Abstract
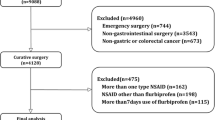
Anastomotic leak (AL) is a feared complication of esophago-gastric surgery. Non-steroidal anti-inflammatory drugs (NSAIDs) are widely used to treat postoperative pain. Previous analyses conveyed heterogeneous data for colorectal surgery with a tendency toward high risk for AL after NSAIDs administration. In the setting of upper gastrointestinal (GI) surgery data are even more puzzled. The purpose of the present study was to assess whether an association exists between postoperative NSAIDs administration and AL after esophago-gastric surgery. PubMed, MEDLINE, Scopus, and Web of Science were searched up to November 2022. The included studies evaluated outcomes for NSAIDs vs. no NSAIDs administration after esophago-gastric surgery. The primary outcome was anastomotic leak (AL). Risk ratio (RR) and 95% confidence intervals (95% CI) were used to assess pooled effect size and relative inference. Six studies (43,784 patients) were included. The patient age ranged from 31 to 84 years, 82.4% were males and preoperative BMI ranged from 15 to 31 kg/m2. Esophagectomy was performed in 95% of patients. NSAIDs were administered in 18,075 (41.3%) patients. The cumulative incidence of AL was similar for NSAIDs vs. no NSAIDs (13.6% vs. 13.4%). The risk for postoperative AL was similar for NSAIDs vs. no NSAIDs administration (RR 1.49; 95% CI 0.81–2.75; p = 0.19). The cumulative incidence of postoperative gastrointestinal bleeding (0.36% vs. 0.39%), acute kidney injury (0.62% vs. 0.71%), and in-hospital mortality (2.39% vs. 2.66%) were comparable. NSAIDs administration for postoperative analgesia seems not associated with an increased risk for AL after esophago-gastric surgery.


Similar content being viewed by others
Data availability
Data generated at a central, large-scale facility, available upon request.
References
Low DE, Kuppusamy MK, Alderson D et al (2019) Benchmarking complications associated with esophagectomy. Ann Surg 269(2):291–298
Aiolfi A, Sozzi A, Bonitta G et al (2022) Linear-versus circular-stapled esophagogastric anastomosis during esophagectomy: systematic review and meta-analysis. Langenbecks Arch Surg 407(8):3297–3309
Kuppusamy MK, Low DE, International Esodata Study Group (IESG) (2022) Evaluation of international contemporary operative outcomes and management trends associated with esophagectomy: a 4-year study of >6000 patients using ECCG definitions and the online esodata database. Ann Surg 275(3):515–525.
Blencowe NS, Strong S, McNair AG, Brookes ST, Crosby T, Griffin SM, Blazeby JM (2012) Reporting of short-term clinical outcomes after esophagectomy: a systematic review. Ann Surg 255(4):658–666
Low DE, Alderson D, Cecconello I et al (2015) International consensus on standardization of data collection for complications associated with esophagectomy: esophagectomy complications consensus group (ECCG). Ann Surg 262(2):286–294
Roh CK, Choi S, Seo WJ et al (2021) Incidence and treatment outcomes of leakage after gastrectomy for gastric cancer: experience of 14,075 patients from a large volume centre. Eur J Surg Oncol 47(9):2304–2312
Trapani R, Rausei S, Reddavid R, Degiuli M; Italian Research Group for Gastric Cancer (GIRCG) Clinical Investigators (2020) Risk factors for esophago-jejunal anastomosis leakage after total gastrectomy for cancer. A multicenter retrospective study of the Italian research group for gastric cancer. Eur J Surg Oncol 46(12):2243–2247
Li H, Zhuang S, Yan H, Wei W, Su Q (2021) Risk factors of anastomotic leakage after esophagectomy with intrathoracic anastomosis. Front Surg 21(8):743266
Grigor EJM, Kaaki S, Fergusson DA, Maziak DE, Seely AJE (2021) Interventions to prevent anastomotic leak after esophageal surgery: a systematic review and meta-analysis. BMC Surg 21(1):42
Wang WJ, Li R, Guo CA et al (2019) Systematic assessment of complications after robotic-assisted total versus distal gastrectomy for advanced gastric cancer: a retrospective propensity score-matched study using Clavien–Dindo classification. Int J Surg 71:140–148
Hakkarainen TW, Steele SR, Bastaworous A et al (2015) Nonsteroidal anti-inflammatory drugs and the risk for anastomotic failure: a report from Washington State’s Surgical Care and Outcomes Assessment Program (SCOAP). JAMA Surg 150(3):223–228. https://doi.org/10.1001/jamasurg.2014.2239. (Erratum in: JAMA Surg. 2015 May;150(5):492)
Wick EC, Grant MC, Wu CL (2017) Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg 152(7):691–697
Ljungqvist O, Scott M, Fearon KC (2017) Enhanced recovery after surgery: a review. JAMA Surg 152:292–298
Low DE, Allum W, De Manzoni G, Ferri L, Immanuel A, Kuppusamy M et al (2019) Guidelines for perioperative care in esophagectomy: enhanced recovery after surgery (ERAS(®)) society recommendations. World J Surg 43:299–330
Rosa F, Longo F, Pozzo C et al (2022) Enhanced recovery after surgery (ERAS) versus standard recovery for gastric cancer patients: the evidences and the issues. Surg Oncol 41:101727
Romario UF, Ascari F, De Pascale S, GIRCG (2022) Implementation of the ERAS program in gastric surgery: a nationwide survey in Italy. Updates Surg 28:1–8
Jamjittrong S, Matsuda A, Matsumoto S et al (2020) Postoperative non-steroidal anti-inflammatory drugs and anastomotic leakage after gastrointestinal anastomoses: systematic review and meta-analysis. Ann Gastroenterol Surg 4:64–75
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 21(339):b2700
Stroup DF, Berlin JA, Morton SC, et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 283(15):2008–2012
Goossen K, Tenckhoff S, Probst P et al (2018) Optimal literature search for systematic reviews in surgery. Langenbecks Arch Surg 403(1):119–129
(2012) Kidney disease improving global outcomes (KDIGO) Clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138
Sterne JA, Hernán MA, Reeves BC, et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919.
Guyatt GH, Oxman AD, Vist GE, et al. GRADE Working Group (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336(7650):924–6.
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Tornese S, Aiolfi A, Bonitta G et al (2019) Remnant gastric cancer after Roux-en-Y gastric bypass: narrative review of the literature. Obes Surg 29(8):2609–2613
Borenstein M, Hedges LV, Higgins JP et al (2010) A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 1(2):97–111
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Davide, Bona Giancarlo, Micheletto Gianluca, Bonitta Valerio, Panizzo Marta, Cavalli Emanuele, Rausa Silvia, Cirri Alberto, Aiolfi (2019) Does C-reactive Protein Have a Predictive Role in the Early Diagnosis of Postoperative Complications After Bariatric Surgery? Systematic Review and Bayesian Meta-analysis Obesity Surgery 29(11) 3448-3456 10.1007/s11695-019-04013-0
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Aiolfi A, Tornese S, Bonitta G, Rausa E, Micheletto G, Bona D. Roux-en-Y gastric bypass: systematic review and Bayesian network meta-analysis comparing open, laparoscopic, and robotic approach. Surg Obes Relat Dis. 2019 Jun;15(6):985-994. doi: 10.1016/j.soard.2019.03.006.
R Development Core Team (2015) A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna (ISBN 3–900051–07–0).
Fjederholt KT, Okholm C, Svendsen LB et al (2018) Ketorolac and other nsaids increase the risk of anastomotic leakage after surgery for GEJ cancers: a cohort study of 557 patients. J Gastrointest Surg 22(4):587–594
Kawakami J, Abe T, Higaki E, Hosoi T, Fukaya M, Komori K, Ito S, Nakatochi M, Nagino M, Shimizu Y (2020) Scheduled intravenous acetaminophen versus nonsteroidal anti-inflammatory drugs (NSAIDs) for better short-term outcomes after esophagectomy for esophageal cancer. Surg Today 50(10):1168–1175
Corsini EM, Hofstetter WL, Anderson Esophageal Cancer Working Group (2021) Ketorolac use and anastomotic leak in patients with esophageal cancer. J Thorac Cardiovasc Surg 161(2):448–454
STARSurg Collaborative (2022) Perioperative nonsteroidal anti-inflammatory drugs (NSAID) administration and acute kidney injury (AKI) in major gastrointestinal surgery: a prospective, multicenter, propensity matched cohort study. Ann Surg 275(5):904–910.
Hirano Y, Konishi T, Kaneko H, Itoh H, Matsuda S, Kawakubo H, Uda K, Matsui H, Fushimi K, Daiko H, Itano O, Yasunaga H, Kitagawa Y (2022) Early postoperative non-steroidal anti-inflammatory drugs and anastomotic leakage after oesophagectomy. Br J Surg:znac399.
Kim SJ, Jeon CH, Lee HH, Song KY, Seo HS (2022) Impact of postoperative NSAIDs (IV-PCA) use on short-term outcomes after laparoscopic gastrectomy for the patients of gastric cancer. Surg Endosc.
Puccetti F, Wijnhoven BPL, Kuppusamy M, Hubka M, Low DE (2022) Impact of standardized clinical pathways on esophagectomy: a systematic review and meta-analysis. Dis Esophagus 35(2):doab027
Jin H, Song S, Lu T, Ma S, Wang Y, Fu L, Zhang G, Han X, Zhang L, Yang K, Cai H (2022) The application of enhanced recovery after surgery in minimally invasive gastrectomy for gastric cancer: a meta-analysis of randomized controlled trials. Expert Rev Gastroenterol Hepatol 16(11–12):1089–1100
Vonkeman HE, van de Laar MA (2010) Nonsteroidal anti-inflammatory drugs: adverse effects and their prevention. Semin Arthritis Rheum 39(4):294–312
Bacchi S, Palumbo P, Sponta A, Coppolino MF (2012) Clinical pharmacology of non-steroidal anti-inflammatory drugs: a review. Antiinflamm Antiall Agents Med Chem 11(1):52–64
Bindu S, Mazumder S, Bandyopadhyay U (2020) Non-steroidal anti-inflammatory drugs (NSAIDs) and organ damage: a current perspective. Biochem Pharmacol 180:114147
Inan A, Koca C, Sen M (2006) Effects of diclofenac sodium on bursting pressures of anastomoses and hydroxyproline contents of perianastomotic tissues in a laboratory study. Int J Surg 4:222–227
Ji C, Xiong Y, Pan X, Guo X, Li Z, Qian S et al (2015) Effect of non-steroidal anti-inflammatory drugs on the increasing the incidence of colonic anastomosis in rats. Int J Clin Exp Pathol 8:6126–6134
Reisinger KW, Schellekens DH, Bosmans JW, Boonen B, Hulsewé KWE, Sastrowijoto P et al (2017) Cyclooxygenase-2 is essential for colorectal anastomotic healing. Ann Surg 265:547–554
Gulcicek OB, Solmaz A, Yigitbas H, Ercetin C, Yavuz E, Ozdogan K et al (2018) Role of diclofenac sodium and paracetamol on colonic anastomosis: an experimental rodent model. Asian J Surg 41:264–269
Kokoska ER, Smith GS, Wolff AB, Deshpande Y, Miller TA (1999) Nonsteroidal anti-inflammatory drugs attenuate epidermal growth factor-induced proliferation independent of prostaglandin synthesis inhibition. J Surg Res 84(2):186–192
Diller R, Stratmann U, Helmschmied T, Bäumer G, Bahde R, Minin E, Spiegel HU (2008) Microcirculatory dysfunction in endotoxemic bowel anastomosis: the pathogenetic contribution of microcirculatory dysfunction to endotoxemia-induced healing impairment. J Surg Res 150(1):3–10
Klein M, Gögenur I, Rosenberg J (2012) Postoperative use of non-steroidal anti-inflammatory drugs in patients with anastomotic leakage requiring reoperation after colorectal resection: cohort study based on prospective data. BMJ 26(345):e6166
Kastora SL, Osborne LL, Jardine R, Kounidas G, Carter B, Myint PK (2021) Non-steroidal anti-inflammatory agents and anastomotic leak rates across colorectal cancer operations and anastomotic sites: a systematic review and meta-analysis of anastomosis specific leak rate and confounding factors. Eur J Surg Oncol 47(11):2841–2848
Modasi A, Pace D, Godwin M, Smith C, Curtis B (2019) NSAID administration post colorectal surgery increases anastomotic leak rate: systematic review/meta-analysis. Surg Endosc 33(3):879–885
Smith SA, Roberts DJ, Lipson ME, Buie WD, MacLean AR (2016) Postoperative nonsteroidal anti-inflammatory drug use and intestinal anastomotic dehiscence: a systematic review and meta-analysis. Dis Colon Rectum 59(11):1087–1097
Burton TP, Mittal A, Soop M (2013) Nonsteroidal anti-inflammatory drugs and anastomotic dehiscence in bowel surgery: systematic review and meta-analysis of randomized, controlled trials. Dis Colon Rectum 56(1):126–134
Arron MNN, Lier EJ, de Wilt JHW, Stommel MWJ, van Goor H, Ten Broek RPG (2020) Postoperative administration of non-steroidal anti-inflammatory drugs in colorectal cancer surgery does not increase anastomotic leak rate—a systematic review and meta-analysis. Eur J Surg Oncol 46(12):2167–2173
Scharf RE (2012) Drugs that affect platelet function. Semin Thromb Hemost 38(8):865–883
Acknowledgements
OGSA Group for Esophagogastric Surgery: Francesca Lombardo, Marta Cavalli, Michele Manara, Juxhin Guraj, Guglielmo Guerrazzi
Funding
None.
Author information
Authors and Affiliations
Consortia
Contributions
AA, MM, JG and GG did the literature search. AA, GB, and DB formed the study design. Data collection done by AA, MM, FL, and MC. AA and GB analyzed the data. AA, GC, and DB interpreted the data. AA wrote the manuscript. All authors critically reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval
For this type of article, ethical approval is not required because does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
For this type of study, formal consent was not necessary.
Research involving human participants and/or animals
Research involved animals and humans. There is no consent required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
OGSA Group for Esophagogastric Surgery members name listed in acknowledgement section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aiolfi, A., Bonitta, G., Campanelli, G. et al. Impact of postoperative NSAIDs administration on anastomotic leak after esophago-gastric surgery: systematic review and meta-analysis. Updates Surg 75, 817–824 (2023). https://doi.org/10.1007/s13304-023-01515-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-023-01515-6