Abstract
Background and Objectives
The most important determinant of long-term graft survival in renal transplantation is adequate immunosuppression. Inadequate immunosuppression may lead to graft loss due to the presence of anti-HLA antibody. The aim of this study was to investigate the effect of variability in tacrolimus blood concentration on anti-HLA antibody development in pediatric recipients of living-donor renal transplants.
Methods
Pediatric recipients of living-donor renal transplants were retrospectively evaluated. Patients with a minimum of two years of follow-up who were administered tacrolimus were included in the study. Patients who had pretransplant anti-HLA antibody were excluded. Variability in tacrolimus blood concentration was assessed using the coefficient of variation (“tacrolimus CV”) method. Tacrolimus CV was calculated separately for the first 6 months post-transplant, between 6 and 12 months post-transplant, and from the end of the first year post-transplant to the last follow-up. We constructed receiver operating characteristic (ROC) curves of the tacrolimus CV for each group to find the best cutoff value.
Results
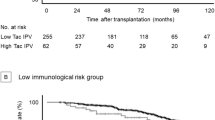
A total of 67 patients (including 48 males; 72%) with a mean age of 15.16 ± 4.43 years were included in the study. Anti-HLA antibody positivity was detected in 12 patients (18%). More than three HLA mismatches and the presence of acute cellular rejection correlated with the development of anti-HLA antibody (p = 0.056, 0.009). Tacrolimus CVs for the three periods were 0.37 ± 0.11, 0.31 ± 0.18, and 0.35 ± 0.12, respectively. The cutoff value of tacrolimus CV for anti-HLA antibody development was calculated as 0.32 with a sensitivity of 90.91% and specificity of 50.94% [AUC (area under the curve) 0.713, p = 0.023]. During the second 6-month period and after a year post-transplant, the percentage of patients with tacrolimus CV > 0.32 was significantly higher in the anti-HLA antibody positive group than in the antibody negative group (67% vs 31%, p = 0.027; 83% vs 47%, p = 0.033). The eGFR (estimated glomerular filtration rate) was similar for the anti-HLA antibody negative and positive groups (78.72 ± 2.86 vs 77.45 ± 8.08, p > 0.05).
Conclusion
High tacrolimus concentration variability appears to be associated with anti-HLA antibody formation in pediatric recipients of living-donor renal transplants.

Similar content being viewed by others
References
Kidney Disease: Improving Global Outcomes Transplant Work Group. KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Transplant. 2009;9(Suppl 3):S1–S155.
Dugast E, Soulillou JP, Foucher Y, Papuchon E, Guerif P, Paul C, et al. Failure of calcineurin inhibitor (tacrolimus) weaning randomized trial in long-term stable kidney transplant recipients. Am J Transplant. 2016;16(11):3255–61.
Staatz CE, Tett SE. Clinical pharmacokinetics and pharmacodynamics of tacrolimus in solid organ transplantation. Clin Pharmacokinet. 2004;43(10):623–53.
Shishido S, Asanuma H, Tajima E, Honda M, Nakai H. Pharmacokinetics of tacrolimus in pediatric renal transplant recipients. Transplant Proc. 2001;33(1–2):1066–8.
Elens L, Capron A, Kerckhove VV, Lerut J, Mourad M, Lison D, et al. 1199G>A and 2677G<T/A polymorphisms of ABCB1 independently affect tacrolimus concentration in hepatic tissue after liver transplantation. Pharmacogenet Genomics. 2007;17(10):873–83.
Wallemacq PE, Verbeeck RK. Comparative clinical pharmacokinetics of tacrolimus in paediatric and adult patients. Clin Pharmacokinet. 2001;40(4):283–95.
Devos JM, Gaber AO, Teeter LD, Graviss EA, Patel SJ, Land GA, et al. Intermediate-term graft loss after renal transplantation is associated with both donor-specific antibody and acute rejection. Transplantation. 2014;15;97(5):534-40.
Sharma A, Lewis JR, Lim WH, Palmer S, Strippoli G, Chapman JR, et al. Renal transplant outcomes and de novo donor-specific anti-human leukocyte antigen antibodies: a systematic review. Nephrol Dial Transplant. 2018;33(8):1472–80.
Girerd S, Schikowski J, Girerd N, Duarte K, Busby H, Gambier N, et al. Impact of reduced exposure to calcineurin inhibitors on the development of de novo DSA: a cohort of non-immunized first kidney graft recipients between 2007 and 2014. BMC Nephrol. 2018;15;19(1):232.
Rodrigo E, Segundo DS, Fernández-Fresnedo G, López-Hoyos M, Benito A, Ruiz JC, et al. Within-patient variability in tacrolimus blood levels predicts kidney graft loss and donor-specific antibody development. Transplantation. 2016;100(11):2479–85.
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, et al. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 200920:629-37.
Tait BD, Süsal C, Gebel HM, Nickerson PW, Zachary AA, Claas FH, et al. Consensus guidelines on the testing and clinical management issues associated with HLA and non-HLA antibodies in transplantation. Transplantation. 2013;95(1):19–47.
Caro-Oleas JL, González-Escribano MF, González-Roncero FM, Acevedo-Calado MJ, Cabello-Chaves V, Gentil-Govantes MÁ, et al. Clinical relevance of HLA donor-specific antibodies detected by single antigen assay in kidney transplantation. Nephrol Dial Transplant. 2012;27(3):1231–8.
Loupy A, Haas M, Solez K, Racusen L, Glotz D, Seron D, et al. The Banff 2015 Kidney Meeting report: current challenges in rejection classification and prospects for adopting molecular pathology. Am J Transplant. 2017;17(1):28–41.
Borra LC, Roodnat JI, Kal JA, Mathot RA, Weimar W, van Gelder T. High within-patient variability in the clearance of tacrolimus is a risk factor for poor long-term outcome after kidney transplantation. Nephrol Dial Transplant. 2010;25(8):2757–63.
Whalen HR, Glen JA, Harkins V, Stevens KK, Jardine AG, Geddes CC, et al. High intrapatient tacrolimus variability is associated with worse outcomes in renal transplantation using a low dose tacrolimus immunosuppressive regime. Transplantation. 2017;101(2):430–6.
Goodall DL, Willicombe M, McLean AG, Taube D. High Intrapatient variability of tacrolimus levels and outpatient clinic nonattendance are associated with inferior outcomes in renal transplant patients. Transplantation Direct. 2017;3:e192. https://doi.org/10.1097/TXD.0000000000000710.
Pollock-BarZiv SM, Finkelstein Y, Manlhiot C, Dipchand AI, Hebert D, Ng VL, Solomon M, et al. Variability in tacrolimus blood levels increases the risk of late rejection and graft loss after solid organ transplantation in older children. Pediatr Transplant. 2010;14:968–75.
Prytula AA, Bouts AH, Mathot RAA, van Gelder T, Croes LK, Hop W, et al. Intra-patient variability in tacrolimus trough concentrations and renal function decline in pediatric renal transplant recipients. Pediatr Transplant. 2012;16:613–8.
Sablik KA, Clahsen-van Groningen MC, Hesselink DA, van Gelder T, Betjes MGH. Tacrolimus intra-patient variability is not associated with chronic active antibody mediated rejection. PLoS One. 2018;13(5):e0196552.
Dobbels F, Ruppar T, De Geest S, Decorte A, Van Damme-Lombaerts R, Fine RN. Adherence to the immunosuppressive regimen in pediatric kidney transplant recipients: a systematic review. Pediatr Transplant. 2010;14:603–13.
Watson AR. Non-compliance and transfer from paediatric to adult transplant units. Pediatr Nephrol. 2000;14:469–72.
Shuker N, van Gelder T, Hesselink DA. Intra-patient variability in tacrolimus exposure: causes, consequences for clinical management. Transplant Rev (Orlando). 2015;29(2):78–84.
Liu C, Shang YF, Zhang XF, Zhang XG, Wang B, Wu Z, et al. Co-administration of grapefruit juice increases bioavailability of tacrolimus in liver transplant patients: a prospective study. Eur J Clin Pharmacol. 2009;65(9):881–5.
Christians U, Jacobsen W, Benet LZ, Lampen A. Mechanisms of clinically relevant drug interactions associated with tacrolimus. Clin Pharmacokinet. 2002;41(11):813–51.
Ginevri F, Nocera A, Comoli P, Innocente A, Cioni M, Parodi A, et al. Posttransplant de novo donor-specific HLA antibodies identify pediatric kidney recipients at risk for late antibody-mediated rejection. Am J Transplant. 2012;12(12):3355–62.
Kim JJ, Balasubramanian R, Michaelides G, Wittenhagen P, Sebire NJ, Mamode N, et al. The clinical spectrum of de novo donor-specific antibodies in pediatric renal transplant recipients. Am J Transplant. 2014;14(10):2350–8.
Azarfar A, Ravanshad Y, Mehrad-Majd H, Esmaeeli M, Aval SB, Emadzadeh M, et al. Comparison of tacrolimus and cyclosporine for immunosuppression after renal transplantation: an updated systematic review and meta-analysis. Saudi J Kidney Dis Transpl. 2018;29(6):1376–85.
Chemouny JM, Suberbielle C, Rabant M, Zuber J, Alyanakian MA, Lebreton X, et al. De novo donor-specific human leukocyte antigen antibodies in nonsensitized kidney transplant recipients after T cell-mediated rejection. Transplantation. 2015;99(5):965–72.
DeVos JM, Gaber AO, Knight RJ, Land GA, Suki WN, Gaber LW, et al. Donor-specific HLA-DQ antibodies may contribute to poor graft outcome after renal transplantation. Kidney Int. 2012;82(5):598–604.
Loupy A, Suberbielle-Boissel C, Hill GS, Lefaucheur C, Anglicheau D, Zuber J, et al. Outcome of subclinical antibody-mediated rejection in kidney transplant recipients with preformed donor-specific antibodies. Am J Transplant. 2009;9(11):2561–70.
Wiebe C, Gibson IW, Blydt-Hansen TD, Karpinski M, Ho J, Storsley LJ, et al. Evolution and clinical pathologic correlations of de novo donor-specific HLA antibody post kidney transplant. Am J Transplant. 2012;12(5):1157–67.
Rozen-Zvi B, Schneider S, Lichtenberg S, Green H, Cohen O, Gafter U, et al. Association of the combination of time-weighted variability of tacrolimus blood level and exposure to low drug levels with graft survival after kidney transplantation. Nephrol Dial Transplant. 2017;32(2):393–99.
Sikma MA, Hunault CC, van de Graaf EA, Verhaar MC, Kesecioglu J, de Lange DW, et al. High tacrolimus blood concentrations early after lung transplantation and the risk of kidney injury. Eur J Clin Pharmacol. 2017;73(5):573–80.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No source of funding was used to conduct this study.
Conflict of interest
Gulsah Kaya Aksoy, Elif Comak, Mustafa Koyun, Halide Akbas, Bahar Akkaya, Bulent Aydınlı, Fahri Ucar, and Sema Akman declare that they have no conflict of interest.
Ethical approval
This study was approved by the review boards and ethics committees of the Akdeniz University Medical Faculty.
Informed consent
Informed consent was obtained from patients, parents, or care givers.
Rights and permissions
About this article
Cite this article
Kaya Aksoy, G., Comak, E., Koyun, M. et al. Tacrolimus Variability: A Cause of Donor-Specific Anti-HLA Antibody Formation in Children. Eur J Drug Metab Pharmacokinet 44, 539–548 (2019). https://doi.org/10.1007/s13318-019-00544-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-019-00544-0