Abstract
Background and objective
P-glycoprotein (P-gp), a transmembrane transporter expressed at the blood–brain barrier, restricts the distribution of diverse central nervous system-targeted drugs from blood into brain, reducing their therapeutic efficacy. The third-generation P-gp inhibitor tariquidar (XR9576) was shown to enhance brain distribution of P-gp substrate drugs in humans. Oral bioavailability of tariquidar was found to be low in humans requiring the compound to be administered intravenously, which hinders a broader clinical use. The objective of the present study was to investigate the plasma pharmacokinetics of tariquidar in rats after single intravenous, oral, and intraperitoneal administration.
Methods
Two different tariquidar formulations (A and B) were used, both at a dosage of 15 mg/kg, respectively. Formulation A was a solution and formulation B was a microemulsion which was previously shown to improve the oral bioavailability of the structurally related P-gp inhibitor elacridar in mice.
Results
In contrast to human data, the present study found a high bioavailability of tariquidar in rats after oral dosing. Oral bioavailability was significantly higher (p = 0.032) for formulation B (86.3%) than for formulation A (71.6%). After intraperitoneal dosing bioavailability was 91.4% for formulation A and 99.6% for formulation B.
Conclusion
The present findings extend the available information on tariquidar and provide a basis for future studies involving oral administration of this compound.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This study investigated the pharmacokinetics of tariquidar in rats after oral, intraperitoneal and intravenous administration. Out of two tariquidar formulations used, a microemulsion showed significantly higher oral bioavailability in rats and might be considered for further testing. |
Availability of a tariquidar formulation with good oral bioavailability in humans would allow for a broader use of the drug in clinical research as a booster of brain delivery of P-gp substrate drugs. |
1 Introduction
P-glycoprotein (P-gp or ABCB1) is a transmembrane transport protein belonging to the adenosine triphosphate (ATP)-binding cassette (ABC) superfamily, which protects different tissues against potentially toxic xenobiotics [1,2,3]. It is expressed in cell membranes of various mammalian organ systems including the kidney, liver, intestine, in the luminal side of brain capillary endothelial cells forming the blood–brain barrier (BBB) and in peripheral blood mononuclear cells like lymphocytes and macrophages [1,2,3]. Accordingly, it has a major impact on the bioavailability, tissue distribution, and excretion of drugs.
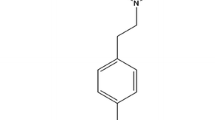
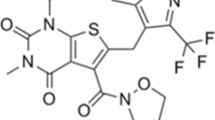
Tariquidar (XR9576) is a non-marketed third-generation P-gp inhibitor [4]. Tariquidar’s potential to overcome P-gp-mediated multidrug resistance (MDR) of tumors has been investigated in human phase I/II clinical studies [5,6,7,8]. However, further clinical development of tariquidar as an MDR reversal agent has been halted due to lack of efficacy and side effects in combination with cytotoxic anticancer drugs. More recently, promising data have been obtained with tariquidar in clinical studies in healthy volunteers with respect to its ability to inhibit P-gp at the BBB and to facilitate brain delivery of P-gp substrate drugs [9, 10]. In addition, since P-gp-related transporters in prokaryotic cells have been shown to mediate resistance to antibiotic drugs, tariquidar has also been investigated as a means to reverse bacterial MDR [11,12,13]. Radiolabeled tariquidar has been used to visualize the function of P-gp and breast cancer-resistance protein (BCRP or ABCG2), another ABC transporter, at the rodent and human BBB [14,15,16,17].
In short, despite the fact that tariquidar has never reached marketing authorization, it still attracts a great deal of scientific interest. To date, although a considerable amount of research on and involving tariquidar has been conducted in laboratory animals, most notably rodents, only limited information is available on the pharmacokinetics of the compound in these species.
The main route of excretion of tariquidar is biliary excretion and direct secretion across the gastrointestinal tract mucosa, with urinary excretion constituting only a minor route [18, 19]. From a clinical study involving intravenous administration of ascending doses of tariquidar up to 8 mg/kg body weight to human healthy volunteers, a long elimination half-life, and a large volume of distribution emerged as the drug’s key pharmacokinetic features [20]. There is some evidence that tariquidar displays non-linear pharmacokinetics, which may be related to saturation of transport proteins mediating excretion and/or tissue distribution of tariquidar at higher doses [15, 20].
Preliminary data on oral dosing of tariquidar in human healthy volunteers have been reported, suggesting a low oral bioavailability of the compound [10, 21]. Aim of the present study was to investigate the pharmacokinetic profile of tariquidar in rats after intravenous, oral, and intraperitoneal administration and to test a previously described microemulsion formulation [22] with respect to its ability to enhance the bioavailability of tariquidar. Exhaustive information on oral pharmacokinetics in rodents could be relevant for future studies involving oral administration to humans as well.
2 Materials and Methods
2.1 Tariquidar Formulations
Two different formulations of tariquidar were tested. Formulation A was obtained by dissolving tariquidar dimesylate (Haoyuan Chemexpress Co., Ltd, Shanghai, PRC) in DMSO and adding heated 5% glucose solution (w/v) to a final DMSO concentration ≤ 2% (v/v). Formulation B was a microemulsion prepared on the basis of a formulation proposed by Sane et al. [22] which was reported to improve oral bioavailability of the structurally related P-gp/BCRP inhibitor elacridar. In brief, the surfactant Kolliphor® EL (Cremophor EL, Sigma-Aldrich, Austria) and the co-surfactant Carbitol™ (diethylene glycol monoethyl ether, Sigma-Aldrich, Austria) were mixed in a 2:1 ratio. After 10 min of heating at 37 °C, the obtained solution was mixed with the medium-chain triglyceride Captex 355 (glyceryl tricaprylate/tricaprate, Abitec, USA) in a 10:1 ratio. Then, tariquidar dimesylate was dissolved in the latter mixture at a concentration of 22.5 mg/mL. This solution was diluted in a 1:3 ratio with deionized water to obtain the desired final tariquidar concentration. Visual inspection of formulation B suggested the formation of a microemulsion, which was not further characterized as this has already been done in detail by Sane et al. [22]. The final concentration of Cremophor EL in formulation B was 0.21 g/mL (w/v).
Both formulations were prepared to give final tariquidar concentrations of 7.5 mg/mL. Aliquots of both tariquidar formulations were snap frozen and stored for a maximum duration of 1 week at − 80 °C immediately after preparation. On the day of scheduled tariquidar administration, the necessary amount of aliquots was thawed and administered after reaching room temperature. Visual appearance of both formulations after thawing was similar to freshly prepared formulations without the presence of precipitates.
2.2 Animals and Study Design
Adult male (10–12 weeks of age and 0.31–0.48 kg of weight, respectively) Sprague–Dawley rats (n = 25, Charles River, Sulzfeld, Germany) were used. The study protocol was approved by the local Animal Welfare Committee. Experiments were performed at the Institute of Biomedical Research, Medical University of Vienna, in full respect of all applicable institutional, national and international guidelines for the conduct of animal research.
Animals were housed at 22 °C protected from noise and vibration in 12-h day/night cycles and were provided with food and water ad libitum. After 14 days of acclimatization, rats were divided into four groups (n = 5) and treated orally or intraperitoneally with both formulations, respectively. In addition, a fifth group of five animals received one intravenous single dose (formulation A only).
Tariquidar was administered at an individually adapted dosage of 15 mg/kg body weight via gastric gavage, intraperitoneal injection or intravenous bolus injection via the tail vein. Total administered volume did not exceed 0.95, 0.76, and 0.9 mL for intravenous, oral, and intraperitoneal administration, respectively. After each tariquidar administration, sublingual blood draws (blood loss at each timepoint = approximately 120 µL) for quantification of tariquidar in plasma were performed at 0.5, 1, 2, 4, 8, and 24-h post-dose in all animals. Blood samples were placed on ice immediately after collection and soon thereafter stored at − 80 °C until analysis. Intravenous administration of tariquidar and venipuncture for blood sampling was performed under short-duration isoflurane anaesthesia.
2.3 Bioanalysis, Pharmacokinetic, and Statistical Analysis
The concentrations of tariquidar in rat plasma were measured with high-performance liquid chromatography–mass spectrometry (LC–MS/MS) using a Dionex “UltiMate 3000” system (Dionex Corp., Sunnyvale, CA, USA) connected with an API 4000 triple-quadrupole mass spectrometer (Applied Biosystems, Concord, Ontario, Canada) according to the literature [23]. Briefly, after the addition of 200 µL of methanol to 100 µL of plasma, the samples were centrifuged (5000×g for 5 min at 4 °C) and 80 µL of the clear supernatant was injected onto the HPLC column. Separation of tariquidar was carried out at 35 °C using a Hypersil BDS-C18 column (5 µm, 250 × 4.6 mm I.D., Thermo Fisher Scientific, Inc, Waltham, MA, USA), preceded by a Hypersil BDS-C18 precolumn (5 µm, 10 × 4.6 mm I.D.). The mobile phase consisted of a continuous linear gradient, mixed from 10 mM ammonium acetate/acetic acid buffer, pH 5.0 (mobile phase A) and methanol (mobile phase B). Linear calibration curves were generated by spiking drug-free rat plasma with standard solutions of tariquidar (final concentrations ranging from 0.005 µg to 10 µg/mL; average correlation coefficient: > 0.999). For this method, the lower limit of detection for tariquidar in plasma was 3 ng/mL and the lower limit of quantification 5 ng/mL. The upper limit of quantification was 5 µg/mL. Coefficients of accuracy and precision for this compound were < 11%.
Pharmacokinetic parameters were calculated by means of standard noncompartmental analysis using a commercially available computer program (Kinetica 3.0, Innaphase Corp., Philadelphia, PA, USA). Maximum plasma concentration (Cmax), time to maximum plasma concentration (Tmax), and area under the concentration–time curve from 0 to last measured concentration (AUC0–24) were calculated from non-fitted data. For AUC calculation, the trapezoidal rule was employed. For accurate description of the pharmacokinetic profile of drugs with long half-lives, the US Food and Drug Administration recommends a sampling period covering 3–5 half-lives of the investigated drug [24]. For practical reasons, sampling in the present study was restricted to 24 h post-dose (i.e., approximately one half-life of tariquidar). Therefore, pharmacokinetic parameters reported here are limited to Cmax, Tmax and AUC0–24.
Absolute bioavailability of orally and intraperitoneally administered tariquidar formulations (formulations A and B) was calculated as ratio of the AUC0–24 of the respective formulation/route to the tariquidar AUC0–24 after intravenous administration of formulation A. Statistical analysis was performed using a commercially available program (IBM SPSS Statistics 22; IBM Corp., Armonk, NY, USA). Independent samples Mann–Whitney U test was used to compare key pharmacokinetic parameters between groups. A two-sided p value of 0.05 was considered as threshold for statistical significance. All values are shown as mean ± standard deviation unless otherwise stated.
3 Results
The median (range) weight of the animals immediately prior to dosing was 0.35 (0.31–0.38) kg, 0.36 (0.31–0.45) kg, and 0.43 (0.36–0.48) kg for the oral, intraperitoneal, and intravenous route, respectively. Tariquidar was well tolerated by all animals. No immediate drug- or procedure-related complications occurred during intravenous, oral, or intraperitoneal administration of the study drug. Concentration–time curves of both tariquidar formulations in plasma of rats for the three administration routes are shown in Fig. 1.
Concentration–time profiles (mean ± standard deviation) of two tariquidar formulations (A = solution, closed symbols vs. B = microemulsion, open symbols) in plasma of male Sprague–Dawley rats after intravenous (a), oral (b) and intraperitoneal (c) single doses of 15 mg/kg, respectively. For comparison, panel d shows all routes of administration plotted in one single graph
Thirty minutes after intravenous injection, tariquidar plasma concentration was 1.91 ± 0.29 µg/mL (Fig. 1a).
After oral administration, drug concentrations in plasma reached their maximum at 4 h after dosing for both formulations (Fig. 1b). Overall, tariquidar plasma concentrations were higher for formulation B (the microemulsion). The difference in AUC0–24 between the two formulations was statistically significant, reflecting a marked increase in bioavailability elicited by the microemulsion (Table 1).
After intraperitoneal injection, peak plasma concentrations were reached more rapidly than after oral administration (Tmax = 2 h for both formulations). Plasma concentrations were numerically higher than after oral dosing, but then showed an elimination pattern very much comparable to intravenous and oral administration (Fig. 1c). Again, albeit to a minor extent compared to oral dosing, formulation B showed slightly increased exposure compared to formulation A. Pooling both formulations within each route, Cmax and AUC0–24 mean values after intraperitoneal dosing reached approximately 80 and 97% of values after intravenous dosing, respectively. Overall oral bioavailability of tariquidar was slightly poorer, with mean Cmax and AUC0–24 values following oral dosing (irrespective of formulation) amounting to approximately 65 and 79% of values after intravenous exposure, respectively. However, with the exception of AUC0–24 after oral dosing, none of the differences between the two formulations were statistically significant. Key pharmacokinetic parameters of tariquidar determined in the present study are summarized in Table 1.
4 Discussion
Over the past years, several P-gp inhibitors, which were originally developed as MDR reversal agents, have been characterized with respect to their ability to inhibit P-gp at the BBB. Among the few compounds tested so far in humans, tariquidar was shown to achieve up to fivefold increases in brain distribution of the model P-gp substrates (R)-[11C]verapamil and [11C]N-desmethyl-loperamide as measured with positron emission tomography (PET) imaging [9, 10]. Such an increase in brain distribution of P-gp substrates can be expected to lead to significant improvements in efficacy of CNS-targeted drugs. However, in these previous studies, tariquidar was administered to humans as a continuous intravenous infusion [9, 10]. For a widespread applicability of tariquidar as a booster of brain distribution of drugs, an oral administration mode would be clearly preferred. One study failed to reveal an effect of orally administered tariquidar on brain distribution of [11C]N-desmethyl-loperamide, which has been attributed to the low oral bioavailability of tariquidar in humans (approximately 12%) [10]. Similarly, while intravenous administration of the structurally related P-gp/BCRP inhibitor elacridar was found to lead to significant P-gp/BCRP inhibition at the non-human primate BBB resulting in a 3.5-fold increase in brain distribution of the dual P-gp/BCRP substrate [11C]erlotinib [25], oral dosing of elacridar in humans failed to increase brain uptake of [11C]erlotinib [26]. Approaches to increase the oral bioavailability of elacridar have been investigated [22, 27] and have shown promising results in rodents. In the present study, we characterized the pharmacokinetic profile of tariquidar in plasma of rats after intravenous, oral and intraperitoneal administration and tested a microemulsion formulation, which has been previously applied to enhance the oral bioavailability of elacridar in rodents [22].
Following administration of tariquidar to human healthy volunteers, a second increase of tariquidar plasma concentrations was observed after reaching the initial Cmax. This second peak was ascribed to the enterohepatic circulation of tariquidar [20]. Interestingly, no such phenomenon was observed in any of the concentration–time profiles in the present study in rats, which might point to species-related differences in metabolism and excretion routes. Among other factors, the impact of enterohepatic circulation of a drug on its plasma concentration depends on rate and extent of breakdown of glucuronidated or otherwise conjugated compound by intestinal microbiota [28]. Substantial compositional diversity of the gut microbiota has been reported previously [29]. After all three administration routes, plasma concentrations of tariquidar remained for 24 h above its previously determined in vivo half-maximum effect concentration (EC50) to increase brain uptake of (R)-[11C]verapamil in rats (545 ± 30 ng/mL) [30]. This suggests that substantial inhibition of P-gp will occur at the BBB and most likely in other P-gp expressing organs of rats (e.g., liver and kidneys). Interestingly, the previous studies found species differences in P-gp inhibition at the human BBB as compared with the rodent BBB with an approximately threefold higher in vivo EC50 value determined for tariquidar in humans (EC50 = 1454 ng/mL) [9]. This suggests that higher tariquidar plasma concentrations are required in humans as compared with rats to overcome P-gp-mediated efflux transport at the BBB.
A noteworthy observation made in our study was the good oral bioavailability of tariquidar in rats achieved with both tested formulations (72–87%), which was substantially higher than previously reported in humans (12%) [10]. Absorption of tariquidar from the intestinal lumen may be restricted by efflux transporters expressed in intestinal epithelial cells, i.e., P-gp and BCRP, for which tariquidar was found to be a substrate [15, 17, 31]. However, tariquidar is a potent inhibitor of P-gp and is also reported to inhibit BCRP [31]. The in vitro EC50 of tariquidar for inhibition of its own transport by human BCRP was approximately 20-fold higher than the EC50 for inhibition of its own transport by human P-gp (EC50: 201 ng/mL for BCRP vs. 11 ng/mL for P-gp) [15]. Values for total intestinal fluid volume reported in the literature range from approximately 100 to 750 mL in adult humans and from approximately 3 to 8 mL in average-weight rats [32,33,34,35]. Accordingly, intestinal concentrations of tariquidar in humans after a 1500 mg oral dose assuming the maximal intestinal fluid volume reported in the literature would be in the range of 2000 ng/mL. Using a median oral dose of 5.3 mg and adjusting volumes from the literature to a median body weight of 0.35 kg, resulting intestinal concentrations of tariquidar in orally dosed rats in the present study would at best reach values of 1000 ng/mL, i.e., half of those in humans. Both values are several folds above the reported in vitro EC50 values of tariquidar for inhibition of its own transport by human P-gp and BCRP, which suggests that intestinal transport by P-gp and BCRP most likely did not contribute to the low oral bioavailability of tariquidar observed in humans. If efflux transport is not involved, then species-related differences in intestinal or hepatic first-pass metabolism might play a role. Tariquidar is extensively metabolized in the liver and its metabolites are excreted into bile [18]. In rats and cynomolgus monkeys, phase I metabolism followed three major pathways: O-demethylation, N-dealkylation, and dehydrogenation. In addition, phase II metabolism occurred via O-glucuronidation. The majority of drug-related material recovered from faeces in rats and monkeys after intravenous administration of [14C]tariquidar was in the form of metabolites [18]. The proportion of parent compound to metabolites in faeces was lower in the monkey than in the rat, indicating that tariquidar was more extensively metabolized in the monkey [18]. In contrast, in plasma, most (> 95%) of the tariquidar-related material existed as the unchanged parent compound [18]. This indicates that tariquidar metabolites, whether formed in the liver or in the intestine, do not distribute into blood. In addition, in humans, no tariquidar metabolites were found in plasma after intravenous administration of the compound [14, 20]. However, no information is currently available regarding the proportion of metabolites relative to parent compound excreted in humans into faeces. If intestinal or hepatic first-pass metabolism of tariquidar occurs in both rats and humans, species differences in metabolism may explain differences in oral bioavailabilities between rats and humans.
Discrepancies in the bioavailability of drugs between rats and humans have been described before [36]. Of all processes that determine systemic concentrations of a drug, those governing intestinal absorptions seem to correlate reasonably well between the two species [36]. Given the drug’s lipophilic character, the ability of tariquidar to penetrate into enterocytes may be similar between rats and humans. However, when administered orally, lipophilic drugs often face the problem of poor water solubility. The latter is determined by various factors including most notably pH and composition of gastrointestinal fluids. While we are not aware of essential differences in physicochemical properties of intestinal fluid between rats and humans, it can be assumed that feeding status at the time of dosing might have an impact on oral bioavailability. Interestingly, the presence of bile salts, which is typically increased in the post-prandial phase [37], is known to enhance the solubilisation and oral absorption of hydrophobic compounds [38]. The animals in the present study had no restrictions regarding intake of food and water during the study, whereas the two studies reporting oral administration of tariquidar in humans do not specify feeding status of the subjects at the time of dosing [10, 21]. Assuming that they were fasted, which seems more likely, one could hypothesize that a poor bile salt content of the intestinal fluid might have determined the poor bioavailability observed in humans opposed to ad libitum-fed rats. Of equal relevance, the impact of the tariquidar formulation should not be ignored. In both studies reporting oral dosing of tariquidar in humans, tariquidar was administered in the form of capsules containing the free base [10, 21], whereas in our study, the dimesylate salt was administered as a solution or microemulsion, which might have facilitated intestinal absorption of the drug.
In the present study, we tested a tariquidar microemulsion for oral and intraperitoneal administration, which has been previously developed and extensively characterized by Sane et al. [22]. The oral bioavailability of elacridar in FVB mice after microemulsion dosing was reported as 47% [22], which was approximately twofold higher as compared with administration of an oral suspension. In addition, the microemulsion formulation was found to retain the P-gp/Bcrp inhibitory effect of elacridar at the mouse BBB. In our study, the standard formulation already had an oral bioavailability of 71.6% and the microemulsion led to a statistically significant improvement in oral bioavailability to 86.9%. This may indicate that tariquidar has a better solubility and permeability across the intestinal mucosa than elacridar. Despite the small sample size of the animal collectives used in the present study, the good tolerability and at least partially significant evidence pointing to a higher bioavailability might justify consideration of the microemulsion as a promising formulation for further rodent studies involving oral and intraperitoneal administration of tariquidar. Moreover, the reported microemulsion may form the basis for the future development of a tariquidar formulation with good oral bioavailability for human use, which could greatly facilitate the utility of tariquidar as a booster of brain distribution of CNS-targeted P-gp substrate drugs.
5 Conclusion
In conclusion, the present project has for the first time described pharmacokinetic profiles of tariquidar in rat plasma after intravenous, oral, and intraperitoneal administration. The good oral bioavailability of tariquidar shown in rats stands in contrast to very low systemic concentrations reported after oral dosing in humans, which constitutes an obstacle to a broader use of the compound as a booster of brain delivery of drugs which are excluded from the brain by P-gp. Possible reasons for this discrepancy have been discussed here, but remain to be fully elucidated. This study has confirmed that the interplay of sometimes conflicting pharmacokinetic subprocesses makes prediction of oral bioavailability of a drug in humans based on rat data challenging. Out of two formulations tested for oral and intraperitoneal dosing, the microemulsion showed improved bioavailability and might be considered for further investigations. The present findings extend the available information on tariquidar and provide a basis for future studies involving oral administration of this compound.
References
Fromm MF. Importance of P-glycoprotein for drug disposition in humans. Eur J Clin Invest. 2003;33(Suppl 2):6–9.
Cascorbi I. Role of pharmacogenetics of ATP-binding cassette transporters in the pharmacokinetics of drugs. Pharmacol Ther. 2006;112(2):457–73.
Leslie EM, Deeley RG, Cole SP. Multidrug resistance proteins: role of P-glycoprotein, MRP1, MRP2, and BCRP (ABCG2) in tissue defense. Toxicol Appl Pharmacol. 2005;204(3):216–37.
Fox E, Bates SE. Tariquidar (XR9576): a P-glycoprotein drug efflux pump inhibitor. Expert Rev Anticancer Ther. 2007;7(4):447–59.
Fox E, Widemann BC, Pastakia D, Chen CC, Yang SX, Cole D, et al. Pharmacokinetic and pharmacodynamic study of tariquidar (XR9576), a P-glycoprotein inhibitor, in combination with doxorubicin, vinorelbine, or docetaxel in children and adolescents with refractory solid tumors. Cancer Chemother Pharmacol. 2015;76(6):1273–83.
Kelly RJ, Draper D, Chen CC, Robey RW, Figg WD, Piekarz RL, et al. A pharmacodynamic study of docetaxel in combination with the P-glycoprotein antagonist tariquidar (XR9576) in patients with lung, ovarian, and cervical cancer. Clin Cancer Res. 2011;17(3):569–80.
Abraham J, Edgerly M, Wilson R, Chen C, Rutt A, Bakke S, et al. A phase I study of the P-glycoprotein antagonist tariquidar in combination with vinorelbine. Clin Cancer Res. 2009;15(10):3574–82.
Pusztai L, Wagner P, Ibrahim N, Rivera E, Theriault R, Booser D, et al. Phase II study of tariquidar, a selective P-glycoprotein inhibitor, in patients with chemotherapy-resistant, advanced breast carcinoma. Cancer. 2005;104(4):682–91.
Bauer M, Karch R, Zeitlinger M, Philippe C, Romermann K, Stanek J, et al. Approaching complete inhibition of P-glycoprotein at the human blood-brain barrier: an (R)-[11C]verapamil PET study. J Cer Blood Flow Metabol. 2015;35(5):743–6.
Kreisl WC, Bhatia R, Morse CL, Woock AE, Zoghbi SS, Shetty HU, et al. Increased permeability-glycoprotein inhibition at the human blood-brain barrier can be safely achieved by performing PET during peak plasma concentrations of tariquidar. J Nucl Med. 2015;56(1):82–7.
Van Bambeke F, Glupczynski Y, Plesiat P, Pechere JC, Tulkens PM. Antibiotic efflux pumps in prokaryotic cells: occurrence, impact on resistance and strategies for the future of antimicrobial therapy. J Antimicrob Chemother. 2003;51(5):1055–65.
Poole K. Efflux-mediated antimicrobial resistance. J Antimicrob Chemother. 2005;56(1):20–51.
Leitner I, Nemeth J, Feurstein T, Abrahim A, Matzneller P, Lagler H, et al. The third-generation P-glycoprotein inhibitor tariquidar may overcome bacterial multidrug resistance by increasing intracellular drug concentration. J Antimicrob Chemother. 2011;66(4):834–9.
Bauer M, Karch R, Zeitlinger M, Stanek J, Philippe C, Wadsak W, et al. Interaction of 11C-tariquidar and 11C-elacridar with P-glycoprotein and breast cancer resistance protein at the human blood-brain barrier. J Nucl Med. 2013;54(8):1181–7.
Bauer M, Romermann K, Karch R, Wulkersdorfer B, Stanek J, Philippe C, et al. Pilot PET study to assess the functional interplay between ABCB1 and ABCG2 at the human blood-brain barrier. Clin Pharmacol Ther. 2016;100(2):131–41.
Wanek T, Kuntner C, Bankstahl JP, Mairinger S, Bankstahl M, Stanek J, et al. A novel PET protocol for visualization of breast cancer resistance protein function at the blood-brain barrier. J Cer Blood Flow Metabol. 2012;32(11):2002–11.
Bankstahl JP, Bankstahl M, Romermann K, Wanek T, Stanek J, Windhorst AD, et al. Tariquidar and elacridar are dose-dependently transported by P-glycoprotein and Bcrp at the blood-brain barrier: a small-animal positron emission tomography and in vitro study. Drug Metab Dispos. 2013;41(4):754–62.
AzaTrius Pharmaceuticals Pvt Ltd M, India. Tariquidar (XR9675, AZT-011) Investigator’s Brochure. 2013.
Bauer M, Blaickner M, Philippe C, Wadsak W, Hacker M, Zeitlinger M, et al. Whole-body distribution and radiation dosimetry of 11C-elacridar and 11C-tariquidar in humans. J Nucl Med. 2016;57(8):1265–8.
Bauer M, Zeitlinger M, Todorut D, Bohmdorfer M, Muller M, Langer O, et al. Pharmacokinetics of single ascending doses of the P-glycoprotein inhibitor tariquidar in healthy subjects. Pharmacology. 2013;91(1–2):12–9.
Stewart A, Steiner J, Mellows G, Laguda B, Norris D, Bevan P. Phase I trial of XR9576 in healthy volunteers demonstrates modulation of P-glycoprotein in CD56 + lymphocytes after oral and intravenous administration. Clin Cancer Res. 2000;6(11):4186–91.
Sane R, Mittapalli RK, Elmquist WF. Development and evaluation of a novel microemulsion formulation of elacridar to improve its bioavailability. J Pharm Sci. 2013;102(4):1343–54.
Bauer M, Zeitlinger M, Karch R, Matzneller P, Stanek J, Jager W, et al. Pgp-mediated interaction between (R)-[11C]verapamil and tariquidar at the human blood-brain barrier: a comparison with rat data. Clin Pharmacol Ther. 2012;91(2):227–33.
U.S. Food and Drug Administration. Bioavailability and Bioequivalence Requirements; Abbreviated Applications; Final Rule. Federal Register Vol. 67, No. 244 2002.
Tournier N, Goutal S, Auvity S, Traxl A, Mairinger S, Wanek T, et al. Strategies to inhibit ABCB1- and ABCG2-mediated efflux transport of erlotinib at the blood-brain barrier: a PET study on nonhuman primates. J Nucl Med. 2017;58(1):117–22.
Verheijen RB, Yaqub MM, Sawicki E, van Tellingen O, Lammertsma AA, Nuijen B, et al. Molecular imaging of ABCB1/ABCG2 inhibition at the human blood brain barrier using elacridar and (11)C-Erlotinib PET. J Nucl Med. 2017. https://doi.org/10.2967/jnumed.117.195800.
Sawicki E, Verheijen RB, Huitema AD, van Tellingen O, Schellens JH, Nuijen B, et al. Clinical pharmacokinetics of an amorphous solid dispersion tablet of elacridar. Drug Del Transl Res. 2017;7(1):125–31.
Noh K, Kang YR, Nepal MR, Shakya R, Kang MJ, Kang W, et al. Impact of gut microbiota on drug metabolism: an update for safe and effective use of drugs. Arch Pharm Res. 2017;40(12):1345–55.
Wang M, Ahrne S, Jeppsson B, Molin G. Comparison of bacterial diversity along the human intestinal tract by direct cloning and sequencing of 16S rRNA genes. FEMS Microbiol Ecol. 2005;54(2):219–31.
Kuntner C, Bankstahl JP, Bankstahl M, Stanek J, Wanek T, Stundner G, et al. Dose-response assessment of tariquidar and elacridar and regional quantification of P-glycoprotein inhibition at the rat blood-brain barrier using (R)-[(11)C]verapamil PET. Eur J Nucl Med Mol Imaging. 2010;37(5):942–53.
Kannan P, Telu S, Shukla S, Ambudkar SV, Pike VW, Halldin C, et al. The “specific” P-glycoprotein inhibitor Tariquidar is also a substrate and an inhibitor for breast cancer resistance protein (BCRP/ABCG2). ACS Chem Neurosci. 2011;2(2):82–9.
Schiller C, Frohlich CP, Giessmann T, Siegmund W, Monnikes H, Hosten N, et al. Intestinal fluid volumes and transit of dosage forms as assessed by magnetic resonance imaging. Aliment Pharmacol Ther. 2005;22(10):971–9.
McConnell EL, Basit AW, Murdan S. Measurements of rat and mouse gastrointestinal pH, fluid and lymphoid tissue, and implications for in vivo experiments. J Pharm Pharmacol. 2008;60(1):63–70.
Mudie DM, Murray K, Hoad CL, Pritchard SE, Garnett MC, Amidon GL, et al. Quantification of gastrointestinal liquid volumes and distribution following a 240 mL dose of water in the fasted state. Mol Pharm. 2014;11(9):3039–47.
Zhang L, Zhang YD, Strong JM, Reynolds KS, Huang SM. A regulatory viewpoint on transporter-based drug interactions. Xenobiotica. 2008;38(7–8):709–24.
Cao X, Gibbs ST, Fang L, Miller HA, Landowski CP, Shin HC, et al. Why is it challenging to predict intestinal drug absorption and oral bioavailability in human using rat model. Pharm Res. 2006;23(8):1675–86.
Porter CJ, Trevaskis NL, Charman WN. Lipids and lipid-based formulations: optimizing the oral delivery of lipophilic drugs. Nat Rev Drug Discov. 2007;6(3):231–48.
Zhang Z, Gao F, Jiang S, Chen L, Liu Z, Yu H, et al. Bile salts enhance the intestinal absorption of lipophilic drug loaded lipid nanocarriers: mechanism and effect in rats. Int J Pharm. 2013;452(1–2):374–81.
Data Availability Statement
The data sets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Acknowledgements
Open access funding provided by Medical University of Vienna. We kindly thank Rajender Mittapalli (University of Minnesota, Minneapolis, MN, USA) for sharing information on the microemulsion used to improve bioavailability of elacridar. Divya Maheshwari (AzaTrius Pharmaceuticals Pvt Ltd, India) is acknowledged for providing the investigator’s brochure of tariquidar.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the Department of Clinical Pharmacology at the Medical University of Vienna, Vienna, Austria.
Conflicts of interest
Disclosure of potential conflicts of interest: PM, MK, SE, AMS, WJ, MB, OL, MZ, and WP declare that they have no conflicts of interest.
Ethics approval
The study protocol was approved by the local Animal Welfare Committee. All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Additional information
Wolfgang Poeppl and Markus Zeitlinger are shared senior authors of this manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Matzneller, P., Kussmann, M., Eberl, S. et al. Pharmacokinetics of the P-gp Inhibitor Tariquidar in Rats After Intravenous, Oral, and Intraperitoneal Administration. Eur J Drug Metab Pharmacokinet 43, 599–606 (2018). https://doi.org/10.1007/s13318-018-0474-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-018-0474-x