasma/DMT was taken and mixed with an equal volume of PBS, and a sample was taken from the buffer side and mixed with an equal volume of blank plasma before quenching 1:3 with ice-cold acetonitrile-containing internal standard. The matrix-matched quenched samples were mixed before protein precipitation at – 12 °C for a minimum of 12 h before centrifugation at 4 °C.
Supernatants were transferred to 96-well plates for LC-MS/MS analysis; values were derived for fraction of unbound and bound drug, together with recovery, following the preparation of matrix-matched standard curve and quality control samples to allow for quantification of the concentration in each sample.
2.1.6 Lipophilicity
The distribution coefficient logD7.4 measures the partition of substances in octanol and aqueous solutions in a solution at pH 7.4, i.e., approximating that of blood. A 10 mM stock of DMT fumarate diluted in DMSO was prepared together with 10 mM control markers (ketoconazole, propranolol and verapamil). These were added to incubation tubes together with octanol before shaking for 5 min; buffer was added and the tubes shaken for a further 90 min at room temperature. The tubes were then centrifuged at room temperature and samples taken from both octanol and buffer fractions, which were diluted to give similar responses on LC-MS/MS before being transferred to 96-well plates with methanol-containing internal standard prior to LC-MS/MS analysis.
2.1.7 Liquid Chromatography-Tandem Mass Spectrometry
Samples were analysed by LC-MS/MS using Thermo TSQ Quantiva with Thermo Vanquish UPLC system (Thermo Fisher Scientific, Hemel Hempstead, UK) with a calibration range of 2.5–1000 nM for DMT. Separation of analytes was performed using Luna Omega 2.1 × 50 mm, 2.6 µm column at 65 °C with a 1 µl/sample. The mobile phase consisted of solvent A [0.1% (v/v) formic acid in water] and solvent B [0.1% (v/v) formic acid in acetonitrile] using a gradient of 5–99% of B (0–1.35 min), 5% (1.36–11.8) and flow rate of 0.8 ml/min. MS was performed with an electrospray ionisation (ESI) source in the positive-ionization mode with multiple reaction monitoring and a sheath gas of 54 Arb and aux gas of 17 Arb. The ion spray voltage was set at 4000 V and the source temperature was 450 °C. The mass-to-charge transition (m/z) of precursor and product ions for DMT was identified as: (m/z) 189.13 → 58.15, 144.04.
2.2 Phase I Clinical Study
2.2.1 Subjects
To be eligible to participate in the phase I clinical study male and female subjects were required to be aged ≥ 25 years, with no previous exposure to serotonergic psychedelic substances, and registered with a general practitioner within the UK. Subjects were also required to have a body mass index (BMI) 18.0–30.9 kg/m2, no clinically relevant physical findings and no abnormal electrocardiogram (ECG) or clinical laboratory parameters at the screening visit.
Subjects with a current or past diagnosis of a mental health disorder as defined by the American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5), a history of suicide attempts or any first- or second-degree relative with a psychotic or bipolar disorder were excluded from the study. The minimum age restriction was set to minimise the risk of recruiting subjects with a predisposition to or undiagnosed non-affective psychosis disorder.
2.2.2 Study Design and Treatment
The phase I study was a single-centre, randomised, double-blind, placebo-controlled, parallel-group dose-escalation trial (ClinicalTrials.gov: NCT04673383; EudraCT: 2020-000251-13). The study was conducted to meet criteria of European Medicines Agency (EMA) guidelines and Good Clinical Practice (GCP). It was approved by the UK Medicines and Healthcare Products Regulatory Agency (MHRA) and London Brent ethics committee.
Due to the psychedelic effects of DMT and the absence of comprehensive safety and tolerability data from previous clinical studies, EMA guidelines for risk identification and risk mitigation were followed [20] together with scientific advice from the MHRA. Additionally, the study was designed in accordance with published guidelines regarding the clinical assessment of hallucinogenic substances in humans [21].
The phase I study was exploratory and there were no null hypotheses; therefore, study data were not subject to formal statistical analyses or sample size calculations. The sequential single ascending dose escalation group design (described below) was based on the Association of the British Pharmaceutical Industry (ABPI) phase I clinical trial guideline example [22].
At the screening visit, subjects provided written informed consent and attended a structured interview with the study psychiatrist using the Mini-International Neuropsychiatric Interview. All subjects participated in individual or group preparation sessions, including advice on what to expect and how to respond to the psychedelic experience at screening and again the day prior to study drug administration.
Subjects were admitted to the clinical pharmacology unit [Hammersmith Medicines Research (HMR), London, UK] the day before study drug administration. No intake of alcohol or caffeine for 24 h before and during the treatment period was permitted. On the day of treatment, study drug was administered in a room set up according to best practice principles for psychedelic studies [21], including soft lighting, soft furnishings, music and photographs/art depicting scenes of nature; subjects were also asked to wear an eye mask during study drug administration. A therapist and a psychiatrist were present in the room, with additional clinical staff supervising study drug administration and blood sampling.
Subjects were carefully monitored for adverse events (AEs) using non-leading questions such as “How are you feeling?” and spontaneously according to subject responses. Drug-related AEs were categorised by severity as either mild, moderate or severe using the following definitions: mild, an AE causing mild discomfort which did not interfere with the subject’s daily routine and did not require intervention; moderate, an AE causing moderate discomfort which interferes with some aspects of the volunteer’s routine or requires intervention, but is not damaging to health; severe, an AE clearly damaging to health which results in alteration, discomfort or disability. Any clinically significant changes in physical findings, ECG or laboratory parameters were also recorded as AEs.
Subjects were required to remain in the clinical unit overnight for further psychological and safety evaluations and discharged the next morning dependent on satisfactory assessment outcomes. Follow-up was conducted by phone or video call for up to 3 months after study treatment.
Four single ascending dose levels of DMT were studied (Table 2); escalation to the next dose was dependent on the safety, tolerability and the PK profile of each prior dose level. Further details of the clinical study and psychotherapy methodology will be published elsewhere (in preparation).
A fumarate salt of DMT (SPL026) drug substance and drug product was manufactured in a 1:1 ratio in the UK in accordance with Good Manufacturing Practice (GMP) with 2.5 mg/ml DMT free base in 10 ml aqueous sterile solution; placebo consisted of the same ingredients and volume with the exception of the active substance. Active and placebo treatments were identical in appearance and administered in the same volume. The synthesis of SPL026 will be reported elsewhere (publication submitted).
2.2.3 Dosing Procedure
Study drug was administered as a continuous 10-min IV infusion, split into two phases. Due to the rapid metabolism of DMT, it was reasoned that an initial slow injection to gradually increase plasma concentrations would provide a gentler onset of subjective psychedelic experience for subjects to begin the DMT infusion. The second infusion phase was designed to achieve similar peak plasma concentrations and therefore peak subjective psychedelic effects attained in previous clinical studies [16, 17].
A single cannula was inserted in the forearm vein with two separate syringes and two separate syringe pumps connected by a three-way tap to provide different infusions rates for the two phases of infusion. The first syringe pump infused study drug over 5 min (phase 1) followed by another 5-min infusion from the second syringe pump (phase 2).
Four dosing regimens of DMT were used (Table 2) and each dose cohort was randomised so that six subjects received DMT and two received placebo. First, two subjects (sentinel subjects) at each dose level received study treatment (1 randomised to DMT and 1 to placebo) and were dosed prior to the remaining subjects within that cohort. Provided the tolerability and safety in the sentinel subjects were acceptable, the remaining subjects at that dose level received study treatment (5 randomised to DMT and 1 to placebo).
Following the completion of each dose level, the PK data were reviewed alongside all safety and tolerability data before progression to the next dose cohort group. All sentinel subjects were included in the safety analyses but only the sentinel subjects receiving DMT were included in the pharmacokinetic analyses.
2.2.4 Dose Rationale
The dosing regimen used in this study was selected based on PK modelling of existing clinical data. Prior to study start, compartmental analysis was performed using plasma concentration-time data from 12 healthy adults over 3 different IV (30 s) bolus doses of DMT fumarate collected in a previous clinical study [17, 23] (3 subjects at 7 mg, 4 subjects at 14 mg and 5 subjects at 20 mg). These data were used generate a single PK model for each dose level. Various weighting schemes were evaluated based on visual fit, parameter errors and runs of residuals. A final one-compartment IV model by an iteratively reweighted non-linear least squares (IRWLS) algorithm and 1/concentration weighting scheme was used to fit the data with the following equation (Eq. 6):
where t* represents t (actual time) post start of infusion. V1 and λ1 represent the volume and elimination rate, respectively.
A series of two-compartment models were also considered; however, parameter errors and overall visual appearance of the fitted lines were determined unsuitable.
2.2.5 Dose Simulation
Estimated V1 and Ke model parameters (Table 3) derived from 14 mg dose level (known to produce marked psychedelic effects [17, 23]) were used to simulate a series of two-phase IV infusion doses. The first infusion phase (phase 1) was designed to slowly bring subjects to the fringe or early stages of a psychedelic experience and was the same across all dose cohorts. An infusion dose of 6 mg over 5 min was modelled to support the intent of a gradual onset of psychedelic experience and peak exposure level equivalent to a previously administered 7 mg DMT fumarate (30 s IV bolus) dose which was considered to produce mild psychedelic effects [17, 23]. The second infusion phase (phase 2) was intended to either maintain or further intensity the psychedelic effects attained in phase 1 and was increased with each dose escalation.
A starting dose (cohort 1) was modelled to attain (phase 1: 6 mg over 5 min) and maintain (phase 2: 3 mg over 5 min) the exposure level and mild psychedelic effects reached in the first phase of infusion, while the intention of the final dose level was to reach peak concentration levels equivalent to those previously reported following a 17 mg DMT fumarate (30 s IV bolus) dose [17, 23]. This exposure was considered to produce a sufficiently intense ‘breakthrough’ psychedelic experience (defined above) which is safe and well tolerated. Following the completion of each dose cohort, the pharmacokinetic profile and tolerability data were reviewed with the objective of attaining a complete psychedelic experience with minimal somatic effects in subjects. Each dose escalation step was carefully modelled to achieve incremental increases in exposure from the previous cohort to ensure that the safety and tolerability of each infusion regimen could be investigated in a dose-dependent manner. A total of four dose cohorts were evaluated; the final infusion regimens of DMT are given in Table 2.
Compartmental and simulated pharmacokinetic analyses were conducted using PCModfit version 6.9 for Windows running with Microsoft Excel [24].
2.2.6 Pharmacokinetics
Blood samples were drawn using a cannula inserted in the forearm vein (the opposite side to where study treatment was administered) pre-dose and at a nominal 2, 5, 6, 7, 10 (end of IV infusion), 11, 13, 15, 30, 60, 120 and 240 min after the start of the infusion. Blood samples (3 ml) were taken into 3-ml K2EDTA tubes and immediately placed on ice. Samples were centrifuged at 1500 × g for 10 min at 4 °C, divided into two aliquots of approximately equal volume (minimum of 0.5 ml in the primary aliquot) in screw-capped polypropylene cryotubes and frozen at ≤ − 80 °C within 2 h after collection, and stored until bioanalysis.
Plasma concentrations at actual time points for each subject were analysed. The following pharmacokinetic parameters were calculated using noncompartmental analysis of all available data for each evaluable subject after IV administration: maximum (peak) plasma concentration (Cmax); concentration at 5 min (C5min), time to peak plasma concentration (Tmax), area under the plasma concentration-time curve from time zero to time of last measurable concentration (AUClast); area under the plasma concentration-time curve from time zero to infinity (AUCinf); terminal half-life (t1/2); clearance (CL); apparent volume of distribution during terminal phase (Vz); volume of distribution at steady state (Vss); mean residence time (MRTinf).
Determination of DMT and IAA in human plasma was conducted using ultra-high-performance LC-MS/MS system (Pharmaron UK Ltd., Rushden). The bioanalytical method for the determination of DMT in human plasma (K2EDTA) using LC-MS/MS was fully validated over the calibration range 0.0619 ng/ml to 310 ng/ml in accordance with GCP and following full validation procedures based on bioanalytical guidelines [25, 26]. The calibration range for IAA was 2.00–1000 ng/ml. Ultra-high-performance liquid chromatography (UHPLC) was performed using ExionLC system with autosampler set at 4 °C. An analytical column (Acquity BEH C18 2.1 × 50 mm, 1.7 µm) maintained at 60 °C was used to separate analytes with a gradient elution programme using mobile phase A [0.1% (v/v) formic acid in water] and mobile phase B (acetonitrile) as follows: 0.00 min (90% A, 10% B); 2.00–2.50 min (5% A, 95 % B); 2.51–3.00 min (90% A, 10% B). The flow rate was 350 μl/min. MS analysis was performed using Applied Biosystems API6500+, with an ESI source in the positive-ionization mode with multiple reaction monitoring. Source conditions were optimized with the curtain gas at 40 psi, IonSpray Voltage at 5500 V and temperature 400 °C. The mass-to-charge transition (m/z) of precursor and product ions for DMT was identified as: (m/z) 189.5 → 58.2 and for IAA was identified as: (m/z) 176.2 → 130.3. The precision and accuracy of the bioanalytical method were within acceptance criteria [± 15% (± 20% for lower limit of quantification, LLOQ)] as determined by measurement of DMT in replicate (n = 6) quality control (QC) samples at four different concentration levels (LLOQ, low, medium and high) on a minimum of three occasions. The internal standard used for DMT was α,α,bis-deuterio-N,N-hexadeuterio-dimethyltryptamine (DMT-d8) and control blank was human plasma (K2EDTA; BiolVT Ltd.).
2.2.7 Statistical Analyses
The pharmacokinetic concentration population comprised subjects who received at least one dose of study treatment and for whom a blood sample had been analysed. The pharmacokinetic parameter population comprised subjects in the pharmacokinetic concentration population for whom pharmacokinetic parameters could be derived.
Actual sampling times were used to derive pharmacokinetic parameters and missing data were not imputed. Plasma concentrations of DMT below the LLOQ of the LC-MS/MS were either treated as zero (if they occurred before Tmax) or considered missing.
Plasma concentrations and pharmacokinetic parameters were summarised by treatment, using descriptive statistics. For log-transformed parameters, the primary measure of central tendency was the geometric mean, and for other parameters, it was the arithmetic mean or median.
Dose proportional relationship between Cmax and AUClast dose were assessed using the power model [27] (log pharmacokinetic parameter = α + β × log(dose) + ε), where α = intercept and β = slope. The power model was fitted by restricted maximum likelihood (REML) mixed effect model, with intercept and log(dose) as fixed effects. The dose proportionality of each PK parameter was confirmed if the 90% confidence interval (CI) of β (log pharmacokinetic parameter vs. log dose) included the value 1.0.
The relationship between BMI and body weight vs. dose-normalised Cmax and concentration at 5 min (C5min) was determined by separate hierarchical regression analyses; age and sex were included as control variables. These analyses were conducted post hoc to investigate the relationship of BMI and body weight regarding pharmacokinetic variability and to confirm that fixed dosing (rather than weight-based dosing) of DMT was appropriate.
Pharmacokinetic analysis was conducted by the Statistics and Data Management Department at HMR, using WinNonlin version 8.1 or higher. Descriptive statistics were derived using SAS version 9.4 or higher, including mean, standard deviation (SD), median, minimum and maximum values. Additionally, for pharmacokinetic variables percent coefficient of variation (%CV) and 95% CI of the arithmetic mean were derived. The adjusted coefficient of determination (R2) measured the goodness of fit for the linear regression model (where values range from 0–1, 0 indicating that the predictor variable accounts for no variation in the dependent variable and 1 predictor variable accounts for all variation in dependent variable values). Post-hoc analyses were performed using IBM SPSS version 28.0 and tested at the p < 0.05 significance level.
3 Results
3.1 In vitro experiments
The intrinsic hepatocyte clearance of DMT [0.62 (1) µM] was 19.4 ± 0.8 µl/min/million cells with a half-life of 98.9 ± 3.9 min (mean ± SD). Separately, MAO inhibition had a minimal impact on the intrinsic hepatocyte clearance rate of DMT [3.1 (5) µM], 13.8 µl/min/million cells (half-life, 92.4 min) with MAO inhibitors vs. 13.24 µl/min/million cells (half-life, 96.1 min) in the absence of MAO inhibition (Table 4).
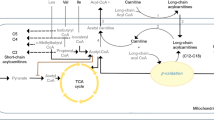
The contribution of MAO in the metabolism of DMT was further assessed in human liver mitochondrial fractions. The intrinsic clearance of DMT (0.62 µM, n = 2) was 175.0 µl/min/mg protein (half-life, 7.9 min). At a higher concentration, the intrinsic clearance of DMT (3.1 µM) was reduced by > 90% (approximately 11-fold) by the MAO-A inhibitor compared to vehicle control (< 3.9 vs. 42.9 µl/min/mg protein), with an accompanying increase in half-life (> 373.7 vs. 33.7 min); however, there was no influence of MAO-B inhibition (intrinsic clearance, 42.7 µl/min/mg protein; half-life, 32.5 min) (Table 4).
Serotonin (MAO-A) and benzylamine (MAO-B) substrate controls demonstrated the effective blocking of MAO activity with the inclusion of inhibitors in hepatocyte and mitochondrial fractions (Table 4).
CYP phenotyping using eight human enzymes showed DMT intrinsic clearance was 801 µl/min/nmol CYP (half-life, 9 min) for CYP2D6 and 37 µl/min/nmol CYP (half-life, 189 min) for CYP2C19. These data correspond to an estimated clearance rate of 9.5 and 0.3 µl/min/mg microsomal protein with CYP2D6 and CYP2C19, respectively, indicating a role for CYP2D6 and minor role of CYP2C19 in DMT metabolism in human liver. No turnover of DMT was detected with CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP3A4 and CYP3A5 (< 29 µl/min/nmol CYP) for the duration of the study indicating that DMT is not a substrate for these isozymes.
Mean logD7.4 (n = 2) was 0.15 demonstrating a low lipophilicity indicative of poor permeability and low non-specific binding of DMT which was supported by the plasma protein binding result of 67.7% unbound DMT (Table 5). The blood:plasma ratio was 1.53 for DMT (Table 6) demonstrating partitioning into blood cells.
3.2 Clinical Study
3.2.1 Clinical Findings
Baseline demographics were similar across dosing cohorts with a mean age of 36.4 (range 25–76) years and mean BMI of 25.0 kg/m2; eight subjects were female (25%) (Table 7). All four doses of DMT were found to be safe and well tolerated in all subjects. All 32 enrolled subjects completed study treatment and a total of 13 subjects had drug-related treatment-emergent AEs (drTEAEs), which were categorised as either mild or moderate; all were transient in nature (Table 8) and no serious AEs were recorded.
3.2.2 Pharmacokinetic Analysis
As mean measured concentrations of DMT at the 120 min and 240 min time points were low (< 0.1 ng/ml) (Table 9), these time points were excluded from Fig. 1 to improve graphical data representation. Due to dosing errors, one subject from cohort 1 and one subject from cohort 3 were excluded from pharmacokinetic analyses. The pharmacokinetic parameters from each dosing group are presented in Table 10.
Pharmacokinetic analysis of five evaluable subjects from cohort 1 that received a total dose of 9 mg DMT (Table 10) had a large observed inter-individual variability for both Cmax (mean 20.8 ng/ml; range 5.0–34.9) and AUClast (mean 349 ng·min/ml; range 71–705) (Table 10, Fig. 1). Mean t1/2 was 12.1 min (range 5.8–18.3).
For the six subjects in cohort 2 that received 12 mg DMT (6 mg over 5 min and then 6 mg over 5 min), mean DMT Cmax = 30.6 ng/ml (range 12.7–62.3), mean AUClast = 451 ng·min/ml (range 245–755) (Table 10, Fig. 1) and mean t1/2 was 9.5 min (range 6.0–17.0).
Regarding the five subjects from cohort 3 that received a dose of 17 mg DMT (6 mg over 5 min then 11 mg over 5 min), sampling cannula issues for pharmacokinetic data resulted in nine missing data points. It was therefore not possible to calculate any parameters for DMT other than Cmax (mean 72.1 ng/ml; range 16.2–126.0) and AUClast (mean 842 ng·min/ml; range 204–1298) (Table 10).
The final cohort (cohort 4) received DMT infused as 6 mg over 5 min followed by 15.5 mg over 5 min (total dose 21.5 mg). For these six subjects mean Cmax was 62.7 ng/ml (range 29.0–107) (Table 10) and mean AUClast was 835 ng·min/ml (range 477–1052); mean t1/2 (12.1 min; range 6.3–20.3) was in line with the previous dose cohorts. Median Tmax for each cohort was approximately 10 min (close to the end of the infusion), before an observed gradual decline over the remaining sampling period (Fig. 1).
Individual C5min following a 6 mg dose ranged from 3.32 ng/ml to 43.0 ng/ml across all dose cohorts. A one-way ANOVA revealed that there were no significant differences between cohorts [F(3,20) = 1.628, p = 0.214].
IAA concentrations were measured from four subjects from cohort 2 and cohort 4 as an exploratory measure to provide a representative sample for determining IAA/DMT concentration ratio. Pre-dose plasma concentrations of IAA were measured in each of the eight evaluated subjects (mean, 316 ng/ml; range, 169–562 ng/ml); however, baseline corrected analysis was not conducted as the lowest IAA concentration measurements were recorded from various different time points from 0–7 min for seven subjects. Mean maximum plasma IAA concentrations were 1532.5 ng/ml (range 1350.0–1760.0 ng/ml; %CV 13.1, cohort 2) and 2182.5 ng/ml (range 1640.0–3250.0; %CV 34.2, cohort 4), which were recorded between 30–60 min post the beginning of infusion dosing of DMT. Of the subjects with IAA measurements, the variation (%CV) in maximum plasma exposure of DMT was 40.5% (cohort 2) and 24.0% (cohort 4). The Cmax of IAA relative to DMT was between 39.5–102.4 times greater for subjects in cohort 2 and 30–42 times greater for subjects in cohort 4. IAA concentrations did not resolve to baseline levels by 240 min.
3.2.3 Dose proportionality
The relationship of individual Cmax and AUClast vs. dose is illustrated in Fig. 2. In the analysis of dose proportionality of Cmax and AUClast using the power model, each slope (β) and corresponding 90% CI were 1.58 (0.84–2.33) and 1.35 (0.65–2.04), respectively. Owing to pharmacokinetic sampling difficulties described above, a sensitivity analysis which removed cohort 3 from analysis β (CI) for Cmax was 1.47 (0.74–2.20) and AUClast 1.29 (0.59–2.00). As the 90% CI of the slope for each analysis encompassed 1.0, these results are consistent with dose proportionality. However, as 90% CIs were wide, this conclusion should be interpreted with caution.
Post-hoc hierarchical regression analysis showed no relationship across all dose cohorts between BMI (β = 0.179, p = 0.508) or weight (β = 0.107, p = 0.671) with dose-normalised Cmax when controlling for sex, age and dose cohort. Similarly, there was no relationship between BMI (β = − 0.490, p = 0.078) or weight (β = − 0.215, p = 0.426) with C5min when controlling for sex and age. None of the four models were predictive of dose-normalised Cmax and C5min outcome variables with statistical significance (p > 0.05).
4 Discussion
DMT is a short-acting psychedelic tryptamine which is currently being developed, with supportive therapy, as a treatment for MDD. While data have previously been published on the metabolism and pharmacokinetics of DMT, data have been limited to a few pharmacokinetic parameters [15, 17, 18] on studies of ayahuasca [9,10,11,12,13] and in animals [28,29,30]. The in vitro and in vivo data presented in this paper aim to strengthen the current understanding of DMT pharmacokinetics and metabolism, which can be used to inform future dose selection in healthy adults and patients with MDD.
DMT metabolism is substantially slowed when administered with MAO inhibitors and is a known substrate for MAO-A [14]. One study found DMT preferentially binds to MAO-B [30], and CYP enzymes have been suggested to play a role in DMT metabolism [31] although supporting experimental data have not been published. The in vitro studies reported here demonstrate a role for MAO-A, CYP2D6 and, in part, CYP2C19 in the metabolism of DMT.
Intrinsic clearance was relatively low in whole cell hepatocytes compared to mitochondrial fractions attributed to a greater proportion of MAO enzymes present in mitochondria, demonstrated by the slower clearance rate of MAO substrate controls (benzylamine and serotonin) in hepatocyte vs. mitochondrial fractions (Table 4). DMT clearance rate was not concentration-dependent and surprisingly was not affected by MAO inhibition in hepatocytes (Table 4A). These results suggest that a MAO-independent route of metabolism (e.g., via CYP enzymes) can contribute to DMT breakdown at a slower rate in certain physiological environments. This hypothesis is supported by CYP phenotyping results which demonstrated a role for CYP2D6 and, to a lesser extent, CYP2C19 in the clearance of DMT. Analogously, CYP2D6 and CYP2C19 isoforms were also shown to contribute to the O-demethylation of a similar family of psychoactive N,N-dialkylated tryptamines [32] indicating that CYP enzymes may contribute to the demethylation of DMT and subsequent formation of N-methyltryptamine metabolite. In contrast, in the mitochondrial fractions DMT clearance rate was high and concentration dependent indicating a saturation of metabolism at the 3.1 µM concentration level which was further slowed by MAO-A inhibition, but not MAO-B inhibition (Table 4).
To improve interpretation of pharmacokinetic and metabolism data, specific physiochemical properties were determined for DMT. The preclinical data in this paper confirm that DMT is a lipophobic molecule (logD7.4 = 0.15) which remains largely unbound in human plasma (> 65%, Table 5), indicating a high proportion of drug available for distribution and metabolism, consistent with the very rapid clinical pharmacokinetic and clearance results (Table 10). The high ratio of blood to plasma concentration (1.53, Table 6) indicates that DMT is likely distributed into erythrocytes and therefore should be considered when evaluating blood and plasma pharmacokinetics. Cohort 4 (21.5 mg IV) plasma clearance was 27.9 l/min, which equates to an estimated blood clearance rate of 18.2 l/min when divided by the 1.53 blood:plasma ratio factor. This value far exceeds average liver blood flow (approximately 1.45 l/min, based on a 70-kg man [33]), indicating that IV-administered DMT is largely cleared before reaching the human liver. CYP enzymes are mainly expressed in the liver whereas MAO enzymes are found in many tissues including the lung, brain, heart, gastrointestinal tract and liver [34]. Therefore, while DMT is a substrate for CYP2D6 and CYP2C19 in vitro, these enzymes are unlikely to play a significant role in DMT metabolism following IV administration in humans; however, they may contribute to its poor oral bioavailability [14]. We predict that DMT is primarily metabolised by MAO-A expressed throughout the body.
The general clinical pharmacokinetic profiles obtained from administration of different doses of DMT were similar to those obtained in previous studies [16, 17], demonstrating a very short plasma half-life of 10–12 min. Median Tmax (10–12 min) was notably different from other studies because of the longer IV infusion regimen in this study. Administration of each infusion regimen was well tolerated and there were no safety concerns: only 1 drTEAE was recorded in placebo and cohort 4 groups (Table 8). There was an overall statistical trend of dose-proportional increases in Cmax and AUClast for doses of DMT between 9 mg and 21.5 mg; however, these results should be interpreted with caution given the high level of inter-individual variability in Cmax and AUClast across all dosing cohorts (Table 10). The variability of DMT pharmacokinetics observed in this study is in broad agreement with previously published data. In the study conducted by Strassman and Qualls, reported Cmax for ten subjects ranged from 32 to 204 ng/ml following an IV bolus of 0.4 mg/kg DMT [16]. It is possible that the variability may be explained, at least in part, by the rapid clearance rate causing small deviations in pharmacokinetic sampling time points to contribute to concentration differences. The most notable variability in DMT concentrations was around Tmax, which could be explained by first-order reaction principles, i.e., clearance rate is proportional to drug concentration.
A number of post-hoc analyses explored potential sources of pharmacokinetic variability; however, no significant predictors were detected. Weight-based dosing is commonly used in pharmacological research as body weight and BMI have been shown to influence drug distribution and metabolism [35, 36]. Based on this, many studies using DMT and other psychedelics have applied a weight-adjusted approach to dosing with the aim of reducing subjective psychedelic response variability [15, 16, 19, 37,38,39]. However, fixed dosing of DMT, particularly when given as an IV infusion, is preferable in terms of practicality and clinical feasibility. Within this study, BMI and weight were not shown to be predictive of peak DMT exposure, measured via dose-normalised Cmax and C5min parameters, demonstrating the appropriateness of fixed infusion doses of DMT. These findings support previous analyses showing no association between the subjective effects of psilocybin and weight or BMI [40,41,42].
The preclinical and clinical data reviewed thus far suggest that, following IV administration, DMT is rapidly distributed and is primarily metabolised by MAO-A in the circulatory system and/or brain. To further explore the metabolism of DMT, additional exploratory analyses were performed to estimate potential differences in DMT metabolism through determination of IAA concentrations in a total of eight subjects from cohort 2 (12 mg) and cohort 4 (21.5 mg). Plasma IAA concentrations were substantially larger than DMT; a similar result has recently been reported following IV bolus dosing [18, 43]. This counterintuitive finding may be explained by DMT’s rapid clearance rate and/or larger volume of distribution, relative to IAA. The high baseline and oscillating IAA concentrations within the first 7 min of pharmacokinetic sampling obscure interpretation relative to DMT breakdown. Nevertheless, by 13 min IAA levels were doubled compared to baseline for all eight analysed subjects, confirming the rapid degradation of DMT in plasma. IAA to DMT Cmax ratio appeared to be higher in cohort 2 (12 mg) compared to cohort 4 (21.5 mg), which supports a theory of potential saturation of metabolism, consistent with in vitro mitochondrial fraction data described above. However, dose-normalised Cmax and AUClast of DMT did not increase with dose (calculated from Table 10) and, when excluding cohort 3 (17 mg) results, were relatively consistent across cohorts 1 (9 mg), 2 (12 mg) and 4 (21.5 mg), which contradicts results expected from a system with saturated metabolism. Additionally, baseline IAA concentration and DMT Cmax did not correlate with maximum IAA concentration in cohort 2 or cohort 4 upon visual inspection of data (data not shown) indicating that the rate of oxidative deamination may contribute to, but is unlikely to account for, the variability in DMT pharmacokinetics. However, small sample sizes, high variability and lack of appropriate IAA AUC calculations mean that these interpretations should be treated with caution. To provide a more reliable analysis of the DMT-IAA relationship, future clinical studies should monitor the pharmacokinetic profile of IAA metabolite over a longer duration and in a larger population size to determine the complete pharmacokinetic profile of IAA. In addition, efforts should be made to validate a more sensitive bioanalytical method for IAA detection prior to future studies.
There were several other limitations in the clinical study that may impact the results presented here. First, missing samples from cohort 1 and 3 prevented the calculation of pharmacokinetic parameters for all subjects in these cohorts. While the sample sizes were determined in accordance with a standard phase 1 study, a larger sample size would be beneficial to better understand the variability of DMT pharmacokinetics. Population models investigating the pharmacokinetic-pharmacodynamic effects of DMT have been developed, [18] however, have not performed covariate analysis to shed light on the driving factors leading to the rapid clearance, distribution and variability in the pharmacokinetic profile of DMT. The development of such population models would be of interest to investigate the potential within subject variability in pharmacokinetic and pharmacodynamic effects of DMT.
5 Conclusion
This is the first study to our knowledge to determine the full pharmacokinetic profile and parameters of DMT in humans following administration via a slow IV infusion over 10 min, confirming the rapid attainment of peak plasma levels of DMT and its subsequent clearance via MAO-A. Additionally, these are the first published findings that identify specific human CYP isozymes (2D6 and 2C19) that can contribute to the metabolism of DMT in active MAO-A sparce environments. These findings contribute to the development of improved pharmacokinetic and metabolic models of DMT and to the design of IV infusion regimens for the treatment of mental health disorders.
References
Carhart-Harris RL, Bolstridge M, Day CMJ, Rucker J, Watts R, Erritzoe DE, et al. Psilocybin with psychological support for treatment-resistant depression: six-month follow-up. Psychopharmacology. 2018;235(2):399–408.
Carhart-Harris RGB, Watts R, Baker-Jones M, Murphy-Beiner A, Murphy R, Martell J, Blemings A, Erritzoe D, Nutt DJ. Trial of psilocybin versus escitalopram for depression. N Engl J Med. 2021;384:1402–11.
Sanches RF, de Lima OF, Dos Santos RG, Macedo LR, Maia-de-Oliveira JP, Wichert-Ana L, et al. antidepressant effects of a single dose of ayahuasca in patients with recurrent depression: a SPECT study. J Clin Psychopharmacol. 2016;36(1):77–81.
Palhano-Fontes F, Barreto D, Onias H, Andrade KC, Novaes MM, Pessoa JA, et al. Rapid antidepressant effects of the psychedelic ayahuasca in treatment-resistant depression: a randomized placebo-controlled trial. Psychol Med. 2019;49(4):655–63.
Carhart-Harris RL, Muthukumaraswamy S, Roseman L, Kaelen M, Droog W, Murphy K, et al. Neural correlates of the LSD experience revealed by multimodal neuroimaging. Proc Natl Acad Sci U S A. 2016;113(17):4853–8.
Luoma JB, Chwyl C, Bathje GJ, Davis AK, Lancelotta R. A Meta-analysis of placebo-controlled trials of psychedelic-assisted therapy. J Psychoactive Drugs. 2020;52(4):289–99.
Ballentine G, Friedman SF, Bzdok D. Trips and neurotransmitters: discovering principled patterns across 6850 hallucinogenic experiences. Sci Adv. 2022;8(11): l6989.
Carbonaro TM, Gatch MB. Neuropharmacology of N, N-dimethyltryptamine. Brain Res Bull. 2016;126(Pt 1):74–88.
Schenberg EE, Alexandre JFM, Filev R, Cravo AM, Sato JR, Muthukumaraswamy SD, et al. Acute biphasic effects of ayahuasca. PLoS ONE. 2015;10(9): e0137202.
Callaway JC, McKenna DJ, Grob CS, Brito GS, Raymon LP, Poland RE, et al. Pharmacokinetics of Hoasca alkaloids in healthy humans. J Ethnopharmacol. 1999;65(3):243–56.
Yritia M, Riba J, Ortuño J, Ramirez A, Castillo A, Alfaro Y, et al. Determination of N,N-dimethyltryptamine and beta-carboline alkaloids in human plasma following oral administration of Ayahuasca. J Chromatogr B Analyt Technol Biomed Life Sci. 2002;779(2):271–81.
Riba J, Valle M, Urbano G, Yritia M, Morte A, Barbanoj MJ. Human pharmacology of ayahuasca: subjective and cardiovascular effects, monoamine metabolite excretion, and pharmacokinetics. J Pharmacol Exp Ther. 2003;306(1):73–83.
Lanaro R, Mello SM, da Cunha KF, Silveira G, Corrêa-Neto NF, Hyslop S, et al. Kinetic profile of N,N-dimethyltryptamine and β-carbolines in saliva and serum after oral administration of ayahuasca in a religious context. Drug Test Anal. 2021;13(3):664–78.
Barker SA. N,N-dimethyltryptamine (DMT), an endogenous hallucinogen: past, present, and future research to determine its role and function. Front Neurosci. 2018;12:536.
Kaplan J, Mandel LR, Stillman R, Walker RW, VandenHeuvel WJ, Gillin JC, et al. Blood and urine levels of N,N-dimethyltryptamine following administration of psychoactive dosages to human subjects. Psychopharmacologia. 1974;38(3):239–45.
Strassman RJ, Qualls CR. Dose-response study of N, N-dimethyltryptamine in humans. I. Neuroendocrine, autonomic, and cardiovascular effects. Arch Gen Psychiatry. 1994;51(2):85–97.
Timmermann C, Roseman L, Schartner M, Milliere R, Williams LTJ, Erritzoe D, et al. Neural correlates of the DMT experience assessed with multivariate EEG. Sci Rep. 2019;9(1):16324.
Eckernäs E, Timmermann C, Carhart-Harris R, Röshammar D, Ashton M. Population pharmacokinetic/pharmacodynamic modeling of the psychedelic experience induced by N,N-dimethyltryptamine—implications for dose considerations. Clin Transl Sci. 2022;2:2.
Strassman RJ. Human psychopharmacology of N,N-dimethyltryptamine. Behav Brain Res. 1996;73(1–2):121–4.
Agency EEM. Guideline on strategies to identify and mitigate risks for first-in-human and early clinical trials with investigational medicinal products. EMEA/CHMP/SWP/28367/07 Revision 1. 2017.
Johnson M, Richards W, Griffiths R. Human hallucinogen research: guidelines for safety. J Psychopharmacol. 2008;22(6):603–20.
ABPI. Guidelines for Phase I clinical trials 2018 edition. 2018.
Timmermann C, Roseman L, Williams L, Erritzoe D, Martial C, Cassol H, et al. DMT models the near-death experience. Front Psychol. 2018;9:1424.
Allen GD. MODFIT: a pharmacokinetics computer program. Biopharm Drug Dispos. 1990;11(6):477–98.
EMEA. Guideline on bioanalytical method validation. EMEA/CHMP/EWP/192217/2009. 21 July 2011;Rev. 1 Corr. 2.
FDA. Bioanalytical Method Validation Guidance for Industry. MAY 2018.
Gough K, Hutchison M, Keene O, Byrom B, Ellis S, Lacey L, et al. Assessment of dose proportionality: report from the statisticians in the pharmaceutical industry/pharmacokinetics UK joint working party. Drug Inf J. 1995;29(3):1039–48.
Barker SA, Beaton JM, Christian ST, Monti JA, Morris PE. Comparison of the brain levels of N,N-dimethyltryptamine and alpha, alpha, beta, beta-tetradeutero-N-N-dimethyltryptamine following intraperitoneal injection. The in vivo kinetic isotope effect. Biochem Pharmacol. 1982;31(15):2513–6.
Barker SA, Littlefield-Chabaud MA, David C. Distribution of the hallucinogens N,N-dimethyltryptamine and 5-methoxy-N,N-dimethyltryptamine in rat brain following intraperitoneal injection: application of a new solid-phase extraction LC-APcI-MS-MS-isotope dilution method. J Chromatogr B Biomed Sci Appl. 2001;751(1):37–47.
Suzuki O, Katsumata Y, Oya M, Chari VM, Vermes B, Wagner H, et al. Inhibition of type A and type B monoamine oxidases by naturally occurring xanthones. Planta Med. 1981;42(1):17–21.
Riba J, McIlhenny EH, Bouso JC, Barker SA. Metabolism and urinary disposition of N,N-dimethyltryptamine after oral and smoked administration: a comparative study. Drug Test Anal. 2015;7(5):401–6.
Caspar AT, Gaab JB, Michely JA, Brandt SD, Meyer MR, Maurer HH. Metabolism of the tryptamine-derived new psychoactive substances 5-MeO-2-Me-DALT, 5-MeO-2-Me-ALCHT, and 5-MeO-2-Me-DIPT and their detectability in urine studied by GC-MS, LC-MS(n), and LC-HR-MS/MS. Drug Test Anal. 2018;10(1):184–95.
Davies B, Morris T. Physiological parameters in laboratory animals and humans. Pharm Res. 1993;10(7):1093–5.
Uhlén M, Fagerberg L, Hallström BM, Lindskog C, Oksvold P, Mardinoglu A, et al. Tissue-based map of the human proteome. Science. 2015;347(6220):1260419.
Derendorf H, Schmidt S, Rowland M. Rowland and Tozer's clinical pharmacokinetics and pharmacodynamics : concepts and applications. Fifth edition. ed. Philadelphia: Wolters Kluwer; 2020.
Pan SD, Zhu LL, Chen M, Xia P, Zhou Q. Weight-based dosing in medication use: what should we know? Patient Prefer Adherence. 2016;10:549–60.
Strassman RJ, Qualls CR, Berg LM. Differential tolerance to biological and subjective effects of four closely spaced doses of N,N-dimethyltryptamine in humans. Biol Psychiatry. 1996;39(9):784–95.
D’Souza DC, Syed SA, Flynn LT, et al. Exploratory study of the dose-related safety, tolerability, and efficacy of dimethyltryptamine (DMT) in healthy volunteers and major depressive disorder. Neuropsychopharmacol. 2022;2:2.
Gouzoulis-Mayfrank E, Heekeren K, Neukirch A, Stoll M, Stock C, Obradovic M, et al. Psychological effects of (S)-ketamine and N, N-dimethyltryptamine (DMT): a double-blind, cross-over study in healthy volunteers. Pharmacopsychiatry. 2005;38(6):301–11.
Garcia-Romeu A, Barrett FS, Carbonaro TM, Johnson MW, Griffiths RR. Optimal dosing for psilocybin pharmacotherapy: considering weight-adjusted and fixed dosing approaches. J Psychopharmacol. 2021;35(4):353–61.
Studerus E, Kometer M, Hasler F, Vollenweider FX. Acute, subacute and long-term subjective effects of psilocybin in healthy humans: a pooled analysis of experimental studies. J Psychopharmacol. 2011;25(11):1434–52.
Spriggs M, Giribaldi B, Lyons T, Rosas F, Kärtner L, Buchborn T, et al. Body mass index (BMI) does not predict responses to psilocybin. J Psychopharmacol. 2022;37:026988112211319.
Eckernäs E, Bendrioua A, Cancellerini C, Timmermann C, Carhart-Harris R, Hoffmann K-J, et al. Development and application of a highly sensitive LC-MS/MS method for simultaneous quantification of N,N-dimethyltryptamine and two of its metabolites in human plasma. J Pharm Biomed Anal. 2022;212: 114642.
McGinnity DFPA, Soars M, Riley RJ. Automated definition of the enzymology of drug oxidation by the major human drug metabolizing cytochrome P450s. Drug Metab Dispos. 2000;28(11):1327–34.
Ohtsuki SSO, Kawakami H, Inoue T, Liehner S, Saito A, Ishiguro N, Kishimoto W, Ludwig-Schwellinger E, Ebner T, Terasaki T. Simultaneous absolute protein quantification of transporters, cytochromes P450, and UDP-glucuronosyltransferases as a novel approach for the characterization of individual human liver: comparison with mRNA levels and activities. Drug Metab Dispos. 2012;40(1):83–92.
Achour BRM, Barber J, Rostami-Hodjegan A. Simultaneous quantification of the abundance of several cytochrome P450 and uridine 5’-diphospho-glucuronosyltransferase enzymes in human liver microsomes using multiplexed targeted proteomics. Drug Metab Dispos. 2014;42(4):500–10.
Acknowledgements
Small Pharma would like to thank all participants involved in the trial as well as investigators and research staff in participating institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M.G., T.B., Z.J., C.R. and E.J. are all currently paid employees of Small Pharma and have owned stock in the company, C.T., D.E., G.A., R.W., C.H., H.T. and A.B., are all paid employees of contracted research and academic organisations or independent consultants engaged by Small Pharma.
Funding
This study was funded by Small Pharma. Editorial support was provided by Michelle Preston and Karen Palmer of Livewire Editorial Communications, which was funded by Small Pharma.
Ethics Approval
The trial proposal and any substantial amendments were reviewed by the UK Medicines and Healthcare products Regulatory Agency (MHRA) and the London—Brent Research Ethics Committee (REC). The trial was not started until a clinical trial authorisation had been obtained from the MHRA, and written approval had been obtained from the REC. The Phase 1 trial was done at HMR in accordance with their standard operating procedures (SOPs); The Medicines for Human Use (Clinical Trials) Regulations 2004 and The Human Medicines Regulations 2012, with current amendments; Good Manufacturing Practice (GMP); the SOPs issued by the Research Ethics Service for RECs in the UK; and Good Clinical Practice (GCP), which has its origins in the Declaration of Helsinki. All data generated during the trial are archived at HMR and will be stored for at least 25 years.
Availability of data and material
The datasets generated during and/or analysed during the current study are filed in EudraCT and are not publicly available (in accordance with the regulations for phase 1 data). Further information is available from the corresponding author on reasonable request.
Code availability
Not applicable.
Consent to participate
All participants gave written consent to participate in this trial. Before giving consent, participants read the information about the trial. They then discussed the trial with the investigator or their delegate and were given the opportunity to ask questions. The trial specific information sheet and the consent form were approved by the REC. Each subject was free to withdraw from the trial at any time, without giving a reason. Consent for coronavirus disease 2019 (COVID-19) testing was taken using a special information and consent form (ICF), which was approved by the Health Research Authority (HRA) Generic Documents Review Committee.
Consent for publication
Not applicable
Authors contributions
EJ, ZJ, TB, CR, DE and CT made substantial contributions to the conception or design of the clinical trial. MG, EJ, GA, ZJ, TB, CR, CH, HT and AB made substantial contributions to analysis and interpretation of clinical trial data. MG, ZJ, EJ, TB, CR, RW and AB made substantial contributions to the design, analysis, and interpretation of preclinical study data. Drafting, revision and approval of the article was led by MG, EJ and CR.
Additional information
The authors confirm that the Principal Investigator was Dr. Malcolm Boyce (HMR, 44 Cumberland Ave, London NW10 7EW) and he had direct clinical responsibility for the study subjects. Dr. David Erritzoe was the Chief Investigator.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Good, M., Joel, Z., Benway, T. et al. Pharmacokinetics of N,N-dimethyltryptamine in Humans. Eur J Drug Metab Pharmacokinet 48, 311–327 (2023). https://doi.org/10.1007/s13318-023-00822-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-023-00822-y