Abstract
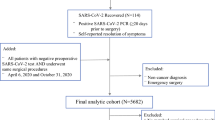
With the emergence of novel variants, Omicron variant caused a different clinical picture than the previous variants and little evidence was reported regarding perioperative outcomes after Omicron variants. The aim of the study was to evaluate the postoperative outcomes of gastrointestinal cancer patients following Omicron variants infection and also to determine the timing of surgery after infection recovery. A total of 124 patients who underwent gastrointestinal cancer surgery with prior SARS-CoV-2 infection between December 2022 and February 2023 were retrospectively reviewed. 174 cases underwent the same operation during December 2018 and February 2019 as control group. SARS-CoV-2-infected patients were further categorized into three groups based on infected time (1–3 weeks; 4–6 weeks; and ≥ 7 weeks). 90.3% of SARS-CoV-2-infected patients had mild symptoms. The COVID-19 vaccination rate was 71.0%, with a full vaccination rate of 48.4%. There were no significant differences in 30-day morbidity and mortality. There was also no significant difference in pulmonary complications, cardiovascular complications, and surgical complications between the three different diagnosis time groups. In conclusion, reducing waiting time for elective surgery was safe for gastrointestinal cancer patients in the context of an increased transmissibility and milder illness severity with Omicron variant.
Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Hu B et al (2021) Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol 19(3):141–154
Baj J et al (2020) COVID-19: specific and non-specific clinical manifestations and symptoms: the current state of knowledge. J Clin Med 9(6):1753
Jonker PKC et al (2021) Perioperative SARS-CoV-2 infections increase mortality, pulmonary complications, and thromboembolic events: a Dutch, multicenter, matched-cohort clinical study. Surgery 169(2):264–274
Kothari AN et al (2021) Surgical outcomes in cancer patients undergoing elective surgery after recovering from mild-to-moderate SARS-CoV-2 infection. Ann Surg Oncol 28(13):8046–8053
Myles PS, Maswime S (2020) Mitigating the risks of surgery during the COVID-19 pandemic. Lancet 396(10243):2–3
Collaborative CO (2021) Effect of COVID-19 pandemic lockdowns on planned cancer surgery for 15 tumour types in 61 countries: an international, prospective, cohort study. Lancet Oncol 22(11):1507–1517
Glasbey JC, Dobbs TD, Abbott TEF (2022) Can patients with asymptomatic SARS-CoV-2 infection safely undergo elective surgery? Br J Anaesth 128(6):909–911
Collaborative CO, GlobalSurg C (2021) Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study. Anaesthesia 76(6):748–758
Hanna TP et al (2020) Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ 371:m4087
Sung H et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
Lievre A et al (2020) Risk factors for Coronavirus Disease 2019 (COVID-19) severity and mortality among solid cancer patients and impact of the disease on anticancer treatment: a French nationwide cohort study (GCO-002 CACOVID-19). Eur J Cancer 141:62–81
Pilz S et al (2022) SARS-CoV-2 reinfections: overview of efficacy and duration of natural and hybrid immunity. Environ Res 209:112911
China’s COVID-19 Response (2023). Available from: https://en.chinacdc.cn/news/latest/202301/W020230126558725888448.pdf. Cited 2023 Aug 4
Gao Z et al (2021) A systematic review of asymptomatic infections with COVID-19. J Microbiol Immunol Infect 54(1):12–16
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
The Lancet R (2021) Too long to wait: the impact of COVID-19 on elective surgery. Lancet Rheumatol 3(2):e83
Lewis D (2023) China’s COVID wave has probably peaked, model suggests. Nature 613(7944):424–425
El-Boghdadly K et al (2023) Timing of elective surgery and risk assessment after SARS-CoV-2 infection: 2023 update: a multidisciplinary consensus statement on behalf of the Association of Anaesthetists, Federation of Surgical Specialty Associations, Royal College of Anaesthetists and Royal College of Surgeons of England. Anaesthesia 78(9):1147–1152
ASA and APSF Joint Statement on Elective Surgery Procedures and Anesthesia for Patients After COVID-19 Infection (2023). Available from: https://www.asahq.org/about-asa/newsroom/news-releases/2023/06/asa-and-apsf-joint-statement-on-elective-surgery-procedures-and-anesthesia-for-patients-after-covid-19-infection. Cited 2023 28 Oct
Sud A et al (2020) Collateral damage: the impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann Oncol 31(8):1065–1074
Wang QX et al (2023) The safety of digestive tract cancer surgery during COVID-19: a living systematic review and meta-analysis. Asian J Surg 46(10):4138–4151
Wang Y et al (2023) Outcomes of liver cancer patients undergoing elective surgery after recovering from mild SARS-CoV-2 omicron infection: a retrospective Cohort Study. Cancers (Basel) 15(17):4254
Menni C et al (2022) Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: a prospective observational study from the ZOE COVID Study. Lancet 399(10335):1618–1624
Yang Q et al (2023) Prolonged viral shedding in cancer patients with asymptomatic or mild omicron infection: a retrospective study. Infect Drug Resist 16:7735–7741
Prevention, C.C.f.D.C.a. COVID-19 Clinical and Surveillance Data—December 9, 2022 to January 23, 2023, China. 2023. Available from: https://en.chinacdc.cn/news/latest/202301/W020230126558725888448.pdf. Cited 2024 19 Jan
Prevention, C.C.f.D.C.a. COVID-19 Clinical and Surveillance Data—December 9, 2022 to April 20, 2023, China. Available from: https://weekly.chinacdc.cn/fileCCDCW/cms/news/info/upload//c6077fe1-dae5-40d2-b7c8-58f419ae8bff.pdf. Cited 2024 20 Jan
Pinato DJ et al (2022) Outcomes of the SARS-CoV-2 omicron (B11529) variant outbreak among vaccinated and unvaccinated patients with cancer in Europe: results from the retrospective, multicentre OnCovid registry study. Lancet Oncol 23(7):865–875
Bui N et al (2021) Preparing previously COVID-19-positive patients for elective surgery: a framework for preoperative evaluation. Perioper Med (Lond) 10(1):1
Funding
This research received no funding.
Author information
Authors and Affiliations
Contributions
D.Z, Y.Y, R,H, X.C, C.M, T.D, B.Y, and D.Y collected data. S.Z. wrote the manuscript draft. X.J. aided in manuscript writing and finalized the manuscript. C.S, S.Z. and X.J. discussed the review content and critically reviewed the manuscript draft. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors have no relevant financial or non-financial interests to disclose.
Informed consent statement
Patient consent was waived for this particular study because this was a retrospective study.
Institutional review board statement
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, D., Yang, Y., Hu, Rh. et al. The impact of SARS-Cov-2 Omicron infection on short-term outcomes after elective surgery in patients with gastrointestinal cancer. Updates Surg (2024). https://doi.org/10.1007/s13304-024-01781-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-024-01781-y