Abstract
Objectives
We investigated the correlation of transient elastography (TE) with MRI R2* values and serum ferritin in patients with transfusion-dependent thalassemia (TDT)
Methods
We reviewed hospital records of 59 patients with TDT aged ≥8 years without any evidence of chronic liver disease and who had fibroscan within 3 months of MRI T2*, who seen at our center between January, 2014 and December, 2019. Spearman correlation and linear regression analysis were used to evaluate the correlation between TE liver stiffness measurements and R2* MRI values and with serum ferritin.
Results
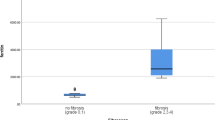
Mean (SD) age of the subjects was 13.0 (3.1) years and body mass index was 16.6 (2.3) kg/m2. Mean liver stiffness measurement, MRI T2*(3T), corresponding MRI R2*(3T), and ferritin values were 6.55 (3.10) kPa, 3.4 (4.6) milliseconds, 616.20 (383.9) Hz, and 2874.69 (1570.7) ng/mL, respectively. TE measurements correlated with MRI R2* values (r=0.61; P=0.001) and with serum ferritin level (r=0.59, P=0.001).
Conclusion
TE is a reliable tool to estimate hepatic iron overload in patients with TDT.
Similar content being viewed by others
References
Shander A, Sazama K. Clinical consequences of iron over-load from chronic red blood cell transfusions, its diagnosis, and its management by chelation therapy. Transfusion. 2010;50:1144–55.
Angelucci E, Brittenham GM, McLaren CE, et al. Hepatic iron concentration and total body iron stores in thalassemia major. N Engl J Med. 2000;343:327–31.
Bedossa P, Dargere D, Paradise V. Sampling variability of liver ûbrosis in chronic hepatitis C. Hepatology. 2003; 38: 1449–57.
Puliyel M, Sposto R, Berdoukas VA, et al. Ferritin trends do not predict changes in total body iron in patients with transfusional iron overload. Am J Hematol. 2014;89:391–4.
St. Pierre TG, El-Beshlawy A, Elalfy M, et al. Multicenter validation of spin-density projection-assisted R2-MRI for the noninvasive measurement of liver iron concentration: multi-center validation of R2-MRI for LIC measurement. Magn Reson Med. 2014;71:2215–23.
Papakonstantinou O, Kostaridou S, Maris T, et al. Quantification of liver iron overload by T2 quantitative magnetic resonance imaging in thalassemia: Impact of chronic hepatitis C on measurements. J Pediatr Hematol Oncol. 1999;21:142–8.
Pipaliya N, Solanke D, Parikh P, et al. Comparison of tissue elastography with magnetic resonance imaging T2* and serum ferritin quantification in detecting liver iron overload in patients with thalassemia major. Clin Gastroenterol Hepatol. 2017;15:292–98.
Fraquelli M, Cassinerio E, Roghi A, et al. Transient elastography in the assessment of liver fibrosis in adult thalassemia patients. Am J Hematol. 2010;85:564–8.
Sandrin L, Fourquet B, Hasquenoph JM, et al. Transient elastography: a new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med Biol. 2003;29:1705–13.
Garbowski MW, Carpenter JP, Smith G, et al. Biopsy-based calibration of T2* magnetic resonance for estimation of liver iron concentration and comparison with R2 ferriscan. J Cardiovasc Magn Reson. 2014;16:40.
Alavian SM, Sadeghian E. Association of fibro scan results with liver biopsy and sonography in major thalassemia patients with hepatitis C. International Journal Advances in Biotechnology Research. 2016;7:532–7.
Sinakos E, Perifanis V, Vlachaki E, et al. Is liver stiffness really unrelated to liver iron concentration? Br J Haematol. 2010;150:247–48.
Elalfy MS, Esmat G, Matter RM, et al. Liver fibrosis in young Egyptian beta-thalassemia major patients: relation to hepatitis C virus and compliance with chelation. Ann Hepatol. 2013;12:54–61.
Mirault T, Lucidarme D, Turlin B et al. Non-invasive assessment of liver ûbrosis by transient elastography in post transfusional iron overload. Eur J Haematol. 2008; 80:337–40.
Atmakusuma TD, Lubis AM. Correlation of serum ferritin and liver iron concentration with transient liver elasto-graphy in adult thalassemia intermedia patients with blood transfusion. J Blood Med. 2021;12: 235–43.
Ou G, Ko HH, Tiwari P, et al. Utility of transient elastography in estimating hepatic iron concentration in comparison to magnetic resonance imaging in patients who are transfusion-dependent: A Canadian center experience. Hemoglobin. 2017;41:21–25.
Funding
None
Author information
Authors and Affiliations
Contributions
Both authors have contributed, designed and approved the study and are accountable for all aspects related to the study.
Corresponding author
Ethics declarations
Institutional Ethics Committee, Kalawati Saran Children’s Hospital; No.LHMC/IEC/2020/57, dated August 19, 2020.
Additional information
Competing interests
None stated.
Rights and permissions
About this article
Cite this article
Parakh, N., Chandra, J. Correlation of Transient Elastography With MRI T2* and Serum Ferritin Levels in Children With Transfusion-Dependent Thalassemia. Indian Pediatr 59, 929–932 (2022). https://doi.org/10.1007/s13312-022-2665-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13312-022-2665-4